Abstract
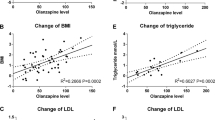
Prescription rates of second-generation antipsychotics (SGAs) are rapidly increasing for non-indicated (i.e., off-label) usage. SGAs used for approved indications are associated with significant metabolic adverse effects, including weight gain. The objective of this systematic review and meta-analysis is to evaluate the metabolic adverse effects of SGA use for off-label management of psychiatric illnesses in the adult population. We performed a systematic database search to identify randomized controlled trials (RCTs) that reported on weight and other metabolic outcomes with off-label use of SGAs among adults. Thirty-eight RCTs met inclusion criteria for this review; 35 of these studies, with a total of 4930 patients, were included in the quantitative meta-analysis. Patients treated with olanzapine, risperidone, and quetiapine were more likely to report weight gain as a side effect and experience clinically significant (≥7%) weight gain compared to those treated with a placebo. Among studies that reported weight as a continuous outcome, olanzapine was associated with significantly greater weight gain across all disorders (mean difference (MD) = 3.24 kg, 95% CI: 2.57–3.90 p = 0.001, N = 12 studies). Similar trends were noted with quetiapine and risperidone. A meta-regression analysis revealed a positive dose-response association between olanzapine dose and weight gain (regression coefficient: 0.36, p = 0.001). This review demonstrates that off-label use of SGAs, and particularly olanzapine, is associated with significant weight gain among adult patients. Our findings are concerning given the widespread off-label use of SGAs. Further studies are required to better understand the effects of off-label SGA use on other metabolic parameters. The study was registered with the PROSPERO international database of prospectively registered systematic reviews (PROSPERO #143186).
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Correll CU, Detraux J, De Lepeleire J, De Hert M. Effects of antipsychotics, antidepressants and mood stabilizers on risk for physical diseases in people with schizophrenia, depression and bipolar disorder. World Psychiatry. 2015;14:119–36.
Rajkumar AP, Horsdal HT, Wimberley T, Cohen D, Mors O, Borglum AD, et al. Endogenous and antipsychotic-related risks for diabetes mellitus in young people with schizophrenia: a danish population-based cohort study. Am J Psychiatry. 2017;174:686–94.
Hennekens CH, Hennekens AR, Hollar D, Casey DE. Schizophrenia and increased risks of cardiovascular disease. Am Heart J. 2005;150:1115–21.
Musil R, Obermeier M, Russ P, Hamerle M. Weight gain and antipsychotics: a drug safety review. Expert Opin Drug Saf. 2015;14:73–96.
Galling B, Roldán A, Nielsen RE, Nielsen J, Gerhard T, Carbon M, et al. Type 2 diabetes mellitus in youth exposed to antipsychotics: a systematic review and meta-analysis. JAMA Psychiatry. 2016;73:247–59.
Wharton S, Lau DCW, Vallis M, Sharma AM, Biertho L, Campbell-Scherer D, et al. Obesity in adults: a clinical practice guideline. Can Med Assoc J. 2020;192:E875–E91.
Canadian Academy of Child and Adolescent Psychiatry, Canadian Academy of Geriatric Psychiatry, Canadian Psychiatric Association. Thirteen Things Physicians and Patients Should Question. Choosing Wisely Canada. https://choosingwiselycanada.org/psychiatry/. Published 2020. Accessed August 23, 2021.
Pringsheim T, Gardner DM. Dispensed prescriptions for quetiapine and other second-generation antipsychotics in Canada from 2005 to 2012: a descriptive study. CMAJ Open. 2014;2:E225–32.
Kalverdijk LJ, Bachmann CJ, Aagaard L, Burcu M, Glaeske G, Hoffmann F, et al. A multi-national comparison of antipsychotic drug use in children and adolescents, 2005-2012. Child Adolesc Psychiatry Ment Health. 2017;11:55.
Alexander GC, Gallagher SA, Mascola A, Moloney RM, Stafford RS. Increasing off-label use of antipsychotic medications in the United States, 1995-2008. Pharmacoepidemiol Drug Saf. 2011;20:177–84.
De Hert M, Detraux J, van Winkel R, Yu W, Correll CU. Metabolic and cardiovascular adverse effects associated with antipsychotic drugs. Nat Rev Endocrinol. 2011;8:114–26.
Zullino D, Bilancioni R, Conus P, Schwartz B, Khazaal Y, Baumann P. Off-label utilization of antipsychotics. South Afr Psychiatry Rev. 2006;9:38–43.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA Statement. PLoS Med. 2009;6:e1000097.
Bogenschutz MP, George Nurnberg H. Olanzapine versus placebo in the treatment of borderline personality disorder. J Clin Psychiatry. 2004;65:104–9.
Linehan MM, McDavid JD, Brown MZ, Sayrs JH, Gallop RJ. Olanzapine plus dialectical behavior therapy for women with high irritability who meet criteria for borderline personality disorder: a double-blind, placebo-controlled pilot study. J Clin Psychiatry. 2008;69:999–1005.
Schulz SC, Zanarini MC, Bateman A, Bohus M, Detke HC, Trzaskoma Q, et al. Olanzapine for the treatment of borderline personality disorder: variable dose 12-week randomised double-blind placebo-controlled study. Br J Psychiatry. 2008;193:485–92.
Soler J, Pascual JC, Campins J, Barrachina J, Puigdemont D, Alvarez E, et al. Double-blind, placebo-controlled study of dialectical behavior therapy plus olanzapine for borderline personality disorder. Am J Psychiatry. 2005;162:1221–4.
Zanarini MC, Frankenburg FR. Olanzapine treatment of female borderline personality disorder patients: a double-blind, placebo-controlled pilot study. J Clin Psychiatry. 2001;62:849–54.
Zanarini MC, Schulz SC, Detke HC, Tanaka Y, Zhao F, Lin D, et al. A dose comparison of olanzapine for the treatment of borderline personality disorder: a 12-week randomized, double-blind, placebo-controlled study. J Clin Psychiatry. 2011;72:1353–62.
Carey P, Suliman S, Ganesan K, Seedat S, Stein DJ. Olanzapine monotherapy in posttraumatic stress disorder: efficacy in a randomized, double-blind, placebo-controlled study. Hum Psychopharmacol. 2012;27:386–91.
Stein MB, Kline NA, Matloff JL. Adjunctive olanzapine for SSRI-resistant combat-related PTSD: a double-blind, placebo-controlled study. Am J Psychiatry. 2002;159:1777–9.
Van Ameringen M, Mancini C, Patterson B, Bennett M, Oakman J. A randomized, double-blind, placebo-controlled trial of olanzapine in the treatment of trichotillomania. J Clin Psychiatry. 2010;71:1336–43.
Pollack MH, Simon NM, Zalta AK, Worthington JJ, Hoge EA, Mick E, et al. Olanzapine augmentation of fluoxetine for refractory generalized anxiety disorder: a placebo controlled study. Biol Psychiatry. 2006;59:211–5.
Shapira NA, Ward HE, Mandoki M, Murphy TK, Yang MC, Blier P, et al. A double-blind, placebo-controlled trial of olanzapine addition in fluoxetine-refractory obsessive-compulsive disorder. Biol Psychiatry. 2004;55:553–5.
McElroy SL, Nelson EB, Welge JA, Kaehler L, Keck PE Jr. Olanzapine in the treatment of pathological gambling: a negative randomized placebo-controlled trial. J Clin Psychiatry. 2008;69:433–40.
Bartzokis G, Lu PH, Turner J, Mintz J, Saunders CS. Adjunctive risperidone in the treatment of chronic combat-related posttraumatic stress disorder. Biol Psychiatry. 2005;57:474–9.
Reich DB, Winternitz S, Hennen J, Watts T, Stanculescu C. A preliminary study of risperidone in the treatment of posttraumatic stress disorder related to childhood abuse in women. J Clin Psychiatry. 2004;65:1601–6.
Krystal JH, Rosenheck RA, Cramer JA, Vessicchio JC, Jones KM, Vertrees JE, et al. Adjunctive risperidone treatment for antidepressant-resistant symptoms of chronic military service-related PTSD: a randomized trial. Jama 2011;306:493–502.
Brawman-Mintzer O, Knapp RG, Nietert PJ. Adjunctive risperidone in generalized anxiety disorder: a double-blind, placebo-controlled study. J Clin Psychiatry. 2005;66:1321–5.
Pandina GJ, Canuso CM, Turkoz I, Kujawa M, Mahmoud RA. Adjunctive risperidone in the treatment of generalized anxiety disorder: a double-blind, prospective, placebo-controlled, randomized trial. Psychopharmacol Bull. 2007;40:41–57.
Loebl T, Angarita GA, Pachas GN, Huang KL, Lee SH, Nino J, et al. A randomized, double-blind, placebo-controlled trial of long-acting risperidone in cocaine-dependent men. J Clin Psychiatry. 2008;69:480–6.
Bandelow B, Chouinard G, Bobes J, Ahokas A, Eggens I, Liu S, et al. Extended-release quetiapine fumarate (quetiapine XR): a once-daily monotherapy effective in generalized anxiety disorder. Data from a randomized, double-blind, placebo- and active-controlled study. Int J Neuropsychopharmacol. 2010;13:305–20.
Khan A, Joyce M, Atkinson S, Eggens I, Baldytcheva I, Eriksson H. A randomized, double-blind study of once-daily extended release quetiapine fumarate (quetiapine XR) monotherapy in patients with generalized anxiety disorder. J Clin Psychopharmacol. 2011;31:418–28.
Merideth C, Cutler AJ, She F, Eriksson H. Efficacy and tolerability of extended release quetiapine fumarate monotherapy in the acute treatment of generalized anxiety disorder: a randomized, placebo controlled and active-controlled study. Int Clin Psychopharmacol. 2012;27:40–54.
Bai YM, Ting Chen T, Chen JY, Chang WH, Wu B, Hung CH, et al. Equivalent switching dose from oral risperidone to risperidone long-acting injection: a 48-week randomized, prospective, single-blind pharmacokinetic study. J Clin Psychiatry. 2007;68:1218–25.
Khan A, Atkinson S, Mezhebovsky I, She F, Leathers T, Pathak S. Extended-release quetiapine fumarate (quetiapine XR) as adjunctive therapy in patients with generalized anxiety disorder and a history of inadequate treatment response: a randomized, double-blind study. Ann Clin Psychiatry. 2013;25:E7–22.
Katzman MA, Brawman-Mintzer O, Reyes EB, Olausson B, Liu S, Eriksson H. Extended release quetiapine fumarate (quetiapine XR) monotherapy as maintenance treatment for generalized anxiety disorder: a long-term, randomized, placebo-controlled trial. Int Clin Psychopharmacol. 2011;26:11–24.
Simon NM, Connor KM, LeBeau RT, Hoge EA, Worthington JJ 3rd, Zhang W, et al. Quetiapine augmentation of paroxetine CR for the treatment of refractory generalized anxiety disorder: preliminary findings. Psychopharmacol. 2008;197:675–81.
Vulink NC, Denys D, Fluitman SB, Meinardi JC, Westenberg HG. Quetiapine augments the effect of citalopram in non-refractory obsessive-compulsive disorder: a randomized, double-blind, placebo-controlled study of 76 patients. J Clin Psychiatry. 2009;70:1001–8.
Atmaca M, Kuloglu M, Tezcan E, Gecici O. Quetiapine augmentation in patients with treatment resistant obsessive-compulsive disorder: a single-blind, placebo-controlled study. Int Clin Psychopharmacol. 2002;17:115–9.
Black DW, Zanarini MC, Romine A, Shaw M, Allen J, Schulz SC. Comparison of low and moderate dosages of extended-release quetiapine in borderline personality disorder: a randomized, double-blind, placebo-controlled trial. Am J Psychiatry. 2014;171:1174–82.
Goddard AW, Mahmud W, Medlock C, Shin YW, Shekhar A. A controlled trial of quetiapine XR coadministration treatment of SSRI-resistant panic disorder. Ann Gen Psychiatry. 2015;14:26.
Villarreal G, Hamner MB, Cañive JM, Robert S, Calais LA, Durklaski V, et al. Efficacy of Quetiapine Monotherapy in Posttraumatic Stress Disorder: A Randomized, Placebo-Controlled Trial. Am J Psychiatry. 2016;173:1205–12.
Javdan NS, Ghoreishi FS, Sehat M, Ghaderi A, Banafshe HR. Mental health and cognitive function responses to quetiapine in patients with methamphetamine abuse under methadone maintenance treatment. J Affect Disord. 2019;251:235–41.
Storch EA, Goddard AW, Grant JE, De Nadai AS, Goodman WK, Mutch PJ, et al. Double-blind, placebo-controlled, pilot trial of paliperidone augmentation in serotonin reuptake inhibitor-resistant obsessive-compulsive disorder. J Clin Psychiatry. 2013;74:e527–32.
Lohoff FW, Etemad B, Mandos LA, Gallop R, Rickels K. Ziprasidone treatment of refractory generalized anxiety disorder: a placebo-controlled, double-blind study. J Clin Psychopharmacol. 2010;30:185–9.
Denys D, de Geus F, van Megen HJ, Westenberg HG. A double-blind, randomized, placebo-controlled trial of quetiapine addition in patients with obsessive-compulsive disorder refractory to serotonin reuptake inhibitors. J Clin Psychiatry. 2004;65:1040–8.
Heyer DB, Meredith RM. Environmental toxicology: Sensitive periods of development and neurodevelopmental disorders. Neurotoxicology 2017;58:23–41.
Mariani JJ, Pavlicova M, Jean Choi C, Basaraba C, Carpenter KM, Mahony AL, et al. Quetiapine treatment for cannabis use disorder. Drug Alcohol Depend. 2020;218:108366.
Sayyah M, Sayyah M, Boostani H, Ghaffari SM, Hoseini A. Effects of aripiprazole augmentation in treatment-resistant obsessive-compulsive disorder (a double blind clinical trial). Depress Anxiety. 2012;29:850–4.
Farr OM, Sloan DM, Keane TM, Mantzoros CS. Stress- and PTSD-associated obesity and metabolic dysfunction: a growing problem requiring further research and novel treatments. Metab: Clin Exp. 2014;63:1463–68.
Barton BB, Segger F, Fischer K, Obermeier M, Musil R. Update on weight-gain caused by antipsychotics: a systematic review and meta-analysis. Expert Opin Drug Saf. 2020;19:295–314.
Zipursky RB, Gu H, Green AI, Perkins DO, Tohen MF, McEvoy JP, et al. Course and predictors of weight gain in people with first-episode psychosis treated with olanzapine or haloperidol. Br J Psychiatry. 2005;187:537–43.
Correll CU, Manu P, Olshanskiy V, Napolitano B, Kane JM, Malhotra AK. Cardiometabolic risk of second-generation antipsychotic medications during first-time use in children and adolescents. JAMA 2009;302:1765–73.
Pillinger T, McCutcheon RA, Vano L, Mizuno Y, Arumuham A, Hindley G, et al. Comparative effects of 18 antipsychotics on metabolic function in patients with schizophrenia, predictors of metabolic dysregulation, and association with psychopathology: a systematic review and network meta-analysis. Lancet Psychiatry. 2020;7:64–77.
Rummel-Kluge C, Komossa K, Schwarz S, Hunger H, Schmid F, Lobos CA, et al. Head-to-head comparisons of metabolic side effects of second generation antipsychotics in the treatment of schizophrenia: a systematic review and meta-analysis. Schizophr Res. 2010;123:225–33.
Newcomer JW. Second-generation (atypical) antipsychotics and metabolic effects: a comprehensive literature review. CNS Drugs. 2005;19:1–93. Suppl 1
Meyer JM, Koro CE. The effects of antipsychotic therapy on serum lipids: a comprehensive review. Schizophr Res. 2004;70:1–17.
Kang SH, Lee JI. Metabolic disturbances independent of body mass in patients with schizophrenia taking atypical antipsychotics. Psychiatry Investig. 2015;12:242.
Spertus J, Horvitz-Lennon M, Abing H, Normand SL. Risk of weight gain for specific antipsychotic drugs: a meta-analysis. NPJ Schizophr. 2018;4:12.
Simon V, van Winkel R, De Hert M. Are weight gain and metabolic side effects of atypical antipsychotics dose dependent? A literature review. J Clin Psychiatry. 2009;70:1041–50.
Brecher M, Leong RW, Stening G, Osterling-Koskinen L, Jones AM. Quetiapine and long-term weight change: a comprehensive data review of patients with schizophrenia. J Clin Psychiatry. 2007;68:597–603.
Højlund M, Lund LC, Andersen K, Correll CU, Hallas J. Association of low-dose quetiapine and diabetes. JAMA Netw Open. 2021;4:e213209.
Leslie DL, Rosenheck R. Off-label use of antipsychotic medications in Medicaid. Am J Manag Care. 2012;18:e109–17.
Castellani LN, Costa-Dookhan KA, McIntyre WB, Wright DC, Flowers SA, Hahn MK, et al. Preclinical and clinical sex differences in antipsychotic-induced metabolic disturbances: a narrative review of adiposity and glucose metabolism. J Psychiatr Brain Sci. 2019;4:e190013.
Liu J, Hanley AJG, Young TK, Harris SB, Zinman B. Characteristics and prevalence of the metabolic syndrome among three ethnic groups in Canada. Int J Obes. 2006;30:669–76.
Hildrum B, Mykletun A, Hole T, Midthjell K, Dahl AA. Age-specific prevalence of the metabolic syndrome defined by the international diabetes federation and the national cholesterol education program: the Norwegian HUNT 2 study. BMC Public Health. 2007;7:220.
Funding
N.S. is supported by the CIHR Canada Graduate Scholarship Master’s Program (CGS-M) and the Banting and Best Diabetes Centre (BBDC) Novo-Nordisk Graduate Studentship. E.S. is supported by the CIHR Canada Graduate Scholarship Master’s Program (CGS-M) and the Banting and Best Diabetes Centre (BBDC) Novo-Nordisk Graduate Studentship. S.B. Nothing to declare. V.T. Nothing to declare. R.A. is supported by the Banting and Best Diabetes Centre (BBDC) Novo-Nordisk Graduate Studentship and the Cleghorn Award. W.B.M. Nothing to declare. G.R. has received research support from the Canadian Institutes of Health Research (CIHR), University of Toronto, Research Hospital Fund–Canada Foundation for Innovation (RHF-CFI), and HLS Therapeutics Inc. He has received advisory board support from HLS Therapeutics and consultant fees from Mitsubishi Tanabe Pharma Corporation. S.M.A. is supported in part by an Academic Scholars Award from the Department of Psychiatry, University of Toronto, and has grant support from the Canadian Institutes of Health Research, PSI Foundation, Ontario, and the CAMH Discovery Fund. D.S. is supported in part by an NHMRC Emerging Leadership Fellowship GNT1194635. M.K.H. is supported in part by an Academic Scholars Award from the Department of Psychiatry, University of Toronto, and has grant support from the Banting and Best Diabetes Center (BBDC), the Canadian Institutes of Health Research (PJT-153262) (CIHR), PSI Foundation, Ontario, holds the Kelly and Michael Meighen Chair in Psychosis Prevention, and the Cardy Schizophrenia Research Chair.
Author information
Authors and Affiliations
Contributions
All authors contributed to drafting and revising the manuscript and approved its final version. S.M.A., D.S., and M.K.H. were involved in the concept and design of the study. N.S. and E.S. were involved in the systematic search, screening of articles, extraction of data, risk of bias assessment, and statistical analysis. S.B. was involved in the systematic search, screening of articles, extraction of data, and statistical analysis. V.T. was involved in the systematic search, screening of articles, and extraction of data. R.A. and W.M. were involved in the screening of articles, data extraction, and risk of bias assessment. G.R revised the work critically and provided suggestions for improvement.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Stogios, N., Smith, E., Bowden, S. et al. Metabolic adverse effects of off-label use of second-generation antipsychotics in the adult population: a systematic review and meta-analysis. Neuropsychopharmacol. 47, 664–672 (2022). https://doi.org/10.1038/s41386-021-01163-7
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41386-021-01163-7
This article is cited by
-
Prescribing and deprescribing of atypical antipsychotics in older multimorbid patients
BMC Geriatrics (2025)
-
Pomgulated methionil (LY2140023) in schizophrenia patients: a systematic review and meta-analysis
BMC Psychiatry (2025)
-
Cardiometabolic adverse effects of long-term antipsychotic treatment in children and adolescents with non-psychotic disorders: a systematic review of available evidence
European Child & Adolescent Psychiatry (2025)
-
QT Interval, Antipsychotics and Correlates Among Patients with Schizophrenia: Cross-Sectional Data from the Multicentric Real-World FACE-SZ
Drug Safety (2025)
-
Antipsychotic-Induced Weight Gain in Severe Mental Illness: Risk Factors and Special Considerations
Current Psychiatry Reports (2023)