Abstract
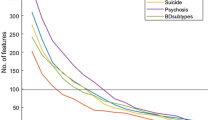
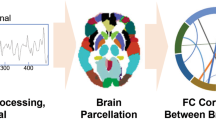
Bipolar disorder (BD) is associated with a high risk of suicidality, and it is challenging to predict suicide attempts in clinical practice to date. Although structural and functional connectivity alterations from neuroimaging studies have been previously reported in BD with suicide attempts, little is known about how abnormal structural and functional connectivity relates to each other. Here, we hypothesize that structure connectivity constrains functional connectivity, and structural–functional coupling is a more sensitive biomarker to detect subtle brain abnormalities than any single modality in BD patients with a current major depressive episode who had attempted suicide. By investigating structural and resting-state fMRI connectivity, as well as their coupling among 191 BD depression patients with or without a history of suicide attempts and 113 healthy controls, we found that suicide attempters in BD depression patients showed significantly decreased central-temporal structural connectivity, increased frontal–temporal functional connectivity, along with decreased structural–functional coupling compared with non-suicide attempters. Crucially, the altered structural connectivity network predicted the abnormal functional connectivity network profile, and the structural–functional coupling was significantly correlated with suicide risk but not with depression or anxiety severity. Our findings suggest that the structural connectome is the key determinant of brain dysfunction, and structural–functional coupling could serve as a valuable trait-like biomarker for BD suicidal predication over and above the intramodality network connectivity. Such a measure can have clinical implications for early identification of suicide attempters with BD depression and inform strategies for prevention.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Plans L, Barrot C, Nieto E, Rios J, Schulze TG, Papiol S, et al. Association between completed suicide and bipolar disorder: a systematic review of the literature. J Affect Disord. 2019;242:111–22.
Pompili M, Gonda X, Serafini G, Innamorati M, Sher L, Amore M, et al. Epidemiology of suicide in bipolar disorders: a systematic review of the literature. Bipolar Disord. 2013;15:457–90.
Novick DM, Swartz HA, Frank E. Suicide attempts in bipolar I and bipolar II disorder: a review and meta-analysis of the evidence. Bipolar Disord. 2010;12:1–9.
Gosnell SN, Fowler JC, Salas R. Classifying suicidal behavior with resting-state functional connectivity and structural neuroimaging. Acta Psychiatr Scand. 2019;140:20–9.
Hagmann P, Cammoun L, Gigandet X, Meuli R, Honey CJ, Wedeen VJ, et al. Mapping the structural core of human cerebral cortex. PLoS Biol. 2008;6:e159.
Geng J, Yan R, Shi J, Chen Y, Mo Z, Shao J, et al. Altered regional homogeneity in patients with somatic depression: a resting-state fMRI study. J Affect Disord. 2019;246:498–505.
Lu Q, Jiang HT, Liu HY, Liu G, Teng GJ, Yao ZJ. Depression severity evaluation for female patients based on a functional mri model. J Magn Reson Imaging. 2010;31:1067–74.
Tian S, Zhang S, Mo Z, Chattun MR, Wang Q, Wang L, et al. Antidepressants normalize brain flexibility associated with multi-dimensional symptoms in major depressive patients. Prog Neuropsychopharmacol Biol Psychiatry. 2020;100:109866.
Ding Y, Pereira F, Hoehne A, Beaulieu MM, Lepage M, Turecki G, et al. Altered brain processing of decision-making in healthy first-degree biological relatives of suicide completers. Mol Psychiatry. 2017;22:1149–54.
Johnston JAY, Wang F, Liu J, Blond BN, Wallace A, Liu J, et al. Multimodal neuroimaging of frontolimbic structure and function associated with suicide attempts in adolescents and young adults with bipolar disorder. Am J Psychiatry. 2017;174:667–75.
Pandey GN, Dwivedi Y, Ren X, Rizavi HS, Mondal AC, Shukla PK, et al. Brain region specific alterations in the protein and mRNA levels of protein kinase A subunits in the post-mortem brain of teenage suicide victims. Neuropsychopharmacology. 2005;30:1548–56.
Lewis CP, Nakonezny PA, Blacker CJ, Vande Voort JL, Port JD, Worrell GA, et al. Cortical inhibitory markers of lifetime suicidal behavior in depressed adolescents. Neuropsychopharmacology. 2018;43:1822–31.
Zhang RB, Shao ROB, Xu GY, Lu WC, Zheng WJ, Miao QZ, et al. Aberrant brain structural-functional connectivity coupling in euthymic bipolar disorder. Hum Brain Mapp. 2019;40:3452–63.
Zhang ZQ, Liao W, Chen HF, Mantini D, Ding JR, Xu Q, et al. Altered functional-structural coupling of large-scale brain networks in idiopathic generalized epilepsy. Brain. 2011;134:2912–28.
Honey CJ, Sporns O, Cammoun L, Gigandet X, Thiran JP, Meuli R, et al. Predicting human resting-state functional connectivity from structural connectivity. Proc Natl Acad Sci USA. 2009;106:2035–40.
Dai Z, Lin Q, Li T, Wang X, Yuan H, Yu X, et al. Disrupted structural and functional brain networks in Alzheimer’s disease. Neurobiol Aging. 2019;75:71–82.
Zhang J, Zhang Y, Wang L, Sang L, Yang J, Yan R, et al. Disrupted structural and functional connectivity networks in ischemic stroke patients. Neuroscience. 2017;364:212–25.
Jiang H, Bahramisharif A, van Gerven MAJ, Jensen O. Distinct directional couplings between slow and fast gamma power to the phase of theta oscillations in the rat hippocampus. Eur J Neurosci. 2020;51:2070–81.
Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59:22–33.
Lish JD, Weissman MM, Adams PB, Hoven CW, Bird H. Family psychiatric screening instruments for epidemiologic studies: pilot testing and validation. Psychiatry Res. 1995;57:169–80.
Monkul ES, Hatch JP, Nicoletti MA, Spence S, Brambilla P, Lacerda AL, et al. Fronto-limbic brain structures in suicidal and non-suicidal female patients with major depressive disorder. Mol Psychiatry. 2007;12:360–6.
World Medical A. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310:2191–4.
Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62.
Hamilton M. The assessment of anxiety states by rating. Br J Med Psychol. 1959;32:50–5.
Cutcliffe JR, Barker P. The Nurses’ Global Assessment of Suicide Risk (NGASR): developing a tool for clinical practice. J Psychiatr Ment Health Nurs. 2004;11:393–400.
Jenkinson M, Beckmann CF, Behrens TE, Woolrich MW, Smith SM. Fsl. NeuroImage. 2012;62:782–90.
Xie S, Chen L, Zuo N, Jiang T. DiffusionKit: A light one-stop solution for diffusion MRI data analysis. J Neurosci Methods. 2016;273:107–19.
Mori S, Crain BJ, Chacko VP, van Zijl PC. Three-dimensional tracking of axonal projections in the brain by magnetic resonance imaging. Ann Neurol. 1999;45:265–9.
Chao-Gan Y, Yu-Feng Z. DPARSF: a MATLAB toolbox for “pipeline” data analysis of resting-state fmri. Front Syst Neurosci. 2010;4:13.
Tzourio-Mazoyer N, Landeau B, Papathanassiou D, Crivello F, Etard O, Delcroix N, et al. Automated anatomical labeling of activations in SPM using a macroscopic anatomical parcellation of the MNI MRI single-subject brain. NeuroImage. 2002;15:273–89.
Zalesky A, Fornito A, Bullmore ET. Network-based statistic: identifying differences in brain networks. NeuroImage. 2010;53:1197–207.
Chung SJ, Kim HR, Jung JH, Lee PH, Jeong Y, Sohn YH. Identifying the functional brain network of motor reserve in early Parkinson’s disease. Mov Disord. 2020;35:577–86.
Chahal R, Gotlib IH, Guyer AE. Research review: brain network connectivity and the heterogeneity of depression in adolescence—a precision mental health perspective. J Child Psychol Psychiatry. 2020. https://doi.org/10.1111/jcpp.13250.
Perlis RH, Ostacher MJ, Goldberg JF, Miklowitz DJ, Friedman E, Calabrese J, et al. Transition to mania during treatment of bipolar depression. Neuropsychopharmacology. 2010;35:2545–52.
Auerbach RP, Pisoni A, Bondy E, Kumar P, Stewart JG, Yendiki A, et al. Neuroanatomical prediction of anhedonia in adolescents. Neuropsychopharmacology. 2017;42:2087–95.
Brown VM, Wilson J, Hallquist MN, Szanto K, Dombrovski AY. Ventromedial prefrontal value signals and functional connectivity during decision-making in suicidal behavior and impulsivity. Neuropsychopharmacology. 2020;45:1034–41.
Schmaal L, van Harmelen AL, Chatzi V, Lippard ETC, Toenders YJ, Averill LA, et al. Imaging suicidal thoughts and behaviors: a comprehensive review of 2 decades of neuroimaging studies. Mol Psychiatry. 2020;25:408–27.
Tanaka SC, Doya K, Okada G, Ueda K, Okamoto Y, Yamawaki S. Prediction of immediate and future rewards differentially recruits cortico-basal ganglia loops. Nat Neurosci. 2004;7:887–93.
van Heeringen K, Van den Abbeele D, Vervaet M, Soenen L, Audenaert K. The functional neuroanatomy of mental pain in depression. Psychiatry Res. 2010;181:141–4.
Jollant F, Lawrence NS, Giampietro V, Brammer MJ, Fullana MA, Drapier D, et al. Orbitofrontal cortex response to angry faces in men with histories of suicide attempts. Am J Psychiatry. 2008;165:740–8.
van Heeringen K, Mann JJ. The neurobiology of suicide. Lancet Psychiatry. 2014;1:63–72.
Bari A, Robbins TW. Inhibition and impulsivity: behavioral and neural basis of response control. Prog Neurobiol. 2013;108:44–79.
Mann JJ. Neurobiology of suicidal behaviour. Nat Rev Neurosci. 2003;4:819–28.
Pan LA, Hassel S, Segreti AM, Nau SA, Brent DA, Phillips ML. Differential patterns of activity and functional connectivity in emotion processing neural circuitry to angry and happy faces in adolescents with and without suicide attempt. Psychol Med. 2013;43:2129–42.
Reisch T, Seifritz E, Esposito F, Wiest R, Valach L, Michel K. An fMRI study on mental pain and suicidal behavior. J Affect Disord. 2010;126:321–5.
Torres-Platas SG, Hercher C, Davoli MA, Maussion G, Labonte B, Turecki G, et al. Astrocytic hypertrophy in anterior cingulate white matter of depressed suicides. Neuropsychopharmacology. 2011;36:2650–8.
Jung J, Choi S, Han KM, Kim A, Kang W, Paik JW, et al. Alterations in functional brain networks in depressed patients with a suicide attempt history. Neuropsychopharmacology. 2020;45:964–74.
Supekar K, Uddin LQ, Prater K, Amin H, Greicius MD, Menon V. Development of functional and structural connectivity within the default mode network in young children. NeuroImage. 2010;52:290–301.
Hagmann P, Sporns O, Madan N, Cammoun L, Pienaar R, Wedeen VJ, et al. White matter maturation reshapes structural connectivity in the late developing human brain. Proc Natl Acad Sci USA. 2010;107:19067–72.
Gamboa OL, Tagliazucchi E, von Wegner F, Jurcoane A, Wahl M, Laufs H, et al. Working memory performance of early MS patients correlates inversely with modularity increases in resting state functional connectivity networks. NeuroImage. 2014;94:385–95.
Jiang H, Dai Z, Lu Q, Yao Z. Magnetoencephalography resting-state spectral fingerprints distinguish bipolar depression and unipolar depression. Bipolar Disord. 2019;00:1–9. https://doi.org/10.1111/bdi.12871.
Jiang H, Tian S, Bi K, Lu Q, Yao Z. Hyperactive frontolimbic and frontocentral resting-state gamma connectivity in major depressive disorder. J Affect Disord. 2019;257:74–82.
Melozzi F, Bergmann E, Harris JA, Kahn I, Jirsa V, Bernard C. Individual structural features constrain the mouse functional connectome. Proc Natl Acad Sci USA. 2019;116:26961–69.
Shen K, Misic B, Cipollini BN, Bezgin G, Buschkuehl M, Hutchison RM, et al. Stable long-range interhemispheric coordination is supported by direct anatomical projections. Proc Natl Acad Sci USA. 2015;112:6473–8.
Tian S, Chattun MR, Zhang S, Bi K, Tang H, Yan R, et al. Dynamic community structure in major depressive disorder: a resting-state MEG study. Prog Neuropsychopharmacol Biol Psychiatry. 2019;92:39–47.
Lu Q, Jiang H, Luo G, Han Y, Yao Z. Multichannel matching pursuit of MEG signals for discriminative oscillation pattern detection in depression. Int J Psychophysiol. 2013;88:206–12.
Lu Q, Jiang H, Bi K, Liu C, Yao Z. Discriminative analysis with a limited number of MEG trials in depression. J Affect Disord. 2014;167:207–14.
Acknowledgements
We thank all participants and staffs of the Affiliated Brain Hospital of Nanjing Medical University for their contributions to data generation.
Author information
Authors and Affiliations
Contributions
HJ, RZ, ZY, and QL conceived and designed this research. HJ, RZ, ST, HW, ZC, XW, JS, JQ, JS, HL, and YC performed research, HJ, RZ, ST, and HW analyzed data. HJ, RZ, ZY, QL wrote the paper. All authors reviewed the final submission and gave final approval of the submitted version.
Corresponding authors
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Jiang, H., Zhu, R., Tian, S. et al. Structural–functional decoupling predicts suicide attempts in bipolar disorder patients with a current major depressive episode. Neuropsychopharmacol. 45, 1735–1742 (2020). https://doi.org/10.1038/s41386-020-0753-5
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41386-020-0753-5
This article is cited by
-
Structural and functional deficits and couplings in the cortico-striato-thalamo-cerebellar circuitry in social anxiety disorder
Translational Psychiatry (2022)
-
Graph theory analysis of whole brain functional connectivity to assess disturbances associated with suicide attempts in bipolar disorder
Translational Psychiatry (2022)
-
Identification of suicidality in patients with major depressive disorder via dynamic functional network connectivity signatures and machine learning
Translational Psychiatry (2022)
-
Spontaneous transient states of fronto-temporal and default-mode networks altered by suicide attempt in major depressive disorder
European Archives of Psychiatry and Clinical Neuroscience (2022)
-
Temporal dynamics alterations of spontaneous neuronal activity in anterior cingulate cortex predict suicidal risk in bipolar II patients
Brain Imaging and Behavior (2021)