Abstract
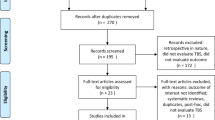
Mixed depression is probably different in terms of clinical course and response to treatment. Repetitive transcranial magnetic stimulation (rTMS) is well established in non-mixed depression, and theta-burst stimulation (TBS) protocol is replacing conventional protocols because of noninferiority and reduced delivery time. However, TBS has not been adequately studied in mixed states. This study was a double-blind, six-week, sham-controlled, and randomized clinical trial of bilateral TBS targeting the right and left dorsolateral prefrontal cortex, respectively. Adults with bipolar and major depressive disorder experiencing an acute mixed depression were eligible if they had not benefited from a first- or second-line treatment for acute unipolar or bipolar depression recommended by the Canadian Network for Mood and Anxiety Treatments. Out of 100 patients included, 90 composed modified intention-to-treat sample, which was patients that completed at least one week of the intervention. There were no significant differences in Montgomery-Asberg depression rating scale score changes (least squares mean difference between groups at week 3, −0.06 [95% CI, − 3.39 to 3.51; P = 0.97] in favor of sham TBS). Response and remission rates per MADRS were also not statistically different among active and sham groups (35.7% vs. 43.7%, and 28.5% vs. 37.5% respectively at week 6, ps > 0.51). No other analyses from baseline to weeks 3 or 6 revealed significant time x group interaction or mean differences among groups in the mITT sample. Bilateral TBS targeting the DLPFC is not efficacious as an add-on treatment of acute bipolar and unipolar mixed depression. ClinicalTrials.govIdentifier: NCT04123301
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Ferrari AJ, Stockings E, Khoo JP, Erskine HE, Degenhardt L, Vos T, et al. The prevalence and burden of bipolar disorder: findings from the Global Burden of Disease Study 2013. Bipolar Disord. 2016;18:440–50.
Ferrari AJ, Charlson FJ, Norman RE, Patten SB, Freedman G, Murray CJ, et al. Burden of depressive disorders by country, sex, age, and year: findings from the global burden of disease study 2010. PLoS med. 2013;10:e1001547.
Verdolini N, Agius M, Ferranti L, Moretti P, Piselli M, Quartesan R. The state of the art of the DSM-5 “with mixed features” specifier. The Scientific World Journal. 2015;2015::757258.
McIntyre R, Tohen M, Berk M, Zhao J, Weiller E. DSM-5 mixed specifier for manic episodes: evaluating the effect of depressive features on severity and treatment outcome using asenapine clinical trial data. J Affect Disord. 2013;150:378–83.
Hergueta T, Weiller E. Evaluating depressive symptoms in hypomanic and manic episodes using a structured diagnostic tool: validation of a new Mini International Neuropsychiatric Interview (MINI) module for the DSM-5’With Mixed Features’ specifier. Int J bipolar Disord. 2013;1:1–10.
Takeshima M, Oka T. DSM‐5‐defined ‘mixed features’ and B enazzi’s mixed depression: which is practically useful to discriminate bipolar disorder from unipolar depression in patients with depression? Psychiatry Clin Neurosci. 2015;69:109–16.
Yatham LN, Kennedy SH, Parikh SV, Schaffer A, Bond DJ, Frey BN, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) and International Society for Bipolar Disorders (ISBD) 2018 guidelines for the management of patients with bipolar disorder. Bipolar Disord. 2018;20:97–170.
McIntyre RS, Soczynska JK, Cha DS, Woldeyohannes HO, Dale RS, Alsuwaidan MT, et al. The prevalence and illness characteristics of DSM-5-defined “mixed feature specifier” in adults with major depressive disorder and bipolar disorder: results from the International Mood Disorders Collaborative Project. J Affect Disord. 2015;172:259–64.
Zimmermann P, Brückl T, Nocon A, Pfister H, Lieb R, Wittchen H-U, et al. Heterogeneity of DSM-IV major depressive disorder as a consequence of subthreshold bipolarity. Arch Gen psychiatry. 2009;66:1341–52.
Goldberg JF, Perlis RH, Bowden CL, Thase ME, Miklowitz DJ, Marangell LB, et al. Manic symptoms during depressive episodes in 1380 patients with bipolar disorder: findings from the STEP-BD. Am J Psychiatry. 2009;166:173–81.
Perugi G, Angst J, Azorin J-M, Bowden CL, Mosolov S, Reis J, et al. Mixed features in patients with a major depressive episode: the BRIDGE-II-MIX study. The. J Clin psychiatry. 2015;76:351–58.
Popovic D, Vieta E, Azorin JM, Angst J, Bowden CL, Mosolov S, et al. Suicide attempts in major depressive episode: evidence from the BRIDGE‐II‐Mix study. Bipolar Disord. 2015;17:795–803.
Tavormina G. Bipolar disorders and bipolarity: the notion of the “mixity”. Psychiatr Danubina. 2019;31:434–7.
Talih F, Gebara NY, Andary FS, Mondello S, Kobeissy F, Ferri R. Delayed sleep phase syndrome and bipolar disorder: pathogenesis and available common biomarkers. Sleep Med Rev. 2018;41:133–40.
Shim IH, Woo YS, Bahk W-M. Prevalence rates and clinical implications of bipolar disorder “with mixed features” as defined by DSM-5. J Affect Disord. 2015;173:120–25.
Verdolini N, Hidalgo‐Mazzei D, Murru A, Pacchiarotti I, Samalin L, Young A, et al. Mixed states in bipolar and major depressive disorders: systematic review and quality appraisal of guidelines. Acta Psychiatr Scandinavica. 2018;138:196–222.
Seo H-J, Wang H-R, Jun T-Y, Woo YS, Bahk W-M. Factors related to suicidal behavior in patients with bipolar disorder: the effect of mixed features on suicidality. Gen hospital psychiatry. 2016;39:91–96.
Berlim M, Van den Eynde F, Tovar-Perdomo S, Daskalakis Z. Response, remission and dropout rates following high-frequency repetitive transcranial magnetic stimulation (rTMS) for treating major depression: a systematic review and meta-analysis of randomized, double-blind and sham-controlled trials. Psychological Med. 2014;44:225.
Teng S, Guo Z, Peng H, Xing G, Chen H, He B, et al. High-frequency repetitive transcranial magnetic stimulation over the left DLPFC for major depression: session-dependent efficacy: a meta-analysis. Eur Psychiatry. 2017;41:75–84.
Brunoni AR, Chaimani A, Moffa AH, Razza LB, Gattaz WF, Daskalakis ZJ, et al. Repetitive transcranial magnetic stimulation for the acute treatment of major depressive episodes: a systematic review with network meta-analysis. JAMA psychiatry. 2017;74:143–52.
Schwippel T, Schroeder PA, Fallgatter AJ, Plewnia C. Clinical review: The therapeutic use of theta-burst stimulation in mental disorders and tinnitus. Prog Neuro-Psychopharmacol Biol Psychiatry. 2019;92:285–300.
Blumberger DM, Vila-Rodriguez F, Thorpe KE, Feffer K, Noda Y, Giacobbe P, et al. Effectiveness of theta burst versus high-frequency repetitive transcranial magnetic stimulation in patients with depression (THREE-D): a randomised non-inferiority trial. Lancet. 2018;391:1683–92.
Cao X, Deng C, Su X, Guo Y. Response and remission rates following high-frequency vs. low-frequency repetitive transcranial magnetic stimulation (rTMS) over right DLPFC for treating major depressive disorder (MDD): a meta-analysis of randomized, double-blind trials. Front psychiatry. 2018;9:413.
Li C-T, Chen M-H, Juan C-H, Liu R-S, Lin W-C, Bai Y-M, et al. Effects of prefrontal theta-burst stimulation on brain function in treatment-resistant depression: a randomized sham-controlled neuroimaging study. Brain stimulation. 2018;11:1054–62.
Fitzgerald PB, Hoy KE, Elliot D, McQueen RS, Wambeek LE, Daskalakis ZJ. Accelerated repetitive transcranial magnetic stimulation in the treatment of depression. Neuropsychopharmacology 2018;43:1565–72.
Lefaucheur J-P, Aleman A, Baeken C, Benninger DH, Brunelin J, Di Lazzaro V, et al. Evidence-based guidelines on the therapeutic use of repetitive transcranial magnetic stimulation (rTMS): an update (2014–2018). Clinical neurophysiology. 2020;131:474-528.
Pallanti S, Grassi G, Antonini S, Quercioli L, Salvadori E, Hollander E. rTMS in resistant mixed states: an exploratory study. J Affect Disord. 2014;157:66–71.
Zeeuws D, De Rycker K, De Raedt R, De Beyne M, Baeken C, Vanderbruggen N. Intensive high-frequency repetitive transcranial magnetic stimulation treatment in an electroconvulsive shock therapy-resistant bipolar I patient with mixed episode. Brain stimulation. 2011;4:46–49.
Praharaj SK, Ram D, Arora M. Efficacy of high frequency (rapid) suprathreshold repetitive transcranial magnetic stimulation of right prefrontal cortex in bipolar mania: a randomized sham controlled study. J Affect Disord. 2009;117:146–50.
Saba G, Rocamora JF, Kalalou K, Benadhira R, Plaze M, Lipski H, et al. Repetitive transcranial magnetic stimulation as an add-on therapy in the treatment of mania: a case series of eight patients. Psychiatry Res. 2004;128:199–202.
Michael N, Erfurth A. Treatment of bipolar mania with right prefrontal rapid transcranial magnetic stimulation. J Affect Disord. 2004;78:253–57.
Williams JR. The Declaration of Helsinki and public health. Bull World Health Organ. 2008;86:650–52.
Del-Ben C, Vilela J, de S, Crippa JA, Hallak JEC, Labate CM, et al. Confiabilidade de” Entrevista Clınica Estruturada para o DSM-IV–Versao Clınica” traduzida para o português./Reliability of the Structured Clinical Interview for DSM-IV—Clinical Version translated into Portuguese. Rev Bras Psiquiatr. 2010;23:156–59.
Hawley C, Gale T, Sivakumaran T, group HNR. Defining remission by cut off score on the MADRS: selecting the optimal value. J Affect Disord. 2002;72:177–84.
Duarte-Guerra LS, Gorenstein C, Paiva-Medeiros PF, Santo MA, Neto FL, Wang Y-P. Clinical utility of the Montgomery-Åsberg Depression Rating Scale for the detection of depression among bariatric surgery candidates. BMC psychiatry. 2016;16:1–8.
Vilela J, Crippa J, Del-Ben C, Loureiro S. Reliability and validity of a Portuguese version of the Young Mania Rating Scale. Braz J Med Biol Res. 2005;38:1429–39.
Swann AC, Lafer B, Perugi G, Frye MA, Bauer M, Bahk W-M, et al. Bipolar mixed states: an international society for bipolar disorders task force report of symptom structure, course of illness, and diagnosis. Am J Psychiatry. 2013;170:31–42.
Tohen M, Kanba S, McIntyre RS, Fujikoshi S, Katagiri H. Efficacy of olanzapine monotherapy in the treatment of bipolar depression with mixed features. J Affect Disord. 2014;164:57–62.
Azorin J-M, Kaladjian A, Adida M, Fakra E, Belzeaux R, Hantouche E, et al. Self-assessment and characteristics of mixed depression in the French national EPIDEP study. J Affect Disord. 2012;143:109–17.
Kennedy SH, Lam RW, McIntyre RS, Tourjman SV, Bhat V, Blier P, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) 2016 clinical guidelines for the management of adults with major depressive disorder: section 3. Pharmacological treatments. Can J Psychiatry. 2016;61:540–60.
Tavares DF, Dos Santos CGR, Valiengo L, Klein I, Borrione L, Forte PM, et al. Efficacy, safety, and tolerability of theta-burst stimulation in mixed depression: design, rationale, and objectives of a randomized, double-blinded, sham-controlled trial. Front psychiatry. 2020;11:435.
Brunoni AR, Sampaio-Junior B, Moffa AH, Aparício LV, Gordon P, Klein I, et al. Noninvasive brain stimulation in psychiatric disorders: a primer. Braz J Psychiatry. 2019;41:70–81.
Li C-T, Chen M-H, Juan C-H, Huang H-H, Chen L-F, Hsieh J-C, et al. Efficacy of prefrontal theta-burst stimulation in refractory depression: a randomized sham-controlled study. Brain 2014;137:2088–98.
Blumberger DM, Vila-Rodriguez F, Thorpe KE, Feffer K, Noda Y, Giacobbe P, et al. Effectiveness of theta burst versus high-frequency repetitive transcranial magnetic stimulation in patients with depression (THREE-D): a randomised non-inferiority trial. Lancet 2018;391:1683–92.
Chistyakov AV, Rubicsek O, Kaplan B, Zaaroor M, Klein E. Safety, tolerability and preliminary evidence for antidepressant efficacy of theta-burst transcranial magnetic stimulation in patients with major depression. Int J Neuropsychopharmacol. 2010;13:387–93.
Nettekoven C, Volz LJ, Kutscha M, Pool EM, Rehme AK, Eickhoff SB, et al. Dose-dependent effects of theta burst rTMS on cortical excitability and resting-state connectivity of the human motor system. J Neurosci. 2014;34:6849–59.
Plewnia C, Pasqualetti P, Große S, Schlipf S, Wasserka B, Zwissler B, et al. Treatment of major depression with bilateral theta burst stimulation: a randomized controlled pilot trial. J Affect Disord. 2014;156:219–23.
Li CT, Cheng CM, Chen MH, Juan CH, Tu PC, Bai YM, et al. Antidepressant efficacy of prolonged intermittent theta burst stimulation monotherapy for recurrent depression and comparison of methods for coil positioning: a randomized, double-blind, sham-controlled study. Biol Psychiatry. 2020;87:443–50.
Li CT, Chen MH, Juan CH, Huang HH, Chen LF, Hsieh JC, et al. Efficacy of prefrontal theta-burst stimulation in refractory depression: a randomized sham-controlled study. Brain 2014;137:2088–98.
Chistyakov AV, Kreinin B, Marmor S, Kaplan B, Khatib A, Darawsheh N, et al. Preliminary assessment of the therapeutic efficacy of continuous theta-burst magnetic stimulation (cTBS) in major depression: a double-blind sham-controlled study. J Affect Disord. 2015;170:225–9.
George MS, Lisanby SH, Avery D, McDonald WM, Durkalski V, Pavlicova M, et al. Daily left prefrontal transcranial magnetic stimulation therapy for major depressive disorder: a sham-controlled randomized trial. Arch Gen Psychiatry. 2010;67:507–16.
Levkovitz Y, Isserles M, Padberg F, Lisanby SH, Bystritsky A, Xia G, et al. Efficacy and safety of deep transcranial magnetic stimulation for major depression: a prospective multicenter randomized controlled trial. World Psychiatry. 2015;14:64–73.
Oberman L, Edwards D, Eldaief M, Pascual-Leone A. Safety of theta burst transcranial magnetic stimulation: a systematic review of the literature. J Clin Neurophysiol. 2011;28:67.
Freire MÁ, Figueiredo VLMD, Gomide A, Jansen K, Silva RAD, Magalhães PVDS, et al. Escala Hamilton: estudo das características psicométricas em uma amostra do sul do Brasil. J Brasileiro de Psiquiatria. 2014;63:281–89.
Guy W. ECDEU Assessment Manual for Psychopharmacology-Revised. Rockville, MD: National Institute of Mental Health. Psychopharmacol Res Branch. 1976:217–22.
Jones SH, Thornicroft G, Coffey M, Dunn G. A brief mental health outcome scale. Br J Psychiatry. 1995;166:654–59.
Fleck M, Louzada S, Xavier M, Chachamovich E, Vieira G, Santos L, et al. Aplicação da versão em português do instrumento abreviado de avaliação da qualidade de vida” WHOQOL-bref”. Rev de saúde pública. 2000;34:178–83.
Malloy-Diniz LF, Mattos P, Leite WB, Abreu N, Coutinho G, Paula JJD, et al. Tradução e adaptação cultural da Barratt Impulsiveness Scale (BIS-11) para aplicação em adultos brasileiros. J Brasileiro de Psiquiatria. 2010;59:99–105.
Bates D, Mächler M, Bolker B, Walker S Fitting linear mixed-effects models using lme4. arXiv preprint arXiv:14065823. 2014.
Buuren SV, Groothuis-Oudshoorn K. mice: Multivariate imputation by chained equations in R. J of statistical software. 2010;45:1–68.
Lenth R, Singmann H, Love J, Buerkner P, Herve M. Emmeans: Estimated marginal means, aka least-squares means. R package version. 2018;1:3.
Team RC (Vienna, Austria: R Foundation for Statistical Computing. Retrieved from, 2017).
Suppes T, Silva R, Cucchiaro J, Mao Y, Targum S, Streicher C, et al. Lurasidone for the Treatment of Major Depressive Disorder With Mixed Features: A Randomized, Double-Blind, Placebo-Controlled Study. Am J Psychiatry. 2016;173:400–7.
Sackeim HA, Greenberg MS, Weiman AL, Gur RC, Hungerbuhler JP, Geschwind N. Hemispheric asymmetry in the expression of positive and negative emotions. Neurologic Evid Arch Neurol. 1982;39:210–8.
Kaladjian A, Belzeaux R, Micoulaud-Franchi JA, Cermolacce M, Fakra E, Azorin JM. [Mixed states and neuroimaging]. Encephale 2013;39:S162–6.
Sani G, Napoletano F, Vöhringer PA, Sullivan M, Simonetti A, Koukopoulos A, et al. Mixed depression: clinical features and predictors of its onset associated with antidepressant use. Psychother Psychosom. 2014;83:213–21.
Fornaro M, Stubbs B, De Berardis D, Perna G, Valchera A, Veronese N, et al. Atypical antipsychotics in the treatment of acute bipolar depression with mixed features: a systematic review and exploratory meta-analysis of placebo-controlled clinical trials. Int J Mol Sci. 2016;17:241.
Pacchiarotti I, Kotzalidis GD, Murru A, Mazzarini L, Rapinesi C, Valentí M, et al. Mixed features in depression: the unmet needs of diagnostic and statistical manual of mental disorders fifth edition. Psychiatr Clin North Am. 2020;43:59–68.
Cuomo A, Nikolova VL, Yalin N, Arnone D, Fagiolini A, Young AH. Pharmacological treatment of mixed states. CNS Spectr. 2017;22:186–95.
Suppes T, Ostacher M. Mixed features in major depressive disorder: diagnoses and treatments. CNS Spectr. 2017;22:155–60.
Grunze H, Vieta E, Goodwin GM, Bowden C, Licht RW, Azorin JM, et al. The World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for the biological treatment of bipolar disorders: acute and long-term treatment of mixed states in bipolar disorder. World J Biol Psychiatry. 2018;19:2–58.
Patel R, Reiss P, Shetty H, Broadbent M, Stewart R, McGuire P, et al. Do antidepressants increase the risk of mania and bipolar disorder in people with depression? A retrospective electronic case register cohort study. BMJ Open. 2015;5:e008341.
Bjørklund L, Horsdal HT, Mors O, Østergaard SD, Gasse C. Trends in the psychopharmacological treatment of bipolar disorder: a nationwide register-based study. Acta Neuropsychiatr. 2016;28:75–84.
Stahl SM, Morrissette DA, Faedda G, Fava M, Goldberg JF, Keck PE, et al. Guidelines for the recognition and management of mixed depression. CNS Spectr. 2017;22:203–19.
Tee MMK, Au CH. A systematic review and meta-analysis of randomized sham-controlled trials of repetitive transcranial magnetic stimulation for bipolar disorder. Psychiatr Q. 2020;91:1225–47.
Benazzi F, Akiskal HS. Delineating bipolar II mixed states in the Ravenna-San Diego collaborative study: the relative prevalence and diagnostic significance of hypomanic features during major depressive episodes. J Affect Disord. 2001;67:115–22.
Akiskal HS, Benazzi F, Perugi G, Rihmer Z. Agitated “unipolar” depression re-conceptualized as a depressive mixed state: implications for the antidepressant-suicide controversy. J Affect Disord. 2005;85:245–58.
Angst J, Azorin JM, Bowden CL, Perugi G, Vieta E, Gamma A, et al. Prevalence and characteristics of undiagnosed bipolar disorders in patients with a major depressive episode: the BRIDGE study. Arch Gen Psychiatry. 2011;68:791–8.
Judd LL, Schettler PJ, Akiskal H, Coryell W, Fawcett J, Fiedorowicz JG, et al. Prevalence and clinical significance of subsyndromal manic symptoms, including irritability and psychomotor agitation, during bipolar major depressive episodes. J Affect Disord. 2012;138:440–8.
Pae CU, Vöhringer PA, Holtzman NS, Thommi SB, Patkar A, Gilmer W, et al. Mixed depression: a study of its phenomenology and relation to treatment response. J Affect Disord. 2012;136:1059–61.
Berlim MT, van den Eynde F, Tovar-Perdomo S, Daskalakis ZJ. Response remission and dropout rates following high-frequency repetitive transcranial magnetic stimulation (rTMS) for treating major depression: a systematic review and meta-analysis of randomized, double-blind and sham-controlled trials. Psychol Med. 2014;44:225–39.
Zhang YQ, Zhu D, Zhou XY, Liu YY, Qin B, Ren GP, et al. Bilateral repetitive transcranial magnetic stimulation for treatment-resistant depression: a systematic review and meta-analysis of randomized controlled trials. Braz J Med Biol Res. 2015;48:198–206.
Mutz J, Vipulananthan V, Carter B, Hurlemann R, Fu CHY, Young AH. Comparative efficacy and acceptability of non-surgical brain stimulation for the acute treatment of major depressive episodes in adults: systematic review and network meta-analysis. Bmj 2019;364:l1079.
Mutz J, Edgcumbe DR, Brunoni AR, Fu CHY. Efficacy and acceptability of non-invasive brain stimulation for the treatment of adult unipolar and bipolar depression: A systematic review and meta-analysis of randomised sham-controlled trials. Neurosci Biobehav Rev. 2018;92:291–303.
McGirr A, Karmani S, Arsappa R, Berlim MT, Thirthalli J, Muralidharan K, et al. Clinical efficacy and safety of repetitive transcranial magnetic stimulation in acute bipolar depression. World Psychiatry. 2016;15:85–6.
Nguyen TD, Hieronymus F, Lorentzen R, McGirr A, Østergaard SD. The efficacy of repetitive transcranial magnetic stimulation (rTMS) for bipolar depression: A systematic review and meta-analysis. J Affect Disord. 2021;279:250–55.
Tavares DF, Myczkowski ML, Alberto RL, Valiengo L, Rios RM, Gordon P, et al. Treatment of bipolar depression with deep TMS: results from a double-blind, randomized, parallel group, sham-controlled clinical trial. Neuropsychopharmacology 2017;42:2593–601.
Bulteau S, Beynel L, Marendaz C, Dall’Igna G, Peré M, Harquel S, et al. Twice-daily neuronavigated intermittent theta burst stimulation for bipolar depression: A Randomized Sham-Controlled Pilot Study. Neurophysiol Clin. 2019;49:371–75.
Rostami R, Kazemi R, Nitsche MA, Gholipour F, Salehinejad MA. Clinical and demographic predictors of response to rTMS treatment in unipolar and bipolar depressive disorders. Clin Neurophysiol. 2017;128:1961–70.
Yang YB, Chan P, Rayani K, McGirr A. Comparative effectiveness of repetitive transcranial magnetic stimulation in unipolar and bipolar depression. Can J Psychiatry. 2021;66:313–15.
McGirr A, Vila-Rodriguez F, Cole J, Torres IJ, Arumugham SS, Keramatian K, et al. Efficacy of active vs sham intermittent theta burst transcranial magnetic stimulation for patients with bipolar depression: a randomized clinical trial. JAMA Netw Open. 2021;4:e210963.
Grisaru N, Chudakov B, Yaroslavsky Y, Belmaker RH. Transcranial magnetic stimulation in mania: a controlled study. Am J Psychiatry. 1998;155:1608–10.
Kaptsan A, Yaroslavsky Y, Applebaum J, Belmaker RH, Grisaru N. Right prefrontal TMS versus sham treatment of mania: a controlled study. Bipolar Disord. 2003;5:36–9.
Michael N, Erfurth A. Treatment of bipolar mania with right prefrontal rapid transcranial magnetic stimulation. J Affect Disord. 2004;78:253–7.
Saba G, Rocamora JF, Kalalou K, Benadhira R, Plaze M, Lipski H, et al. Repetitive transcranial magnetic stimulation as an add-on therapy in the treatment of mania: a case series of eight patients. Psychiatry Res. 2004;128:199–202.
Praharaj SK, Ram D, Arora M. Efficacy of high frequency (rapid) suprathreshold repetitive transcranial magnetic stimulation of right prefrontal cortex in bipolar mania: a randomized sham controlled study. J Affect Disord. 2009;117:146–50.
Pathak V, Sinha VK, Praharaj SK. Efficacy of adjunctive high frequency repetitive transcranial magnetic stimulation of right prefrontal cortex in adolescent mania: a randomized sham-controlled study. Clin Psychopharmacol Neurosci. 2015;13:245–9.
Mir-Moghtadaei A, Caballero R, Fried P, Fox MD, Lee K, Giacobbe P, et al. Concordance between BeamF3 and MRI-neuronavigated target sites for repetitive transcranial magnetic stimulation of the left dorsolateral prefrontal cortex. Brain Stimul. 2015;8:965–73.
Prasser J, Schecklmann M, Poeppl TB, Frank E, Kreuzer PM, Hajak G, et al. Bilateral prefrontal rTMS and theta burst TMS as an add-on treatment for depression: a randomized placebo controlled trial. World J Biol Psychiatry. 2015;16:57–65.
Duprat R, Desmyter S, Rudi de R, van Heeringen K, Van den Abbeele D, Tandt H, et al. Accelerated intermittent theta burst stimulation treatment in medication-resistant major depression: A fast road to remission? J Affect Disord. 2016;200:6–14.
Author information
Authors and Affiliations
Contributions
Conceived and designed the clinical trial: DFT, ARB, RAM. Contributed to the acquisition, analysis, or interpretation of data for the work: DFT, PS, CGRS, DHM, LCLV, IK, LB, PMF, ARB, RAM. Wrote the first draft of the manuscript: DFT. Contributed to the writing of the manuscript: ARB, RAM.
Corresponding author
Ethics declarations
Competing interests
DFT worked as a speaker and produced scientific source during the last two years for the following pharmaceutical companies: Cristália, Aché, Torrent, Abbott, Lundbeck. ARB reports grants from SaoPaulo Research State Foundation (FAPESP, 2017/50223-6, 2018/10861-7, 2019/06009-6), Newton Advanced Fellowship (12/1010), Brazilian National Council of Scientific Development Productivity Support (PQ-1B) and University of Sao Paulo Medical School Productivity Support (PIPA-A). . RAM reports grants from Sao Paulo Research State Foundation (FAPESP) and from the National Research Council (CNPq). Other authors declare no conflicts of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Tavares, D.F., Suen, P., Rodrigues dos Santos, C.G. et al. Treatment of mixed depression with theta-burst stimulation (TBS): results from a double-blind, randomized, sham-controlled clinical trial. Neuropsychopharmacol. 46, 2257–2265 (2021). https://doi.org/10.1038/s41386-021-01080-9
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41386-021-01080-9
This article is cited by
-
The medial prefrontal cortex as a proposed regulatory structure in the relationship between anxiety and perceived social support: a review
BMC Psychology (2025)
-
Theta burst stimulation for depression: a systematic review and network and pairwise meta-analysis
Molecular Psychiatry (2024)
-
Growing placebo response in TMS treatment for depression: a meta-analysis of 27-year randomized sham-controlled trials
Nature Mental Health (2023)