Abstract
Each child’s unique environment and experiences play a crucial role in shaping neurodevelopment and cognitive outcomes. Though a long history of prior research has highlighted the importance of numerous aspects of early life environments, including physical/chemical, psychosocial, socioeconomic, and cultural factors, it remains challenging to fully capture an individual’s complete set of varied exposures, experiences, and external environments (“exposome”) in a single study. The growing field of “exposomics” aims to overcome these challenges by leveraging interdisciplinary ideas and diverse methodologies to assess the additive and interactive effects of multimodal environmental features in relation to health outcomes. Here, we expand upon prior theories to describe a conceptual framework for leveraging exposomics in studies of brain health and cognitive functioning, including the outsized role of environmental influences during sensitive windows of neurodevelopmental plasticity in childhood and adolescence. We also describe current methodologies for the measurement and analysis of the exposome and suggest new ways to apply these methods in future work. Efforts to quantify the exposome in large-scale samples of youth have already begun to yield important new insights regarding environmental impacts on cognitive neurodevelopment and hold great promise for future work aiming to support healthy development in youth.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 13 print issues and online access
$259.00 per year
only $19.92 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Coscia JM, Ris MD, Succop PA, Dietrich KN. Cognitive development of lead exposed children from ages 6 to 15 years: an application of growth curve analysis. Child Neuropsychol J Norm Abnorm Dev Child Adolesc. 2003;9:10–21.
Wodtke GT, Ard K, Bullock C, White K, Priem B. Concentrated poverty, ambient air pollution, and child cognitive development. Sci Adv. 2022;8:eadd0285.
Cohodes EM, Kitt ER, Baskin-Sommers A, Gee DG. Influences of early-life stress on frontolimbic circuitry: Harnessing a dimensional approach to elucidate the effects of heterogeneity in stress exposure. Dev Psychobiol. 2021;63:153–72.
Thompson RC, Montena AL, Liu K, Watson J, Warren SL. Associations of family distress, family income, and acculturation on pediatric cognitive performance using the NIH toolbox: implications for clinical and research settings. Arch Clin Neuropsychol. 2022;37:798–813.
Gellci K, Marusak HA, Peters C, Elrahal F, Iadipaolo AS, Rabinak CA. Community and household-level socioeconomic disadvantage and functional organization of the salience and emotion network in children and adolescents. Neuroimage. 2019;184:729–40.
Meca A, Peraza JA, Riedel MC, Hale W, Pettit JW, Musser ED, et al. Acculturative orientations among Hispanic/Latinx caregivers in the ABCD study: associations with caregiver and youth mental health and youth brain function. Biol Psychiatry Glob Open Sci. 2023;3:785–96.
Wild CP. Complementing the genome with an “exposome”: the outstanding challenge of environmental exposure measurement in molecular epidemiology. Cancer Epidemiol Biomark Prev. 2005;14:1847–50.
Mirkatouli NB, Hirota S, Yoshinaga S. Thyroid cancer risk after radiation exposure in adults-systematic review and meta-analysis. J Radiat Res. 2023;64:893–903.
Vineis P, Barouki R. The exposome as the science of social-to-biological transitions. Environ Int. 2022;165:107312.
Bronfenbrenner U Ecological systems theory. In: Six theories of child development: revised formulation and current issues. London, England: Jessica Kingsley Publishers; 1992. p. 187–249.
Schulz A, Northridge ME. Social determinants of health: implications for environmental health promotion. Health Educ Behav. 2004;31:455–71.
Beech BM, Ford C, Thorpe RJ, Bruce MA, Norris KC. Poverty, racism, and the public health crisis in America. Front Public Health. 2021;9:699049.
Berry OO, Londoño Tobón A, Njoroge WFM. Social determinants of health: the impact of racism on early childhood mental health. Curr Psychiatry Rep. 2021;23:23.
Braveman P, Gottlieb L. The social determinants of health: it’s time to consider the causes of the causes. Public Health Rep. 2014;129:19–31.
Cotton NK, Shim RS. Social determinants of health, structural racism, and the impact on child and adolescent mental health. J Am Acad Child Adolesc Psychiatry. 2022;61:1385–9.
Yearby R, Lewis C, Gibson C. Incorporating structural racism, employment discrimination, and economic inequities in the social determinants of health framework to understand agricultural worker health inequities. Am J Public Health. 2023;113:S65–S71.
Xiao Y, Mann JJ, Chow JC-C, Brown TT, Snowden LR, Yip PS-F, et al. Patterns of social determinants of health and child mental health, cognition, and physical health. JAMA Pediatr. 2023;177:1294–305.
Bevel MS, Tsai M-H, Parham A, Andrzejak SE, Jones S, Moore JX. Association of food deserts and food swamps with obesity-related cancer mortality in the US. JAMA Oncol. 2023;9:909–16.
Shim RS. Dismantling structural racism in psychiatry: a path to mental health equity. Am J Psychiatry. 2021;178:592–8.
Pratap P, Dickson A, Love M, Zanoni J, Donato C, Flynn MA, et al. Public health impacts of underemployment and unemployment in the United States: exploring perceptions, gaps and opportunities. Int J Environ Res Public Health. 2021;18:10021.
Bose S, Madrigano J, Hansel NN. When health disparities hit home: redlining practices, air pollution, and asthma. Am J Respir Crit Care Med. 2022;206:803–4.
Rappaport SM. Implications of the exposome for exposure science. J Expo Sci Environ Epidemiol. 2011;21:5–9.
Gatzke-Kopp LM, Willoughby M, Kress AM, McArthur K, Wychgram C, Folch DC, et al. Airborne lead exposure and childhood cognition: the Environmental influences on Child Health Outcomes (ECHO) cohort (2003-22). Am J Public Health. 2024;114:309–18.
Marshall AT, McConnell R, Lanphear BP, Thompson WK, Herting MM, Sowell ER. Risk of lead exposure, subcortical brain structure, and cognition in a large cohort of 9- to 10-year-old children. PLoS ONE. 2021;16:e0258469.
Kim S-Y, Bechle M, Hankey S, Sheppard L, Szpiro AA, Marshall JD. Concentrations of criteria pollutants in the contiguous U.S., 1979 – 2015: role of prediction model parsimony in integrated empirical geographic regression. PLoS ONE. 2020;15:e0228535.
Chaplin TM, Mauro KL, Niehaus CE. Effects of parenting environment on child and adolescent social-emotional brain function. Curr Top Behav Neurosci. 2022;54:341–72.
Farooq B, Russell AE, Howe LD, Herbert A, Smith ADAC, Fisher HL, et al. The relationship between type, timing and duration of exposure to adverse childhood experiences and adolescent self-harm and depression: findings from three UK prospective population-based cohorts. J Child Psychol Psychiatry. 2024;65:1369–87.
McLaughlin KA, Sheridan MA, Lambert HK. Childhood adversity and neural development: deprivation and threat as distinct dimensions of early experience. Neurosci Biobehav Rev. 2014;47:578–91.
Cohodes EM, McCauley S, Pierre JC, Hodges HR, Haberman JT, Santiuste I, et al. Development and validation of the Dimensional Inventory of Stress and Trauma Across the Lifespan (DISTAL): a novel assessment tool to facilitate the dimensional study of psychobiological sequelae of exposure to adversity. Dev Psychobiol. 2023;65:e22372.
Cardenas-Iniguez C, Schachner JN, Ip KI, Schertz KE, Gonzalez MR, Abad S, et al. Building towards an adolescent neural urbanome: expanding environmental measures using linked external data (LED) in the ABCD study. Dev Cogn Neurosci. 2024;65:101338.
Kind AJH, Buckingham WR. Making neighborhood-disadvantage metrics accessible — the neighborhood atlas. N Eng J Med. 2018;378:2456–8.
Noelke C, McArdle N, DeVoe B, Leonardos M, Lu Y, Ressler RW, et al. Child Opportunity Index 3.0 Technical Documentation. diversitydatakids.org, Brandeis University. Retrieved from diversitydatakids.org/research-library/coi-30-technical-documentation. 2024.
Nilsen FM, Ruiz JDC, Tulve NS. A meta-analysis of stressors from the total environment associated with children’s general cognitive ability. Int J Environ Res Public Health. 2020;17:5451.
Bhaktaram A, Kress AM, Li Z, Knapp EA. Unpacking neighborhood socioeconomic status in children’s health research from an environmental justice perspective: a scoping review. Curr Environ Health Rep. 2024;11:288–99.
Merrick MT, Ford DC, Ports KA, Guinn AS. Prevalence of adverse childhood experiences from the 2011-2014 behavioral risk factor surveillance system in 23 states. JAMA Pediatr. 2018;172:1038–44.
Wickramaratne PJ, Yangchen T, Lepow L, Patra BG, Glicksburg B, Talati A, et al. Social connectedness as a determinant of mental health: a scoping review. PLoS ONE. 2022;17:e0275004.
Volkow ND, Koob GF, Croyle RT, Bianchi DW, Gordon JA, Koroshetz WJ, et al. The conception of the ABCD study: from substance use to a broad NIH collaboration. Dev Cogn Neurosci. 2018;32:4–7.
Moore TM, Visoki E, Argabright ST, Didomenico GE, Sotelo I, Wortzel JD, et al. Modeling environment through a general exposome factor in two independent adolescent cohorts. Exposome. 2022;2:osac010.
Bycroft C, Freeman C, Petkova D, Band G, Elliott LT, Sharp K, et al. The UK Biobank resource with deep phenotyping and genomic data. Nature. 2018;562:203–9.
Maitre L, de Bont J, Casas M, Robinson O, Aasvang GM, Agier L, et al. Human Early Life Exposome (HELIX) study: a European population-based exposome cohort. BMJ Open. 2018;8:e021311.
Guxens M, Ballester F, Espada M, Fernández MF, Grimalt JO, Ibarluzea J, et al. Cohort profile: the INMA–INfancia y Medio Ambiente–(Environment and Childhood) Project. Int J Epidemiol. 2012;41:930–40.
Cioffredi L-A, Yerby LG, Burris HH, Cole KM, Engel SM, Murray TM, et al. Assessing prenatal and early childhood social and environmental determinants of health in the HEALthy Brain and Child Development Study (HBCD). Dev Cogn Neurosci. 2024;69:101429.
Morales E, Julvez J, Torrent M, de Cid R, Guxens M, Bustamante M, et al. Association of early-life exposure to household gas appliances and indoor nitrogen dioxide with cognition and attention behavior in preschoolers. Am J Epidemiol. 2009;169:1327–36.
Robinson O, Basagaña X, Agier L, De Castro M, Hernandez-Ferrer C, Gonzalez JR, et al. The pregnancy exposome: multiple environmental exposures in the INMA-Sabadell birth cohort. Environ Sci Technol. 2015;49:10632–41.
Ibrahim FA, Mehta UM, Thekkumkara SN, Rakesh K, Swetha G, Kumar CN, et al. Multivariate associations between cognition and neighborhood geospatial characteristics in schizophrenia. Asian J Psychiatry. 2023;84:103593.
Simpson-Kent IL, Gataviņš MM, Tooley UA, Boroshok AL, McDermott CL, Park AT, et al. Multilayer network associations between the exposome and childhood brain development. bioRxiv. 2023.
Brieant A, Vannucci A, Nakua H, Harris J, Lovell J, Brundavanam D, et al. Characterizing the dimensional structure of early-life adversity in the Adolescent Brain Cognitive Development (ABCD) Study. Dev Cogn Neurosci. 2023;61:101256.
Keller AS, Moore TM, Luo A, Visoki E, Gataviņš MM, Shetty A, et al. A general exposome factor explains individual differences in functional brain network topography and cognition in youth. Dev Cogn Neurosci. 2024;66:101370.
Moore TM, Di Sandro A, Hillman N, Ruparel K, Barzilay R, Gur RE, et al. Development and public release of five continuous summary metrics for all census block-groups in the United States. PsyArXiv. 2025.
Rakesh D, McLaughlin KA, Sheridan M, Humphreys KL, Rosen ML. Environmental contributions to cognitive development: the role of cognitive stimulation. Dev Rev. 2024;73:101135.
Tooley UA, Bassett DS, Mackey AP. Environmental influences on the pace of brain development. Nat Rev Neurosci. 2021;22:372–84.
Bradley RH, Corwyn RF. Socioeconomic status and child development. Annu Rev Psychol. 2002;53:371–99.
Manalew WS, Tennekoon VS, Lee J, O’Connell B, Quinn M. Adversity in infancy and childhood cognitive development: evidence from four developing countries. Int J Public Health. 2022;67:1604503.
Pandics T, Major D, Fazekas-Pongor V, Szarvas Z, Peterfi A, Mukli P, et al. Exposome and unhealthy aging: environmental drivers from air pollution to occupational exposures. GeroScience. 2023;45:3381–408.
Luby JL, Tillman R, Barch DM. Association of timing of adverse childhood experiences and caregiver support with regionally specific brain development in adolescents. JAMA Netw Open. 2019;2:e1911426.
Yuan A, Halabicky O, Rao H, Liu J. Lifetime air pollution exposure, cognitive deficits, and brain imaging outcomes: a systematic review. Neurotoxicology. 2023;96:69–80.
Dobbins DL, Chen H, Cepeda MJ, Berenson L, Talton JW, Anderson KA, et al. Comparing impact of pesticide exposure on cognitive abilities of Latinx children from rural farmworker and urban non-farmworker families in North Carolina. Neurotoxicol Teratol. 2022;92:107106.
Lubczyńska MJ, Muetzel RL, El Marroun H, Hoek G, Kooter IM, Thomson EM, et al. Air pollution exposure during pregnancy and childhood and brain morphology in preadolescents. Environ Res. 2021;198:110446.
Papanikolaou M, Skenteris N, Piperakis SM. Effect of external classroom noise on schoolchildren’s reading and mathematics performance: correlation of noise levels and gender. Int J Adolesc Med Health. 2015;27:25–29.
Julvez J, López-Vicente M, Warembourg C, Maitre L, Philippat C, Gützkow KB, et al. Early life multiple exposures and child cognitive function: a multi-centric birth cohort study in six European countries. Environmental pollution (Barking, Essex : 1987). 2021;284:117404.
Nwobi NL, Adedapo SK, Olukolade O, Oyinlade OA, Lagunju IA, Atulomah NO, et al. Positive and inverse correlation of blood lead level with erythrocyte acetylcholinesterase and intelligence quotient in children: implications for neurotoxicity. Interdiscip Toxicol. 2019;12:136–42.
Bellinger D, Leviton A, Waternaux C, Needleman H, Rabinowitz M. Low-level lead exposure, social class, and infant development. I. Neurotoxicol Teratol. 1988;10:497–503.
Heidari S, Mostafaei S, Razazian N, Rajati M, Saeedi A, Rajati F. Correlation between lead exposure and cognitive function in 12-year-old children: a systematic review and meta-analysis. Environ Sci Pollut Res. 2021;28:43064–73.
Parithathvi A, Choudhari N, Dsouza HS. Prenatal and early life lead exposure induced neurotoxicity. Hum Exp Toxicol. 2024;43:09603271241285523.
Grippo A, Zhu K, Yeung EH, Bell EM, Bonner MR, Tian L, et al. Indoor air pollution exposure and early childhood development in the Upstate KIDS Study. Environ Res. 2023;234:116528.
Thompson R, Stewart G, Vu T, Jephcote C, Lim S, Barratt B, et al. Air pollution, traffic noise, mental health, and cognitive development: a multi-exposure longitudinal study of London adolescents in the SCAMP cohort. Environ Int. 2024;191:108963.
Beckwith T, Cecil K, Altaye M, Severs R, Wolfe C, Percy Z, et al. Reduced gray matter volume and cortical thickness associated with traffic-related air pollution in a longitudinally studied pediatric cohort. PLoS ONE. 2020;15:e0228092.
Binter A-C, Bernard JY, Mon-Williams M, Andiarena A, González-Safont L, Vafeiadi M, et al. Urban environment and cognitive and motor function in children from four European birth cohorts. Environ Int. 2022;158:106933.
Pérez-Crespo L, Kusters MSW, López-Vicente M, Lubczyńska MJ, Foraster M, White T, et al. Exposure to traffic-related air pollution and noise during pregnancy and childhood, and functional brain connectivity in preadolescents. Environ Int. 2022;164:107275.
Miller JG, Dennis EL, Heft-Neal S, Jo B, Gotlib IH. Fine particulate air pollution, early life stress, and their interactive effects on adolescent structural brain development: a longitudinal tensor-based morphometry study. Cereb Cortex. 2022;32:2156–69.
Cserbik D, Chen J-C, McConnell R, Berhane K, Sowell ER, Schwartz J, et al. Fine particulate matter exposure during childhood relates to hemispheric-specific differences in brain structure. Environ Int. 2020;143:105933.
Ramírez Benítez Y, Díaz Bringas M, Jiménez-Morales RM, Ngyah-Etchutambe IB, Pagani LS. Secondhand smoke exposure and brain health indicators in cuban preschoolers. Toxics. 2025;13:62.
Klatte M, Spilski J, Mayerl J, Möhler U, Lachmann T, Bergström K. Effects of aircraft noise on reading and quality of life in primary school children in Germany: results from the NORAH study. Environ Behav. 2017;49:390–424.
Sánchez Lizardi P, O’Rourke MK, Morris RJ. The effects of organophosphate pesticide exposure on Hispanic children’s cognitive and behavioral functioning. J Pediatr Psychol. 2008;33:91–101.
van Wendel de Joode B, Mora AM, Lindh CH, Hernández-Bonilla D, Córdoba L, Wesseling C, et al. Pesticide exposure and neurodevelopment in children aged 6–9 years from Talamanca, Costa Rica. Cortex. 2016;85:137–50.
Wade NE, McCabe CJ, Wallace AL, Gonzalez MR, Hoh E, Infante MA, et al. Clouding up cognition? Secondhand cannabis and tobacco exposure related to cognitive functioning in youth. Biol Psychiatry Glob Open Sci. 2023;3:233–42.
Fuemmeler BF, Glasgow TE, Schechter JC, Maguire R, Sheng Y, Bidopia T, et al. Prenatal and childhood smoke exposure associations with cognition, language, and attention-deficit/hyperactivity disorder. J Pediatr. 2023;256:77–84.e1.
Stansfeld S, Hygge S, Clark C, Alfred T. Night time aircraft noise exposure and children’s cognitive performance. Noise Health. 2010;12:255–62.
van Kempen E, van Kamp I, Lebret E, Lammers J, Emmen H, Stansfeld S. Neurobehavioral effects of transportation noise in primary schoolchildren: a cross-sectional study. Environ Health. 2010;9:25.
Davis EP, Korja R, Karlsson L, Glynn LM, Sandman CA, Vegetabile B, et al. Across continents and demographics, unpredictable maternal signals are associated with children’s cognitive function. EBioMedicine. 2019;46:256–63.
Cabrera NJ, Fagan J, Wight V, Schadler C. The influence of mother, father, and child risk on parenting and children’s cognitive and social behaviors. Child Dev. 2011;82:1985–2005.
Raikes H, Alexander Pan B, Luze G, Tamis-LeMonda CS, Brooks-Gunn J, Constantine J, et al. Mother–child bookreading in low-income families: correlates and outcomes during the first three years of life. Child Dev. 2006;77:924–53.
Slykerman RF, Thompson JMD, Pryor JE, Becroft DMO, Robinson E, Clark PM, et al. Maternal stress, social support and preschool children’s intelligence. Early Hum Dev. 2005;81:815–21.
Oh DL, Jerman P, Silvério Marques S, Koita K, Purewal Boparai SK, Burke Harris N, et al. Systematic review of pediatric health outcomes associated with childhood adversity. BMC Pediatr. 2018;18:83.
Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14:245–58.
Richards M, Wadsworth M. Long term effects of early adversity on cognitive function. Arch Dis Child. 2004;89:922–27.
Kalia V, Knauft K, Hayatbini N. Adverse childhood experiences (ACEs) associated with reduced cognitive flexibility in both college and community samples. PLoS ONE. 2021;16:e0260822.
Buimer EEL, Brouwer RM, Mandl RCW, Pas P, Schnack HG, Hulshoff Pol HE Adverse childhood experiences and fronto-subcortical structures in the developing brain. Front Psychiatry. 2022;13.
Fraser A, Macdonald-Wallis C, Tilling K, Boyd A, Golding J, Davey Smith G, et al. Cohort Profile: the Avon Longitudinal Study of Parents and Children: ALSPAC mothers cohort. Int J Epidemiol. 2013;42:97–110.
Nweze T, Ezenwa M, Ajaelu C, Hanson JL, Okoye C. Cognitive variations following exposure to childhood adversity: evidence from a pre-registered, longitudinal study. eClinicalMedicine. 2023;56:101784.
Sheridan MA, McLaughlin KA. Dimensions of early experience and neural development: deprivation and threat. Trends Cogn Sci. 2014;18:580–5.
McLaughlin KA, Sheridan MA. Beyond cumulative risk: a dimensional approach to childhood adversity. Curr Dir Psychol Sci. 2016;25:239–45.
Tibu F, Sheridan MA, McLaughlin KA, Nelson CA, Fox NA, Zeanah CH. Disruptions of working memory and inhibition mediate the association between exposure to institutionalization and symptoms of attention deficit hyperactivity disorder. Psychol Med. 2016;46:529–41.
Noble KG, McCandliss BD, Farah MJ. Socioeconomic gradients predict individual differences in neurocognitive abilities. Dev Sci. 2007;10:464–80.
McLaughlin KA, Sheridan MA, Gold AL, Duys A, Lambert HK, Peverill M, et al. Maltreatment exposure, brain structure, and fear conditioning in children and adolescents. Neuropsychopharmacology. 2016;41:1956–64.
Machlin L, Miller AB, Snyder J, McLaughlin KA, Sheridan MA. Differential associations of deprivation and threat With cognitive control and fear conditioning in early childhood. Front Behav Neurosci. 2019;13:80.
Carozza S, Holmes J, Astle DE. Testing deprivation and threat: a preregistered network analysis of the dimensions of early adversity. Psychol Sci. 2022;33:1753–66.
Teicher MH, Samson JA, Anderson CM, Ohashi K. The effects of childhood maltreatment on brain structure, function and connectivity. Nat Rev Neurosci. 2016;17:652–66.
Tottenham N. Human amygdala development in the absence of species-expected caregiving. Dev Psychobiol. 2012;54:598–611.
Weiss NH, Goncharenko S, Forkus SR, Ferguson JJ, Yang M. Longitudinal investigation of bidirectional relations between childhood trauma and emotion-driven impulsivity in the Adolescent Brain Cognitive Development Study. J Adolesc Health Off Publ Soc Adolesc Med. 2023;73:731–8.
Gur RE, Moore TM, Rosen AFG, Barzilay R, Roalf DR, Calkins ME, et al. Burden of environmental adversity associated with psychopathology, maturation, and brain behavior parameters in youths. JAMA Psychiatry. 2019;76:966–75.
Guerra R, Rodrigues RB, Aguiar C, Carmona M, Alexandre J, Lopes RC. School achievement and well-being of immigrant children: the role of acculturation orientations and perceived discrimination. J Sch Psychol. 2019;75:104–18.
Kiang L, Witkow MR, Thompson TL. Model minority stereotyping, perceived discrimination, and adjustment among adolescents from Asian American backgrounds. J Youth Adolesc. 2016;45:1366–79.
Chen S, Lopez-Quintero C, Elton A. Perceived racism, brain development, and internalizing and externalizing symptoms: findings from the ABCD study. J Am Acad Child Adolesc Psychiatry 2025. In Press.
Obenauf C, Ravi K, Kamper J Executive functioning task performance as predicted by linguistic and cultural factors among Latin American youth living in the USA. Arch Clin Neuropsychol Off J Natl Acad Neuropsychol 2025. In Press.
Schneider JM, Kim J, Poudel S, Lee YS, Maguire MJ. Socioeconomic status (SES) and cognitive outcomes are predicted by resting-state EEG in school-aged children. Dev Cogn Neurosci. 2024;70:101468.
Meyer OL, Harrati A, Gavett BE, Farias ST, Whitmer RA, Widaman K, et al. Effects of early life environment and adulthood SES on cognitive change in a multiethnic cohort. J Int Neuropsychol Soc JINS. 2023;29:742–50.
Petrill SA, Deater‐Deckard K. Task orientation, parental warmth and SES account for a significant proportion of the shared environmental variance in general cognitive ability in early childhood: evidence from a twin study. Dev Sci. 2004;7:25–32.
Taylor RL, Cooper SR, Jackson JJ, Barch DM. Assessment of neighborhood poverty, cognitive function, and prefrontal and hippocampal volumes in children. JAMA Netw Open. 2020;3:e2023774.
Ruiz JDC, Quackenboss JJ, Tulve NS. Contributions of a child’s built, natural, and social environments to their general cognitive ability: a systematic scoping review. PLoS ONE. 2016;11:e0147741.
Meredith WJ, Cardenas-Iniguez C, Berman MG, Rosenberg MD. Effects of the physical and social environment on youth cognitive performance. Dev Psychobiol. 2022;64:e22258.
Juvrud J, Haas SA, Lindskog M, Astor K, Namgyel SC, Wangmo T, et al. High quality social environment buffers infants’ cognitive development from poor maternal mental health: evidence from a study in Bhutan. Dev Sci. 2022;25:e13203.
Gartland D, Riggs E, Muyeen S, Giallo R, Afifi TO, MacMillan H, et al. What factors are associated with resilient outcomes in children exposed to social adversity? A systematic review. BMJ Open. 2019;9:e024870.
Ku BS, Aberizk K, Feurer C, Yuan Q, Druss BG, Jeste DV, et al. Aspects of Area Deprivation Index in relation to hippocampal volume among children. JAMA Netw Open. 2024;7:e2416484.
Rakesh D, Whittle S. Socioeconomic status and the developing brain – A systematic review of neuroimaging findings in youth. Neurosci Biobehav Rev. 2021;130:379–407.
Hackman DA, Farah MJ. Socioeconomic status and the developing brain. Trends Cogn Sci. 2009;13:65–73.
Weissman DG, Hatzenbuehler ML, Cikara M, Barch DM, McLaughlin KA. State-level macro-economic factors moderate the association of low income with brain structure and mental health in U.S. children. Nat Commun. 2023;14:2085.
Noble KG, Houston SM, Brito NH, Bartsch H, Kan E, Kuperman JM, et al. Family income, parental education and brain structure in children and adolescents. Nat Neurosci. 2015;18:773–8.
Zhao S, Su H, Cong J, Wen X, Yang H, Chen P, et al. Hierarchical individual variation and socioeconomic impact on personalized functional network topography in children. BMC Med. 2024;22:556.
Gornik AE, Jacobson LA, Kalb LG, Pritchard AE. If opportunity knocks: understanding contextual factors’ influence on cognitive systems. Res Child Adolesc Psychopathol. 2024;52:521–33.
Cui Z, Li H, Xia CH, Larsen B, Adebimpe A, Baum GL, et al. Individual variation in functional topography of association networks in youth. Neuron. 2020;106:340–353.e8.
Tao C, Li Z, Fan Y, Huang Y, Wan T, Shu M, et al. Estimating lead-attributable mortality burden by socioeconomic status in the USA. Int J Epidemiol. 2024;53:dyae089.
Rakesh D, Zalesky A, Whittle S. Assessment of parent income and education, neighborhood disadvantage, and child brain structure. JAMA Netw Open. 2022;5:e2226208.
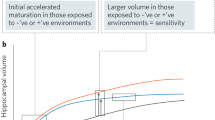
Larsen B, Sydnor VJ, Keller AS, Yeo BTT, Satterthwaite TD. A critical period plasticity framework for the sensorimotor–association axis of cortical neurodevelopment. Trends Neurosci. 2023;46:847–62.
Sydnor VJ, Larsen B, Bassett DS, Alexander-Bloch A, Fair DA, Liston C, et al. Neurodevelopment of the association cortices: patterns, mechanisms, and implications for psychopathology. Neuron. 2021;109:2820–46.
Sisk LM, Gee DG. Stress and adolescence: vulnerability and opportunity during a sensitive window of development. Curr Opin Psychol. 2022;44:286–92.
Keller AS, Pines AR, Shanmugan S, Sydnor VJ, Cui Z, Bertolero MA, et al. Personalized functional brain network topography is associated with individual differences in youth cognition. Nat Commun. 2023;14:8411.
Shanmugan S, Seidlitz J, Cui Z, Adebimpe A, Bassett DS, Bertolero MA, et al. Sex differences in the functional topography of association networks in youth. Proc Natl Acad Sci. 2022;119:e2110416119.
Larsen B, Luna B. Adolescence as a neurobiological critical period for the development of higher-order cognition. Neurosci Biobehav Rev. 2018;94:179–95.
Somerville LH, Jones RM, Ruberry EJ, Dyke JP, Glover G, Casey B. Medial prefrontal cortex and the emergence of self-conscious emotion in adolescence. Psychol Sci. 2013;24:1554–62.
Rakesh D, Whittle S, Sheridan MA, McLaughlin KA. Childhood socioeconomic status and the pace of structural neurodevelopment: accelerated, delayed, or simply different? Trends Cogn Sci. 2023;27:833–51.
Jenkins LM, Chiang JJ, Vause K, Hoffer L, Alpert K, Parrish TB, et al. Subcortical structural variations associated with low socioeconomic status in adolescents. Hum Brain Mapp. 2020;41:162–71.
Callaghan BL, Tottenham N. The Stress Acceleration Hypothesis: effects of early-life adversity on emotion circuits and behavior. Curr Opin Behav Sci. 2016;7:76–81.
Herzberg MP, McKenzie KJ, Hodel AS, Hunt RH, Mueller BA, Gunnar MR, et al. Accelerated maturation in functional connectivity following early life stress: circuit specific or broadly distributed? Dev Cogn Neurosci. 2021;48:100922.
Colich NL, Rosen ML, Williams ES, McLaughlin KA. Biological aging in childhood and adolescence following experiences of threat and deprivation: a systematic review and meta-analysis. Psychol Bull. 2020;146:721–64.
McLaughlin KA, Sheridan MA, Humphreys KL, Belsky J, Ellis BJ. The value of dimensional models of early experience: thinking clearly about concepts and categories. Perspect Psychol Sci. 2021;16:1463–72.
Roubinov D, Meaney MJ, Boyce WT. Change of pace: how developmental tempo varies to accommodate failed provision of early needs. Neurosci Biobehav Rev. 2021;131:120–34.
McLaughlin KA, Sheridan MA, Nelson CA. Neglect as a violation of species-expectant experience: neurodevelopmental consequences. Biol Psychiatry. 2017;82:462–71.
Ellis BJ, Sheridan MA, Belsky J, McLaughlin KA. Why and how does early adversity influence development? Toward an integrated model of dimensions of environmental experience. Dev Psychopathol. 2022;34:447–71.
Firestone M, Moya J, Cohen‐Hubal E, Zartarian V, Xue J. Identifying childhood age groups for exposure assessments and monitoring. Risk Anal. 2007;27:701–14.
Persson Waye K, Löve J, Lercher P, Dzhambov AM, Klatte M, Schreckenberg D, et al. Adopting a child perspective for exposome research on mental health and cognitive development - Conceptualisation and opportunities. Environ Res. 2023;239:117279.
Rudolph KD, Skymba HV, Modi HH, Davis MM, Sze WY, Rosswurm CP, et al. How does peer adversity “get inside the brain?” adolescent girls’ differential susceptibility to neural dysregulation of emotion following victimization. Dev Psychobiol. 2021;63:481–95.
Harkness KL, Bruce AE, Lumley MN. The role of childhood abuse and neglect in the sensitization to stressful life events in adolescent depression. J Abnorm Psychol. 2006;115:730–41.
Marek S, Tervo-Clemmens B, Calabro FJ, Montez DF, Kay BP, Hatoum AS, et al. Reproducible brain-wide association studies require thousands of individuals. Nature. 2022;603:654–60.
Tervo-Clemmens B, Marek S, Barch DM. Tailoring psychiatric neuroimaging to translational goals. JAMA Psychiatry. 2023;80:765–6.
Kalisch R, Cramer AOJ, Binder H, Fritz J, Leertouwer I, Lunansky G, et al. Deconstructing and reconstructing resilience: a dynamic network approach. Perspectives on psychological science : a journal of the Association for Psychological Science. 2019;14:765–77.
Shaw R, Pengelly C, Crinnin C, Amina E, Wutz AV, King PR. Scoping review of the role of social support in women Veterans’ psychosocial and health outcomes. J Women Aging. 2024;36:450–74.
Höltge J, Theron L, van Rensburg A, Cowden RG, Govender K, Ungar M. Investigating the interrelations between systems of support in 13- to 18-year-old adolescents: a network analysis of resilience promoting systems in a high and middle-income country. Child Dev. 2021;92:586–99.
Ellis BJ, Abrams LS, Masten AS, Sternberg RJ, Tottenham N, Frankenhuis WE. Hidden talents in harsh environments. Dev Psychopathol. 2022;34:95–113.
Zundel CG, Ryan P, Brokamp C, Heeter A, Huang Y, Strawn JR, et al. Air pollution, depressive and anxiety disorders, and brain effects: a systematic review. Neurotoxicology. 2022;93:272–300.
Evans GW. The built environment and mental health. J Urban Health Bull N Y Acad Med. 2003;80:536–55.
Chou T, Asnaani A, Hofmann SG. Perception of racial discrimination and psychopathology across three U.S. ethnic minority groups. Cult Divers Ethn Minor Psychol. 2012;18:74–81.
Hahad O, Al-Kindi S, Lelieveld J, Münzel T, Daiber A. Supporting and implementing the beneficial parts of the exposome: the environment can be the problem, but it can also be the solution. Int J Hyg Environ Health. 2024;255:114290.
Troller-Renfree SV, Costanzo MA, Duncan GJ, Magnuson K, Gennetian LA, Yoshikawa H, et al. The impact of a poverty reduction intervention on infant brain activity. Proc Natl Acad Sci. 2022;119:e2115649119.
Upadhyay RP, Taneja S, Chowdhury R, Dhabhai N, Sapra S, Mazumder S, et al. Child neurodevelopment after multidomain interventions from preconception through early childhood: the WINGS randomized clinical trial. JAMA. 2024;331:28.
Collins-Anderson A, Vahedi L, Hutson W, Hudson D. Intersectionality and mental health among emerging adult Black American men: a scoping review. Curr Psychiatry Rep. 2022;24:819–30.
Cecil KM, Brubaker CJ, Adler CM, Dietrich KN, Altaye M, Egelhoff JC, et al. Decreased brain volume in adults with childhood lead exposure. PLoS Med. 2008;5:e112.
Mohamed NN, Loy SL, Lim PY, Al Mamun A, Jan Mohamed HJ. Early life secondhand smoke exposure assessed by hair nicotine biomarker may reduce children’s neurodevelopment at 2 years of age. Sci Total Environ. 2018;610-1:147–53.
El Marroun H, Schmidt MN, Franken IHA, Jaddoe VWV, Hofman A, van der Lugt A, et al. Prenatal tobacco exposure and brain morphology: a prospective study in young children. Neuropsychopharmacol Publ Am Coll Neuropsychopharmacol. 2014;39:792–800.
Gong W, Rolls ET, Du J, Feng J, Cheng W. Brain structure is linked to the association between family environment and behavioral problems in children in the ABCD study. Nat Commun. 2021;12:3769.
Hong S-J, Sisk LM, Caballero C, Mekhanik A, Roy AK, Milham MP, et al. Decomposing complex links between the childhood environment and brain structure in school-aged youth. Dev Cogn Neurosci. 2021;48:100919.
Kishiyama MM, Boyce WT, Jimenez AM, Perry LM, Knight RT. Socioeconomic disparities affect prefrontal function in children. J Cogn Neurosci. 2009;21:1106–15.
Ramphal B, Whalen DJ, Kenley JK, Yu Q, Smyser CD, Rogers CE, et al. Brain connectivity and socioeconomic status at birth and externalizing symptoms at age 2 years. Dev Cogn Neurosci. 2020;45:100811.
Elansary M, Wei WS, Pierce LJ, McCoy DC, Nelson CA. Association of neighborhood opportunity with infant brain activity and cognitive development. J Dev Behav Pediatr. 2024;45:e217–e224.
Zhi D, Jiang R, Pearlson G, Fu Z, Qi S, Yan W, et al. Triple interactions between the environment, brain, and behavior in children: an ABCD study. Biol Psychiatry. 2024;95:828–38.
Acknowledgements
Funding for this work was provided by a NARSAD Young Investigator Award from the Brain and Behavior Research Foundation (ASK) and the National Institute of Mental Health (1L30MH131061-01; ASK).
Author information
Authors and Affiliations
Contributions
HR and ASK formulated the topic and the main idea. HR, ND and NK conducted the review of literature material. HR wrote the initial draft. AW designed all schematics. HR, ND, RB, AW, NK and ASK revised the manuscript. All authors contributed to the final draft.
Corresponding author
Ethics declarations
Competing interests
RB reports owning stock in Taliaz Health and serving on the scientific boards of Taliaz Health outside the submitted work. All other authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Robinson, H., Dave, N., Barzilay, R. et al. The effect of the “exposome” on developmental brain health and cognitive outcomes. Neuropsychopharmacol. 51, 169–184 (2026). https://doi.org/10.1038/s41386-025-02180-6
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41386-025-02180-6
This article is cited by
-
Integrated assessment of environmental infrastructural and social risks for urban public safety
Scientific Reports (2026)
-
Trajectories of mental health and mental illness: where we are now and where we go next
Neuropsychopharmacology (2026)
-
The puzzle of heterogeneity: an introduction to part II
Neuropsychopharmacology (2026)
-
The PAthways to Resilience And Mental health (PARAM) project: protocol for a multi-site developmental cohort in India
BMC Psychiatry (2025)