Abstract
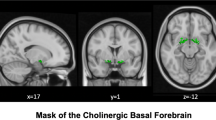
Schizophrenia is associated with widespread gray matter reduction. This is influenced by the underlying connectivity, resulting in covarying patterns of structural changes that are more pronounced in treatment-resistant individuals. However, it remains uncertain whether a distinct network of brain regions, with specific neurotransmitter basis, forms the substrate for treatment resistance in schizophrenia. We investigated the structural covariance networks (SCN) in 198 individuals; 55 with treatment-resistant schizophrenia (TRS) and 79 without TRS (non-TRS) in active symptomatic phase, and 64 healthy controls (HC) using Calhoun’s Source-Based Morphometry. We mapped the putative neurotransmitter basis of the SCNs using a PET-based chemoarchitectural atlas. Twelve independent components (i.e., SCNs) were identified. A prefrontal-limbic SCN had lower gray matter volume (GMV) in TRS compared to HC and non-TRS (F = 7.757, p < 0.001, FDR-corrected). Spatial correlation with chemoarchitectural atlas revealed predominant contributions from serotonergic [5HT1b and 5HT2a], glutamatergic [mGluR5], histaminergic [H3], and opioid [MOR] receptors for this TRS-related SCN (all pspin-permutation < 0.05, FDR-corrected). A different SCN comprised of dorsal fronto-temporal and parieto-occipital regions, not associated with any specific neurotransmitter distribution, exhibited reduced GMV in both TRS and non-TRS groups vs. HC (F = 7.239, p < 0.001, FDR-corrected). Amidst the generic GMV reduction that is shared with non-TRS patients, patients with TRS have specific prefrontal-limbic structural deficits with a unique non-dopaminergic chemoarchitecture. These findings indicate a putative molecular and structural basis for poor treatment response, guiding the development of second- and third-line pharmacotherapies for TRS.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 13 print issues and online access
$259.00 per year
only $19.92 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
The datasets generated and/or analyzed during the current study are not publicly available due that they contain patients’ personal information, and our hospital has strict data sharing policy, but are available from the corresponding author on reasonable request.
Code availability
The accompanying code for this study is available on GitHub (https://github.com/huanhuang1988/TRS_neuromaps).
References
Kane JM, Agid O, Baldwin ML, Howes O, Lindenmayer JP, Marder S, et al. Clinical guidance on the identification and management of treatment-resistant schizophrenia. J Clin Psychiatry. 2019;80:18com12123.
Howes OD, McCutcheon R, Agid O, de Bartolomeis A, van Beveren NJ, Birnbaum ML, et al. Treatment-resistant schizophrenia: treatment response and resistance in psychosis (TRRIP) working group consensus guidelines on diagnosis and terminology. Am J Psychiatry. 2017;174:216–29.
Farooq S, Hattle M, Kingstone T, Ajnakina O, Dazzan P, Demjaha A, et al. Development and initial evaluation of a clinical prediction model for risk of treatment resistance in first-episode psychosis: schizophrenia prediction of resistance to treatment (SPIRIT). Br J Psychiatry. 2024;225:379–88.
Lee R, Griffiths SL, Gkoutos GV, Wood SJ, Bravo-Merodio L, Lalousis PA, et al. Predicting treatment resistance in positive and negative symptom domains from first episode psychosis: development of a clinical prediction model. Schizophr Res. 2024;274:66–77.
Barruel D, Hilbey J, Charlet J, Chaumette B, Krebs MO, Dauriac-Le Masson V. Predicting treatment resistance in schizophrenia patients: machine learning highlights the role of early pathophysiologic features. Schizophr Res. 2024;270:1–10.
Llorca-Bofi V, Bioque M, Madero S, Mallorqui A, Oliveira C, Garriga M, et al. Blood cell count ratios at baseline are associated with initial clinical response to clozapine in treatment-resistant, clozapine-naive, schizophrenia-spectrum disorder. Pharmacopsychiatry. 2024;57:173–79.
Siskind D, Orr S, Sinha S, Yu O, Brijball B, Warren N, et al. Rates of treatment-resistant schizophrenia from first-episode cohorts: systematic review and meta-analysis. Br J Psychiatry. 2022;220:115–20.
Yoshimura B, Yada Y, So R, Takaki M, Yamada N. The critical treatment window of clozapine in treatment-resistant schizophrenia: secondary analysis of an observational study. Psychiatry Res. 2017;250:65–70.
Correll CU, Howes OD. Treatment-resistant schizophrenia: definition, predictors, and therapy options. J Clin Psychiatry. 2021;82:MY20096AH1C.
Mouchlianitis E, McCutcheon R, Howes OD. Brain-imaging studies of treatment-resistant schizophrenia: a systematic review. Lancet Psychiatry. 2016;3:451–63.
Anderson VM, Goldstein ME, Kydd RR, Russell BR. Extensive gray matter volume reduction in treatment-resistant schizophrenia. Int J Neuropsychopharmacol. 2015;18:pyv016.
Tronchin G, Akudjedu TN, Ahmed M, Holleran L, Hallahan B, Cannon DM, et al. Progressive subcortical volume loss in treatment-resistant schizophrenia patients after commencing clozapine treatment. Neuropsychopharmacology. 2020;45:1353–61.
Haijma SV, Van Haren N, Cahn W, Koolschijn PC, Hulshoff Pol HE, Kahn RS. Brain volumes in schizophrenia: a meta-analysis in over 18 000 subjects. Schizophr Bull. 2013;39:1129–38.
Nakajima S, Takeuchi H, Plitman E, Fervaha G, Gerretsen P, Caravaggio F, et al. Neuroimaging findings in treatment-resistant schizophrenia: a systematic review: lack of neuroimaging correlates of treatment-resistant schizophrenia. Schizophr Res. 2015;164:164–75.
Nucifora FC Jr., Woznica E, Lee BJ, Cascella N, Sawa A. Treatment resistant schizophrenia: clinical, biological, and therapeutic perspectives. Neurobiol Dis. 2019;131:104257.
Pan Y, Pu W, Chen X, Huang X, Cai Y, Tao H, et al. Morphological profiling of schizophrenia: cluster analysis of MRI-based cortical thickness data. Schizophr Bull. 2020;46:623–32.
Liang L, Heinrichs RW, Liddle PF, Jeon P, Theberge J, Palaniyappan L. Cortical impoverishment in a stable subgroup of schizophrenia: validation across various stages of psychosis. Schizophr Res. 2024;264:567–77.
Jiang Y, Wang J, Zhou E, Palaniyappan L, Luo C, Ji G, et al. Neuroimaging biomarkers define neurophysiological subtypes with distinct trajectories in schizophrenia. Nat Ment Health. 2023;1:186–99.
Jiang Y, Palaniyappan L, Luo C, Chang X, Zhang J, Tang Y, et al. Neuroimaging epicenters as potential sites of onset of the neuroanatomical pathology in schizophrenia. Sci Adv. 2024;10:eadk6063.
Palaniyappan L. Clusters of psychosis: compensation as a contributor to the heterogeneity of schizophrenia. J Psychiatry Neurosci. 2023;48:E325–E29.
Palaniyappan L. Progressive cortical reorganisation: a framework for investigating structural changes in schizophrenia. Neurosci Biobehav Rev. 2017;79:1–13.
Georgiadis F, Lariviere S, Glahn D, Hong LE, Kochunov P, Mowry B, et al. Connectome architecture shapes large-scale cortical alterations in schizophrenia: a worldwide ENIGMA study. Molecular psychiatry. 2024;29:1869–1881.
Potkin SG, Kane JM, Correll CU, Lindenmayer JP, Agid O, Marder SR, et al. The neurobiology of treatment-resistant schizophrenia: paths to antipsychotic resistance and a roadmap for future research. Focus Am Psychiatr Publ. 2020;18:456–65.
Jiang Y, Luo C, Wang J, Palaniyappan L, Chang X, Xiang S, et al. Neurostructural subgroup in 4291 individuals with schizophrenia identified using the subtype and stage inference algorithm. Nat Commun. 2024;15:5996.
Makhlouf AT, Drew W, Stubbs JL, Taylor JJ, Liloia D, Grafman J, et al. Heterogeneous patterns of brain atrophy in schizophrenia localize to a common brain network. Nat Ment Health. 2024;3:19–30.
Liu Z, Palaniyappan L, Wu X, Zhang K, Du J, Zhao Q, et al. Resolving heterogeneity in schizophrenia through a novel systems approach to brain structure: individualized structural covariance network analysis. Mol psychiatry. 2021;26:7719–31.
Xu L, Groth KM, Pearlson G, Schretlen DJ, Calhoun VD. Source-based morphometry: the use of independent component analysis to identify gray matter differences with application to schizophrenia. Hum Brain Mapp. 2009;30:711–24.
Gupta CN, Turner JA, Calhoun VD. Source-based morphometry: a decade of covarying structural brain patterns. Brain Struct Funct. 2019;224:3031–44.
Saha DK, Silva RF, Baker BT, Saha R, Calhoun VD. dcSBM: A federated constrained source-based morphometry approach for multivariate brain structure mapping. Hum Brain Mapp. 2023;44:5892–905.
Gupta CN, Calhoun VD, Rachakonda S, Chen J, Patel V, Liu J, et al. Patterns of gray matter abnormalities in schizophrenia based on an international mega-analysis. Schizophr Bull. 2015;41:1133–42.
Palaniyappan L, Mahmood J, Balain V, Mougin O, Gowland PA, Liddle PF. Structural correlates of formal thought disorder in schizophrenia: An ultra-high field multivariate morphometry study. Schizophr Res. 2015;168:305–12.
Wolf R, Huber M, Lepping P, Sambataro F, Depping MS, Karner M, et al. Source-based morphometry reveals distinct patterns of aberrant brain volume in delusional infestation. Prog Neuropsychopharmacol Biol Psychiatry. 2014;48:112–6.
Tsugawa S, Honda S, Noda Y, Wannan C, Zalesky A, Tarumi R, et al. Associations between structural covariance network and antipsychotic treatment response in schizophrenia. Schizophr Bull. 2024;50:382–92.
Hansen JY, Shafiei G, Markello RD, Smart K, Cox SML, Norgaard M, et al. Mapping neurotransmitter systems to the structural and functional organization of the human neocortex. Nat Neurosci. 2022;25:1569–81.
Leucht S, Samara M, Heres S, Patel MX, Woods SW, Davis JM. Dose equivalents for second-generation antipsychotics: the minimum effective dose method. Schizophr Bull. 2014;40:314–26.
Lally J, Ajnakina O, Di Forti M, Trotta A, Demjaha A, Kolliakou A, et al. Two distinct patterns of treatment resistance: clinical predictors of treatment resistance in first-episode schizophrenia spectrum psychoses. Psychol Med. 2016;46:3231–40.
Farooq S, Hattle M, Dazzan P, Kingstone T, Ajnakina O, Shiers D, et al. Study protocol for the development and internal validation of Schizophrenia Prediction of Resistance to Treatment (SPIRIT): a clinical tool for predicting risk of treatment resistance to antipsychotics in first-episode schizophrenia. BMJ Open. 2022;12:e056420.
Gaser C, Dahnke R, Thompson PM, Kurth F, Luders E, The Alzheimer's Disease Neuroimaging Initiative. CAT: a computational anatomy toolbox for the analysis of structural MRI data. Gigascience. 2024;13:giae049.
Bell AJ, Sejnowski TJ. An information-maximization approach to blind separation and blind deconvolution. Neural Comput. 1995;7:1129–59.
Schaefer A, Kong R, Gordon EM, Laumann TO, Zuo XN, Holmes AJ, et al. Local-global parcellation of the human cerebral cortex from intrinsic functional connectivity MRI. Cereb Cortex. 2018;28:3095–114.
Tian Y, Margulies DS, Breakspear M, Zalesky A. Topographic organization of the human subcortex unveiled with functional connectivity gradients. Nat Neurosci. 2020;23:1421–32.
Kasparek T, Marecek R, Schwarz D, Prikryl R, Vanicek J, Mikl M, et al. Source-based morphometry of gray matter volume in men with first-episode schizophrenia. Hum Brain Mapp. 2010;31:300–10.
Li M, Deng W, Li Y, Zhao L, Ma X, Yu H, et al. Ameliorative patterns of grey matter in patients with first-episode and treatment-naive schizophrenia. Psychol Med. 2023;53:3500–10.
Glahn DC, Laird AR, Ellison-Wright I, Thelen SM, Robinson JL, Lancaster JL, et al. Meta-analysis of gray matter anomalies in schizophrenia: application of anatomic likelihood estimation and network analysis. Biol Psychiatry. 2008;64:774–81.
Qiu L, Yan H, Zhu R, Yan J, Yuan H, Han Y, et al. Correlations between exploratory eye movement, hallucination, and cortical gray matter volume in people with schizophrenia. BMC Psychiatry. 2018;18:226.
Picado M, Carmona S, Hoekzema E, Pailhez G, Berge D, Mane A, et al. The neuroanatomical basis of panic disorder and social phobia in schizophrenia: a voxel based morphometric study. PLoS ONE. 2015;10:e0119847.
Moorhead TW, Job DE, Whalley HC, Sanderson TL, Johnstone EC, Lawrie SM. Voxel-based morphometry of comorbid schizophrenia and learning disability: analyses in normalized and native spaces using parametric and nonparametric statistical methods. Neuroimage. 2004;22:188–202.
Yeo BT, Krienen FM, Sepulcre J, Sabuncu MR, Lashkari D, Hollinshead M, et al. The organization of the human cerebral cortex estimated by intrinsic functional connectivity. J Neurophysiol. 2011;106:1125–65.
Fan L, Yu M, Pinkham A, Zhu Y, Tang X, Wang X, et al. Aberrant large-scale brain modules in deficit and non-deficit schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry. 2022;113:110461.
Nelson BG, Bassett DS, Camchong J, Bullmore ET, Lim KO. Comparison of large-scale human brain functional and anatomical networks in schizophrenia. Neuroimage Clin. 2017;15:439–48.
Rong B, Huang H, Gao G, Sun L, Zhou Y, Xiao L, et al. Widespread intra- and inter-network dysconnectivity among large-scale resting state networks in schizophrenia. J Clin Med. 2023;12:3176.
Geyer S, Schormann T, Mohlberg H, Zilles K. Areas 3a, 3b, and 1 of human primary somatosensory cortex. Part 2. Spatial normalization to standard anatomical space. Neuroimage. 2000;11:684–96.
Rao SM, Binder JR, Hammeke TA, Bandettini PA, Bobholz JA, Frost JA, et al. Somatotopic mapping of the human primary motor cortex with functional magnetic resonance imaging. Neurology. 1995;45:919–24.
Haber SN, Calzavara R. The cortico-basal ganglia integrative network: the role of the thalamus. Brain Res Bull. 2009;78:69–74.
Boos HB, Aleman A, Cahn W, Hulshoff Pol H, Kahn RS. Brain volumes in relatives of patients with schizophrenia: a meta-analysis. Arch Gen Psychiatry. 2007;64:297–304.
Skouras S, Kleinert ML, Lee EHM, Hui CLM, Suen YN, Camchong J, et al. Aberrant connectivity in the hippocampus, bilateral insula and temporal poles precedes treatment resistance in first-episode psychosis: a prospective resting-state functional magnetic resonance imaging study with connectivity concordance mapping. Brain Commun. 2024;6:fcae094.
Tronchin G, McPhilemy G, Ahmed M, Kilmartin L, Costello L, Forde NJ, et al. White matter microstructure and structural networks in treatment-resistant schizophrenia patients after commencing clozapine treatment: a longitudinal diffusion imaging study. Psychiatry Res. 2021;298:113772.
Horne CM, Vanes LD, Verneuil T, Mouchlianitis E, Szentgyorgyi T, Averbeck B, et al. Cognitive control network connectivity differentially disrupted in treatment resistant schizophrenia. Neuroimage Clin. 2021;30:102631.
Wada M, Nakajima S, Tarumi R, Masuda F, Miyazaki T, Tsugawa S, et al. Resting-state isolated effective connectivity of the cingulate cortex as a neurophysiological biomarker in patients with severe treatment-resistant schizophrenia. J Pers Med. 2020;10:89.
Chan NK, Kim J, Shah P, Brown EE, Plitman E, Carravaggio F, et al. Resting-state functional connectivity in treatment response and resistance in schizophrenia: a systematic review. Schizophr Res. 2019;211:10–20.
McNabb CB, Tait RJ, McIlwain ME, Anderson VM, Suckling J, Kydd RR, et al. Functional network dysconnectivity as a biomarker of treatment resistance in schizophrenia. Schizophr Res. 2018;195:160–67.
Mehta UM, Ithal D, Roy N, Shekhar S, Govindaraj R, Ramachandraiah CT, et al. Posterior cerebellar resting-state functional hypoconnectivity: a neural marker of schizophrenia across different stages of treatment response. Biol Psychiatry. 2024;96:365–75.
Palaniyappan L, Marques TR, Taylor H, Mondelli V, Reinders A, Bonaccorso S, et al. Globally efficient brain organization and treatment response in psychosis: a connectomic study of gyrification. Schizophr Bull. 2016;42:1446–56.
Wannan CMJ, Cropley VL, Chakravarty MM, Bousman C, Ganella EP, Bruggemann JM, et al. Evidence for network-based cortical thickness reductions in schizophrenia. Am J Psychiatry. 2019;176:552–63.
Ajnakina O, Das T, Lally J, Di Forti M, Pariante CM, Marques TR, et al. Structural covariance of cortical gyrification at illness onset in treatment resistance: a longitudinal study of first-episode psychoses. Schizophr Bull. 2021;47:1729–39.
Jiang Y, Wang Y, Huang H, He H, Tang Y, Su W, et al. Antipsychotics effects on network-level reconfiguration of cortical morphometry in first-episode schizophrenia. Schizophr Bull. 2022;48:231–40.
Saiz-Masvidal C, Contreras F, Soriano-Mas C, Mezquida G, Diaz-Caneja CM, Vieta E, et al. Structural covariance predictors of clinical improvement at 2-year follow-up in first-episode psychosis. Prog Neuropsychopharmacol Biol Psychiatry. 2023;120:110645.
Prasad K, Rubin J, Mitra A, Lewis M, Theis N, Muldoon B, et al. Structural covariance networks in schizophrenia: a systematic review Part I. Schizophr Res. 2022;240:1–21.
Prasad K, Rubin J, Mitra A, Lewis M, Theis N, Muldoon B, et al. Structural covariance networks in schizophrenia: a systematic review Part II. Schizophr Res. 2022;239:176–91.
Kubera KM, Sambataro F, Vasic N, Wolf ND, Frasch K, Hirjak D, et al. Source-based morphometry of gray matter volume in patients with schizophrenia who have persistent auditory verbal hallucinations. Prog Neuropsychopharmacol Biol Psychiatry. 2014;50:102–9.
Menon B. Towards a new model of understanding - the triple network, psychopathology and the structure of the mind. Med Hypotheses. 2019;133:109385.
Menon V. Large-scale brain networks and psychopathology: a unifying triple network model. Trends Cogn Sci. 2011;15:483–506.
Supekar K, Cai W, Krishnadas R, Palaniyappan L, Menon V. Dysregulated brain dynamics in a triple-network saliency model of schizophrenia and its relation to psychosis. Biol Psychiatry. 2019;85:60–69.
Menon V, Palaniyappan L, Supekar K. Integrative brain network and salience models of psychopathology and cognitive dysfunction in schizophrenia. Biol Psychiatry. 2023;94:108–20.
Harikumar A, Solovyeva KP, Misiura M, Iraji A, Plis SM, Pearlson GD, et al. Revisiting functional dysconnectivity: a review of three model frameworks in schizophrenia. Curr Neurol Neurosci Rep. 2023;23:937–46.
Liang S, Wang Q, Greenshaw AJ, Li X, Deng W, Ren H, et al. Aberrant triple-network connectivity patterns discriminate biotypes of first-episode medication-naive schizophrenia in two large independent cohorts. Neuropsychopharmacology. 2021;46:1502–09.
Gaitonde SA, Avet C, de la Fuente Revenga M, Blondel-Tepaz E, Shahraki A, Pastor AM, et al. Pharmacological fingerprint of antipsychotic drugs at the serotonin 5-HT(2A) receptor. Mol psychiatry. 2024;29:2753–64.
Kantrowitz JT. Targeting serotonin 5-HT(2A) receptors to better treat schizophrenia: rationale and current approaches. CNS Drugs. 2020;34:947–59.
Audinot V, Newman-Tancredi A, Cussac D, Millan MJ. Inverse agonist properties of antipsychotic agents at cloned, human (h) serotonin (5-HT)(1B) and h5-HT(1D) receptors. Neuropsychopharmacology. 2001;25:410–22.
Wang HY, MacDonald ML, Borgmann-Winter KE, Banerjee A, Sleiman P, Tom A, et al. mGluR5 hypofunction is integral to glutamatergic dysregulation in schizophrenia. Mol Psychiatry. 2020;25:750–60.
Matosin N, Newell KA. Metabotropic glutamate receptor 5 in the pathology and treatment of schizophrenia. Neurosci Biobehav Rev. 2013;37:256–68.
Gray L, van den Buuse M, Scarr E, Dean B, Hannan AJ. Clozapine reverses schizophrenia-related behaviours in the metabotropic glutamate receptor 5 knockout mouse: association with N-methyl-D-aspartic acid receptor up-regulation. Int J Neuropsychopharmacol. 2009;12:45–60.
Akkus F, Treyer V, Ametamey SM, Johayem A, Buck A, Hasler G. Metabotropic glutamate receptor 5 neuroimaging in schizophrenia. Schizophr Res. 2017;183:95–101.
Ashok AH, Myers J, Reis Marques T, Rabiner EA, Howes OD. Reduced mu opioid receptor availability in schizophrenia revealed with [(11)C]-carfentanil positron emission tomographic Imaging. Nat Commun. 2019;10:4493.
Arumuham A, Nour MM, Veronese M, Onwordi EC, Rabiner EA, Howes OD. The histamine system and cognitive function: an in vivo H3 receptor PET imaging study in healthy volunteers and patients with schizophrenia. J Psychopharmacol. 2023;37:1011–22.
Coyle JT. Passing the torch: the ascendance of the glutamatergic synapse in the pathophysiology of schizophrenia. Biochem Pharm. 2024;228:116376.
Clark SD, Van Snellenberg JX, Lawson JM, Abi-Dargham A. Opioid antagonists are associated with a reduction in the symptoms of schizophrenia: a meta-analysis of controlled trials. Neuropsychopharmacology. 2020;45:1860–69.
McCutcheon RA, Cowen P, Nour MM, Pillinger T. Psychotropic taxonomies: constructing a therapeutic framework for psychiatry. Biol Psychiatry. 2024. https://doi.org/10.1016/j.biopsych.2024.12.004.
Ye N, Wang Q, Li Y, Zhen X. Current emerging therapeutic targets and clinical investigational agents for schizophrenia: challenges and opportunities. Med Res Rev. 2025;45:755–87.
Riddy DM, Cook AE, Shackleford DM, Pierce TL, Mocaer E, Mannoury la Cour C, et al. Drug-receptor kinetics and sigma-1 receptor affinity differentiate clinically evaluated histamine H(3) receptor antagonists. Neuropharmacology. 2019;144:244–55.
Hill MD, Fang H, Brown JM, Molski T, Easton A, Han X, et al. Development of 1H-Pyrazolo[3,4-b]pyridines as metabotropic glutamate receptor 5 positive allosteric modulators. ACS Med Chem Lett. 2016;7:1082–86.
Kaul I, Sawchak S, Walling DP, Tamminga CA, Breier A, Zhu H, et al. Efficacy and safety of xanomeline-trospium chloride in schizophrenia: a randomized clinical trial. JAMA Psychiatry. 2024;81:749–56.
Achtyes ED, Hopkins SC, Dedic N, Dworak H, Zeni C, Koblan K. Ulotaront: review of preliminary evidence for the efficacy and safety of a TAAR1 agonist in schizophrenia. Eur Arch Psychiatry Clin Neurosci. 2023;273:1543–56.
Rosenbrock H, Desch M, Wunderlich G. Development of the novel GlyT1 inhibitor, iclepertin (BI 425809), for the treatment of cognitive impairment associated with schizophrenia. Eur Arch Psychiatry Clin Neurosci. 2023;273:1557–66.
Lotter LD, Saberi A, Hansen JY, Misic B, Paquola C, Barker GJ, et al. Regional patterns of human cortex development correlate with underlying neurobiology. Nat Commun. 2024;15:7987.
Acknowledgements
The authors would like to express their sincere gratitude to all subjects for their time and efforts.
Funding
The study is supported by the Fundamental Research Funds for the Central Universities (2042020kf0128), Health Commission of Hubei Province scientific research project (WJ2021M142), the Medical Science Advancement Program of Wuhan University (TFLC2018001), Interdisciplinary Innovative Talents Foundation from Renmin Hospital of Wuhan University (JCRCFZ-2022-003), Hubei Provincial Science and Technology Plan Project (2023BCB133), and National Natural Science Foundation of China (82471523). L. Palaniyappan’s research is supported by the Canada First Research Excellence Fund, awarded to the Healthy Brains, Healthy Lives initiative at McGill University (through a New Investigator Supplement to LP) and Monique H. Bourgeois Chair in Developmental Disorders and the Graham Boeckh Foundation. He receives a salary award from the Fonds de recherche du Québec-Santé (FRQS 366934).This work was undertaken with the support of a China Canada High Level Medical Research Talent Fellowship for HH supervised by LP.
Author information
Authors and Affiliations
Contributions
HLW and LP designed the study. HH, WXW, XQ, RX, YX, CC, WY, YLP, HL, QRW, and HLW conducted subjects’ recruitment and performed the study. HH, LP, YZ, WXW, and XQ undertook the data analysis; HH wrote the first draft of the manuscript. WHL and LP revised the manuscript. All authors contributed to and have approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics
The authors confirm that all experiments involving human participants were performed in accordance with relevant guidelines and regulations. The Ethics Committee of Renmin Hospital of Wuhan University approved the study protocol. The written, informed consent of all subjects was obtained after receiving a complete description of the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Huang, H., Wang, X., Qin, X. et al. Distinct structural deficits in treatment-resistant schizophrenia and their putative neurotransmitter basis: a source-based morphometry analysis. Neuropsychopharmacol. 50, 1807–1816 (2025). https://doi.org/10.1038/s41386-025-02135-x
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41386-025-02135-x
This article is cited by
-
Molecular and topographic mapping of antipsychotic effects: a meta-analysis of postsynaptic density proteins in animal models with translational implications
Molecular Psychiatry (2026)
-
Intrinsic connectivity patterns of striatal subfields predict individual dimensions of psychopathology and are associated with cholinergic and serotonergic neurotransmission in schizophrenia
Neuropsychopharmacology (2026)