Abstract
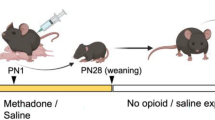
The current opioid epidemic has dramatically increased the number of children who are prenatally exposed to opioids, including oxycodone. A number of social and cognitive abnormalities have been documented in these children as they reach young adulthood. However, little is known about the mechanisms underlying developmental effects of prenatal opioid exposure. Microglia, the resident immune cells of the brain, respond to acute opioid exposure in adulthood. Moreover, microglia are known to sculpt neural circuits during typical development. Indeed, we recently found that microglial phagocytosis of dopamine D1 receptors (D1R) in the nucleus accumbens (NAc) is required for the natural developmental decline in NAc-D1R that occurs between adolescence and adulthood in rats. This microglial pruning occurs only in males, and is required for the normal developmental trajectory of social play behavior. However, virtually nothing is known as to whether this developmental program is altered by prenatal exposure to opioids. Here, we show in rats that maternal oxycodone self-administration during pregnancy leads to reduced adolescent microglial phagocytosis of D1R and subsequently higher D1R density within the NAc in adult male, but not female, offspring. Finally, we show prenatal and adult behavioral deficits in opioid-exposed offspring, including impaired extinction of oxycodone-conditioned place preference in males. This work demonstrates for the first time that microglia play a key role in translating prenatal opioid exposure to changes in neural systems and behavior.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Haight SC, Ko JY, Tong VT, Bohm MK, Callaghan WM. Opioid use disorder documented at delivery hospitalization—United States, 1999–2014. MMWR Morb Mortal Wkly Rep. 2018;67:845–9.
Conradt E, Flannery T, Aschner JL, Annett RD, Croen LA, Duarte CS.et al. Prenatal opioid exposure: neurodevelopmental consequences and future research priorities. Pediatrics. 2019;144: https://doi.org/10.1542/peds.2019-0128.
Arter S, Lambert J, Brokman A, Fall N. Diagnoses during the first three years of life for children with prenatal opioid exposure and neonatal abstinence syndrome using a large maternal-infant data hub. J Pediatr Nurs. 2021;61:34–9.
Nygaard E, Moe V, Slinning K, Walhovd KB. Longitudinal cognitive development of children born to mothers with opioid and polysubstance use. Pediatr Res. 2015;78:330–5.
van Baar A, de Graaff BM. Cognitive development at preschool-age of infants of drug-dependent mothers. Dev Med Child Neurol. 1994;36:1063–75.
Moe V. Foster-placed and adopted children exposed in utero to opiates and other substances: prediction and outcome at four and a half years. J Dev Behav Pediatr. 2002;23:330–9.
Hunt RW, Tzioumi D, Collins E, Jeffery HE. Adverse neurodevelopmental outcome of infants exposed to opiate in-utero. Early Hum Dev. 2008;84:29–35.
Benninger KL, Borghese T, Kovalcik JB, Moore-Clingenpeel M, Isler C, Bonachea EM, et al. Prenatal exposures are associated with worse neurodevelopmental outcomes in infants with neonatal opioid withdrawal syndrome. Front Pediatr. 2020;8:462.
Sandtorv LB, Fevang SKE, Nilsen SA, Bøe T, Gjestad R, Haugland S, et al. Symptoms associated with attention-deficit/hyperactivity disorder and autism spectrum disorders in school-aged children prenatally exposed to substances. Subst Abus. 2018;12:1178221818765773.
de Cubas MM, Field T. Children of methadone-dependent women: developmental outcomes. Am J Orthopsychiatry. 1993;63:266–76.
Nygaard E, Slinning K, Moe V, Walhovd KB. Cognitive function of youths born to mothers with opioid and poly-substance abuse problems during pregnancy. Child Neuropsychol. 2017;23:159–87.
Singer LT, Chambers C, Coles C, Kable J. Fifty years of research on prenatal substances: lessons learned for the opioid epidemic. Advers Resil Sci. 2020;1:223–34.
Skumlien M, Ibsen IO, Kesmodel US, Nygaard E. Sex differences in early cognitive development after prenatal exposure to opioids. J Pediatr Psychol. 2020;45:475–85.
Grecco GG, Atwood BK, Prenatal Opioid exposure enhances responsiveness to future drug reward and alters sensitivity to pain: a review of preclinical models and contributing mechanisms. eNeuro. 2020;7. https://doi.org/10.1523/ENEURO.0393-20.2020.
Minakova E, Sarafinovska S, Mikati MO, Barclay KM, McCullough KB, Dougherty JD, et al. Ontogenetic oxycodone exposure affects early life communicative behaviors, sensorimotor reflexes, and weight trajectory in mice. Front Behav Neurosci. 2021;15:615798.
Byrnes EM, Vassoler FM. Modeling prenatal opioid exposure in animals: Current findings and future directions. Front Neuroendocrinol. 2018;51:1–13.
Abu Y, Roy S. Prenatal opioid exposure and vulnerability to future substance use disorders in offspring. Exp Neurol. 2021;339:113621.
Vassoler FM, Oranges ML, Toorie AM, Byrnes EM. Oxyxodone self-administration during pregnancy disrupts the maternal-infant dyad and decreases midbrain OPRM1 expression during early postnatal development in rats. Pharm Biochem Behav. 2018;173:74–83.
Shen Y-L, Chen S-T, Chan T-Y, Hung T-W, Tao P-L, Liao R-M, et al. Delayed extinction and stronger drug-primed reinstatement of methamphetamine seeking in rats prenatally exposed to morphine. Neurobiol Learn Mem. 2016;128:56–64.
Wong C-S, Lee Y-J, Chiang Y-C, Fan L-W, Ho I-K, Tien L-T. Effect of prenatal methadone on reinstated behavioral sensitization induced by methamphetamine in adolescent rats. Behav Brain Res. 2014;258:160–5.
Kopec AM, Smith CJ, Ayre NR, Sweat SC, Bilbo SD. Microglial dopamine receptor elimination defines sex-specific nucleus accumbens development and social behavior in adolescent rats. Nat Commun. 2018;9:3769.
Tarazi FI, Baldessarini RJ. Comparative postnatal development of dopamine D(1), D(2), and D(4) receptors in rat forebrain. Int J Dev Neurosci. 2000;18:29–37.
Jantzie LL, Maxwell JR, Newville JC, Yellowhair TR, Kitase Y, Madurai N, et al. Prenatal opioid exposure: The next neonatal neuroinflammatory disease. Brain Behav Immun. 2020;84:45–58.
Mavrikaki M, Pravetoni M, Page S, Potter D, Chartoff E. Oxycodone self-administration in male and female rats. Psychopharmacology 2017;234:977–87.
Paxinos G, Watson C, The rat brain in stereotaxic coordinates: Hard Cover Edition. Elsevier; 2006.
Russell SE, Puttick DJ, Sawyer AM, Potter DN, Mague S, Carlezon WA Jr, et al. Nucleus accumbens AMPA receptors are necessary for morphine-withdrawal-induced negative-affective states in rats. J Neurosci. 2016;36:5748–62.
Faust TE, Gunner G, Schafer DP. Mechanisms governing activity-dependent synaptic pruning in the developing mammalian CNS. Nat Rev Neurosci. 2021;22:657–73.
VanRyzin JW, Marquardt AE, Argue KJ, Vecchiarelli HA, Ashton SE, Arambula SE, et al. Microglial phagocytosis of newborn cells is induced by endocannabinoids and sculpts sex differences in juvenile rat social play. Neuron 2019;102:435–449. e6.
Seney ML, Kim S-M, Glausier JR, Hildebrand MA, Xue X, Zong W, et al. Transcriptional alterations in dorsolateral prefrontal cortex and nucleus accumbens implicate neuroinflammation and synaptic remodeling in opioid use disorder. Biol Psychiatry. 2021;90:550–62.
Schwarz JM, Smith SH, Bilbo SD. FACS analysis of neuronal-glial interactions in the nucleus accumbens following morphine administration. Psychopharmacology. 2013;230:525–35.
Rivera PD, Hanamsagar R, Kan MJ, Tran PK, Stewart D, Jo YC, et al. Removal of microglial-specific MyD88 signaling alters dentate gyrus doublecortin and enhances opioid addiction-like behaviors. Brain Behav Immun. 2019;76:104–15.
Patrick SW, Barfield WD, Poindexter BB. Neonatal opioid withdrawal syndrome. Pediatrics 2020;146:1–18.
Chini M, Hanganu-Opatz IL. Prefrontal cortex development in health and disease: lessons from rodents and humans. Trends Neurosci. 2021;44:227–40.
Bordt EA, Ceasrine AM, Bilbo SD. Microglia and sexual differentiation of the developing brain: A focus on ontogeny and intrinsic factors. Glia 2020;68:1085–99.
VanRyzin JW, Marquardt AE, Pickett LA, McCarthy MM. Microglia and sexual differentiation of the developing brain: A focus on extrinsic factors. Glia 2020;68:1100–13.
Klein SL, Flanagan KL. Sex differences in immune responses. Nat Rev Immunol. 2016;16:626–38.
Acknowledgements
We thank all the members of the Bilbo lab for their critical reading of the manuscript, as well as Dr. Ravikiran Raju for providing his clinical insight as a neonatologist. We thank the Animal Care staff at McLean Hospital for providing excellent animal care and the staff of the Duke Light Microscopy Core for assistance with learning and trouble-shooting confocal microscopy.
Funding
This work was supported by NIH R21DA048399 to EHC and SDB, NIH F32ES029912 to CJS, and by a Harvard University Mind, Brain, and Behavior Faculty Research Award to EHC and SDB.
Author information
Authors and Affiliations
Contributions
EHC, SDB, CJS, and TL designed the study. CJS, TL, MJC, KEM, NC, AA, YAC, VJK, and YCJ conducted experiments. CJS, EHC, and SDB wrote the manuscript. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Smith, C.J., Lintz, T., Clark, M.J. et al. Prenatal opioid exposure inhibits microglial sculpting of the dopamine system selectively in adolescent male offspring. Neuropsychopharmacol. 47, 1755–1763 (2022). https://doi.org/10.1038/s41386-022-01376-4
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41386-022-01376-4
This article is cited by
-
The ultrasonic vocalization (USV) syllable profile during neonatal opioid withdrawal and a kappa opioid receptor component to increased USV emissions in female mice
Psychopharmacology (2025)
-
Effect of prenatal and early post-natal oxycodone exposure on the reinforcing and antinociceptive effects of oxycodone in adult C57BL/6 J mice
Psychopharmacology (2024)