Abstract
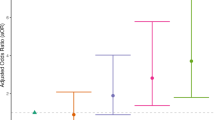
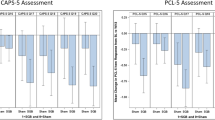
Little is understood about cognitive mechanisms that confer risk and resiliency for posttraumatic stress disorder (PTSD). Prepulse Inhibition (PPI) is a measure of pre-attentional response inhibition that is a stable cognitive trait disrupted in many neuropsychiatric disorders characterized by poor behavioral or cognitive inhibition, including PTSD. Differentiating between PTSD-related phenotypes that are pre-existing factors vs. those that emerge specifically after trauma is critical to understanding PTSD etiology and can only be addressed by prospective studies. This study tested the hypothesis that sensorimotor gating performance is associated with risk/resiliency for combat-related PTSD. As part of a prospective, longitudinal study, 1226 active duty Marines and Navy Corpsman completed a PPI test as well as a clinical interview to assess PTSD symptoms both before, and 3 and 6 months after a combat deployment. Participants that developed PTSD 6 months following deployment (N=46) showed lower PPI across pre and post-deployment time points compared to participants who did not develop PTSD (N=1182) . Examination of the distribution of PTSD across PPI performance revealed a lower than expected number of cases in the highest performing quartile compared to the rest of the distribution (p < 0.04). When controlling for other factors that predict PTSD in this population, those in the top 25% of PPI performance showed a >50% reduction in chance to develop PTSD (OR = 0.32). Baseline startle reactivity and startle habituation were not significantly different between PTSD risk and control groups. These findings suggest that robust sensorimotor gating may represent a resiliency factor for development of PTSD following trauma.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Druss BG, Hwang I, Petukhova M, Sampson NA, Wang PS, Kessler RC. Impairment in role functioning in mental and chronic medical disorders in the United States: results from the National Comorbidity Survey Replication. Mol Psychiatry. 2008;14:728–37.
Alonso J, Angermeyer MC, Bernert S, Bruffaerts R, Brugha TS, Bryson H, et al. Disability and quality of life impact of mental disorders in Europe: results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. Acta Psychiatr Scand Suppl. 2004;109:21–27.
Breslau N. The epidemiology of trauma, PTSD, and other posttrauma disorders. Trauma Violence Abuse. 2009;10:198–210.
Kilpatrick DG, Resnick HS, Milanak ME, Miller MW, Keyes KM, Friedman MJ. National estimates of exposure to traumatic events and PTSD prevalence using DSM-IV and DSM-5 criteria. J Trauma Stress. 2013;26:537–47.
Zhang L, Li H, Benedek D, Li X, Ursano R. A strategy for the development of biomarker tests for PTSD. Med Hypotheses. 2009;73:404–9.
Swerdlow NR, Braff DL, Geyer MA. Cross-species studies of sensorimotor gating of the startle reflex. Ann N Y Acad Sci. 1999;877:202–16.
Greenwood TA, Braff DL, Light GA, Cadenhead KS, Calkins ME, Dobie DJ, et al. Initial heritability analyses of endophenotypic measures for Schizophrenia: the consortium on the genetics of schizophrenia. Arch Gen Psychiatry. 2007;64:1242–50.
Kohl S, Heekeren K, Klosterkötter J, Kuhn J. Prepulse inhibition in psychiatric disorders - apart from schizophrenia. J Psychiatr Res. 2013;47:445–52.
Flaten MA. Test-retest reliability of the somatosensory blink reflex and its inhibition. Int J Psychophysiol. 2002;45:261–5.
Abel K, Waikar M, Pedro B, Hemsley D, Geyer M. Repeated testing of prepulse inhibition and habituation of the startle reflex: a study in healthy human controls. J Psychopharmacol. 1998;12:330–7. 337
Schwarzkopf SB, McCoy L, Smith DA, Boutros NN. Test-retest reliability of prepulse inhibition of the acoustic startle response. Biol Psychiatry. 1993;34:896–900.
Ludewig K, Ludewig S, Seitz A, Obrist M, Geyer MA, Vollenweider FX. The acoustic startle reflex and its modulation: effects of age and gender in humans. Biol Psychol. 2003;63:311–23.
Francis DD, Szegda K, Campbell G, Martin WD, Insel TR. Epigenetic sources of behavioral differences in mice. Nat Neurosci. 2013;6:445–6.
Swerdlow NR, Light GA, Cadenhead KS, Sprock J, Hsieh MH, Braff DL. Startle gating deficits in a large cohort of patients with schizophrenia: relationship to medications, symptoms, neurocognition, and level of function. Arch Gen Psychiatry. 2006;63:1325–35.
Castellanos FX, Fine EJ, Kaysen D, Marsh WL, Rapoport JL, Hallett M. Sensorimotor gating in boys with Tourette’s syndrome and ADHD: preliminary results. Biol Psychiatry. 1996;39:33–41.
Perry W, Minassian A, Feifel D, Braff DL. Sensorimotor gating deficits in bipolar disorder patients with acute psychotic mania. Biol Psychiatry. 2001;50:418–24.
Ahmari SE, Risbrough VB, Geyer MA, Simpson HB. Impaired sensorimotor gating in unmedicated adults with obsessive-compulsive disorder. Neuropsychopharmacology. 2012;37:1216–23.
Ludewig S, Ludewig K, Geyer MA, Hell D, Vollenweider FX. Prepulse inhibition deficits in patients with panic disorder. Depress Anxiety. 2002;15:55–60.
Nievergelt CM, Maihofer AX, Klengel T, Atkinson EG, Chen CY, Choi KW, et al. International meta-analysis of PTSD genome-wide association studies identifies sex and ancestry-specific genetic risk loci. Nat Commun. 2019;10:4558.
Stein MB, Levey DF, Cheng Z, Wendt FR, Harrington K, Pathak GA, et al. Genome-wide association analyses of post-traumatic stress disorder and its symptom subdomains in the Million Veteran Program. Nat Genet. 2021;53:174–84.
Risbrough VB, Vaughn MN, Friend SF. Role of inflammation in traumatic brain injury–associated risk for neuropsychiatric disorders: state of the evidence and where do we go from here. Biol Psychiatry. 2022;91:438–48.
Swerdlow NR, Braff DL, Geyer MA. Sensorimotor gating of the startle reflex: What we said 25 years ago, what has happened since then, and what comes next. Psychopharmacology. 2016;30:1072–81.
Swerdlow NR, Geyer MA, Braff DL. Neural circuit regulation of prepulse inhibition of startle in the rat: current knowledge and future challenges. Psychopharmacology. 2001;156:194–215.
Naysmith LF, Kumari V, Williams SCR. Neural mapping of prepulse-induced startle reflex modulations as indices of sensory information processing in healthy and clinical populations: a systematic review. Hum Brain Mapp. 2021;42:5495–518.
Braff DL, Geyer MA, Swerdlow NR. Human studies of prepulse inhibition of startle: normal subjects, patient groups, and pharmacological studies. Psychopharmacology. 2001;156:234–58.
Acheson DT, Gresack JE, Risbrough VB. Hippocampal dysfunction effects on context memory: Possible etiology for posttraumatic stress disorder. Neuropharmacology. 2012;62:674–85.
Ressler KJ, Berretta S, Bolshakov VY, Rosso IM, Meloni EG, Rauch SL, et al. Post-traumatic stress disorder: clinical and translational neuroscience from cells to circuits. Nat Rev Neurol. 2022;18:273–88.
Ornitz EM, Pynoos RS. Startle modulation in children with posttraumatic stress disorder. Am J Psychiatry. 1989;146:866–70.
Grillon C, Morgan CA, Southwick SM, Davis M, Charney DS. Baseline startle amplitude and prepulse inhibition in Vietnam veterans with posttraumatic stress disorder. Psychiatry Res. 1996;64:169–78.
Grillon C, Morgan CA 3rd, Davis M, Southwick SM. Effects of experimental context and explicit threat cues on acoustic startle in Vietnam veterans with posttraumatic stress disorder. Biol Psychiatry. 1998;44:1027–36.
Echiverri-Cohen AM, Zoellner LA, Ho W, Husain J. An analysis of inhibitory functioning in individuals with chronic posttraumatic stress disorder. J Anxiety Disord. 2016;37:94–103.
Pineles SL, Blumenthal TD, Curreri AJ, Nillni YI, Putnam KM, Resick PA, et al. Prepulse inhibition deficits in women with PTSD. Psychophysiology. 2016;53:1377–85.
Butler RW, Braff DL, Rausch JL, Jenkins MA, Sprock J, Geyer MA. Physiological evidence of exaggerated startle response in a subgroup of Vietnam veterans with combat-related PTSD. Am J Psychiatry. 1990;147:1308–12.
Lipschitz DS, Mayes LM, Rasmusson AM, Anyan W, Billingslea E, Gueorguieva R, et al. Baseline and modulated acoustic startle responses in adolescent girls with posttraumatic stress disorder. J Am Acad Child Adolesc Psychiatry. 2005;44:807–14.
Holstein DH, Vollenweider FX, Jancke L, Schopper C, Csomor PA. P50 suppression, prepulse inhibition, and startle reactivity in the same patient cohort suffering from posttraumatic stress disorder. J Affect Disord. 2010;126:188–97.
Vrana SR, Calhoun PS, McClernon FJ, Dennis MF, Lee ST, Beckham JC. Effects of smoking on the acoustic startle response and prepulse inhibition in smokers with and without posttraumatic stress disorder. Psychopharmacology. 2013;230:477–85.
Meteran H, Vindbjerg E, Wiingaard Uldall S, Glenthoj B, Carlsson J, Orange B. Startle habituation, senory, and sensorimotor gating in trauma-affected refuges with posttraumatic stress disorder. Psychol Med. 2018;49:581–9.
Bakshi VP, Alsene KM, Roseboom PH, Connors EE. Enduring sensorimotor gating abnormalities following predator exposure or corticotropin-releasing factor in rats: a model for PTSD-like information-processing deficits? Neuropharmacology. 2012;62:737–48.
Risbrough VB, Hauger RL, Roberts AL, Vale WW, Geyer MA. Corticotropin-releasing factor receptors CRF1 and CRF2 exert both additive and opposing influences on defensive startle behavior. J Neurosci. 2004;24:6545–52.
Flandreau E, Risbrough V, Lu A, Ableitner M, Geyer MA, Holsboer F, et al. Cell type-specific modifications of corticotropin-releasing factor (CRF) and its type 1 receptor (CRF) on startle behavior and sensorimotor gating. Psychoneuroendocrinology. 2014;53C:16–28.
Rajbhandari AK, Baldo BA, Bakshi VP. Predator stress-induced CRF release causes enduring sensitization of basolateral amygdala norepinephrine systems that promote PTSD-like startle abnormalities. J Neurosci. 2015;35:14270–85.
Baker DG, Nash WP, Litz BT, Geyer MA, Risbrough VB, Nievergelt CM, et al. Predictors of risk and resilience for posttraumatic stress disorder among ground combat Marines: methods of the Marine Resiliency Study. Prev Chronic Dis. 2012;9:E97.
Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, et al. The development of a Clinician-Administered PTSD Scale. J Trauma Stress. 1995;8:75–90.
Blanchard EB, Hickling EJ, Taylor AE, Forneris CA, Loos W, Jaccard J. Effects of varying scoring rules of the Clinician-Administered PTSD Scale (CAPS) for the diagnosis of post-traumatic stress disorder in motor vehicle accident victims. Behav Res Ther. 1995;33:471–5.
Blanchard EB, Hickling EJ, Taylor AE, Loos W. Psychiatric morbidity associated with motor vehicle accidents. J Nerv Ment Dis. 1995;183:495–504.
Blanchard EB, Hickling EJ, Buckley TC, Taylor AE, Vollmer A, Loos WR. Psychophysiology of posttraumatic stress disorder related to motor vehicle accidents: replication and extension. J Consult Clin Psychol. 1996;64:742–51.
Weathers FW, Ruscio AM, Keane TM. Psychometric properties of nine scoring rules for the Clinician-Administered Post-traumatic Stress Disorder Scale. Psychological Assess. 1999;11:124–33.
King LA, King DW, Vogt DS, Knight J, Samper RE. Deployment Risk and Resilience Inventory: a collection of measures for studying deployment-related experiences of military personnel and veterans. Mil Psychol. 2006;18:89–120.
Nievergelt CM, Maihofer AX, Shekhtman T, Libiger O, Wang X, Kidd KK, et al. Inference of human continental origin and admixture proportions using a highly discriminative ancestry informative 41-SNP panel. Investig Genet. 2013;4:13.
Yurgil KA, Barkauskas DA, Vasterling JJ, Nievergelt CM, Larson GE, Schork NJ, et al. Association between traumatic brain injury and risk of posttraumatic stress disorder in active-duty Marines. JAMA Psychiatry. 2014;71:149–57.
von Holst H, Cassidy JD. Mandate of the WHO Collaborating Centre Task Force on mild traumatic brain injury. J Rehabil Med. 2004:43;8–10.
Gray MJ, Litz BT, Hsu JL, Lombardo TW. Psychometric properties of the life events checklist. Assessment. 2004;11:330–41.
Braff DL, Grillon C, Geyer MA. Gating and habituation of the startle reflex in schizophrenic patients. Arch Gen Psychiatry. 1992;49:206–15.
Acheson DT, Stein MB, Paulus MP, Geyer MA, Risbrough VB. The effect of pregabalin on sensorimotor gating in ‘low’ gating humans and mice. Neuropharmacology. 2012;63:480–5.
Glenn DE, Acheson DT, Geyer MA, Nievergelt CM, Baker DG, Risbrough VB. High and low threshold for startle reactivity associated with Ptsd symptoms but not Ptsd risk: evidence from a prospective study of active duty marines. Depress Anxiety. 2016;33:192–202.
Acheson DT, Stein MB, Paulus MP, Ravindran L, Simmons AN, Lohr JB, et al. Effects of anxiolytic treatment on potentiated startle during aversive image anticipation. Hum Psychopharmacol Clin Exp. 2012;27:419–27.
Swerdlow NR, Sprock J, Light GA, Cadenhead K, Calkins ME, Dobie DJ, et al. Multi-site studies of acoustic startle and prepulse inhibition in humans: initial experience and methodological considerations based on studies by the Consortium on the Genetics of Schizophrenia. Schizophr Res. 2007;92:237–51.
Swerdlow NR, Light GA, Sprock J, Calkins ME, Green MF, Greenwood TA, et al. Deficient prepulse inhibition in schizophrenia detected by the multi-site COGS. Schizophr Res. 2014;152:503–12.
Acheson DT, Geyer MA, Risbrough VB. Psychophysiology in the study of psychological trauma: where are we now and where do we need to be? Curr Top Behav Neurosci. 2014;21:157–83.
Admon R, Milad MR, Hendler T. A causal model of post-traumatic stress disorder: disentangling predisposed from acquired neural abnormalities. Trends Cogn Sci. 2013;17:337–47.
Kumari V, Antonova E, Zachariah E, Galea A, Aasen I, Ettinger U, et al. Structural brain correlates of prepulse inhibition of the acoustic startle response in healthy humans. Neuroimage. 2005;26:1052–8.
Hazlett EA, Buchsbaum MS, Haznedar MM, Singer MB, Germans MK, Schnur DB, et al. Prefrontal cortex glucose metabolism and startle eyeblink modification abnormalities in unmedicated schizophrenia patients. Psychophysiology. 1998;35:186–98.
Neuner I, Stöcker T, Kellermann T, Ermer V, Wegener HP, Eickhoff SB, et al. Electrophysiology meets fMRI: neural correlates of the startle reflex assessed by simultaneous EMG-fMRI data acquisition. Hum Brain Mapp. 2010;31:1675–85.
Kumari V, Fannon D, Geyer MA, Premkumar P, Antonova E, Simmons A, et al. Cortical grey matter volume and sensorimotor gating in schizophrenia. Cortex. 2008;44:1206–14.
Ota M, Sato N, Matsuo J, Kinoshita Y, Kawamoto Y, Hori H, et al. Multimodal image analysis of sensorimotor gating in healthy women. Brain Res. 2013;1499:61–68.
Swerdlow NR, Light GA. Neurophysiological biomarkers informing the clinical neuroscience of schizophrenia: mismatch negativity and prepulse inhibition of startle. Curr Topics Behav Neurosci. 2022, in press..
Light GA, Swerdlow NR, Rissling AJ, Radant A, Sugar CA, Sprock J, et al. Characterization of neurophysiologic and neurocognitive biomarkers for use in genomic and clinical outcome studies of schizophrenia. PLoS ONE. 2012;7:e39434.
Greenwood TA, Light GA, Swerdlow NR, Calkins ME, Green MF, Gur RE, et al. Gating deficit heritability and correlation with increased clinical severity in schizophrenia patients with positive family history. Am J Psychiatry. 2016;173:385–91.
Quednow BB, Ejebe K, Wagner M. Meta-analysis on the association between genetic polymorphisms and prepulse inhibition of the acoustic startle response. Schizophr Res. 2018;198:52–59.
Vinogradov S, Fisher M, de Villers-Sidani E. Cognitive training for impaired neural systems in neuropsychiatric illness. Neuropsychopharmacology. 2012;37:43–76.
Funding
Support for this work includes NIMH P50MH096889 (DGB and VBR), a Department of Veterans Affairs Merit Award and NIH R01AA026560 (VBR), project No. SDR 09-0128 (DGB and VBR) from the Veterans Administration Health Service Research and Development, the US Marine Corps and Navy Bureau of Medicine and Surgery (DGB and VBR), and the Center of Excellence for Stress and Mental Health (all authors). VBR is also the recipient of a Research Career Scientist award (# IK6BX006186) from the Department of Veterans Affairs. The project described was also supported by the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant UL1 TR001414. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Author information
Authors and Affiliations
Contributions
VBR, MAG, and DGB designed the study and supervised data collection and edited the manuscript, DTA contributed to data collection, conducted the analysis, and lead the manuscript preparation, CMN, KAY, and VBR aided data collection, processing, and analysis and edited the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Acheson, D.T., Baker, D.G., Nievergelt, C.M. et al. Prospective longitudinal assessment of sensorimotor gating as a risk/resiliency factor for posttraumatic stress disorder. Neuropsychopharmacol. 47, 2238–2244 (2022). https://doi.org/10.1038/s41386-022-01460-9
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41386-022-01460-9