Abstract
Migraine is a debilitating neurological disorder with significant impact on quality of life, including social functioning. This study investigated the effects of nitroglycerin (NTG)-induced migraine in male and female mice on social behavior and neuronal activation and explored the therapeutic potential of nociceptin opioid peptide (NOP) receptor agonism. We found that acute NTG administration induced mechanical allodynia in periorbital region and paw as well as impaired social behavior in both sexes, albeit with sex-specific patterns. The NOP receptor agonist, Ro 64-6198, reversed both the allodynia and social deficits induced by NTG. The reversal of social impairment elicited by Ro 64-6198 was partially blocked by the NOP receptor antagonist, SB-612111, confirming NOP receptor-mediated action. Using TRAP2/Ai9 transgenic mice, we demonstrated that NTG induced significant neuronal activation in brain regions associated with pain and social behavior, including the anterior cingulate cortex, amygdala, hippocampus, hypothalamus, and periaqueductal gray (in female mice) as well as trigeminal nucleus caudalis (TNC) in male and female mice. Consistent with the behavioral results, NTG-induced neuronal activation in these brain regions was significantly reduced in the presence of Ro 64-6198. Our findings provide further evidence for the involvement of the NOP system in migraine pathophysiology, particularly social aspects that are indirectly pain-related symptoms, and provide a direct correlation with neuronal activation in several brain regions.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 13 print issues and online access
$259.00 per year
only $19.92 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
Data are available via Repository for Open Data “RepOD” (https://doi.org/10.18150/JCTHAV) at the Interdisciplinary Centre for Mathematical and Computational Modelling, University of Warsaw.
References
Stovner LJ, Hagen K, Linde M, Steiner TJ. The global prevalence of headache: an update, with analysis of the influences of methodological factors on prevalence estimates. J Headache Pain. 2022;23:34.
Storer RJ, Akerman S, Goadsby PJ. Characterization of opioid receptors that modulate nociceptive neurotransmission in the trigeminocervical complex. Br J Pharmacol. 2003;138:317–24.
Tepper SJ. Opioids should not be used in migraine. Headache. 2012;52:30–34.
Pradhan AA, Smith ML, Zyuzin J, Charles A. δ-Opioid receptor agonists inhibit migraine-related hyperalgesia, aversive state and cortical spreading depression in mice. Br J Pharmacol. 2014;171:2375–84.
Abdallah K, Gendron L. The delta opioid receptor in pain control. Handb Exp Pharmacol. 2018;247:147–77.
Burks K. Intravenous acetaminophen reduces opioid use for postoperative pain in obese patients undergoing laparoscopic cholecystectomy. Doctoral dissertation. University of Southern Mississippi; 2015.
Parker KE, Sugiarto E, Taylor AMW, Pradhan AA, Al-Hasani R. Pain, motivation, migraine, and the microbiome: new frontiers for opioid systems and disease. Mol Pharmacol. 2020;98:433–44.
Neal CR, Mansour A, Reinscheid R, Nothacker H-P, Civelli O, Akil H, et al. Opioid receptor-like (ORL1) receptor distribution in the rat central nervous system: comparison of ORL1 receptor mRNA expression with125I-[14Tyr]-orphanin FQ binding. J Comp Neurol. 1999;412:563–605.
Targowska-Duda KM, Ozawa A, Bertels Z, Cippitelli A, Marcus JL, Mielke-Maday HK, et al. NOP receptor agonist attenuates nitroglycerin-induced migraine-like symptoms in mice. Neuropharmacology. 2020;170:108029.
El Daibani A, Che T. Spotlight on nociceptin/orphanin FQ receptor in the treatment of pain. Molecules. 2022;27:595.
Lambert GA, Donaldson C, Boers PM, Zagami AS. Activation of trigeminovascular neurons by glyceryl trinitrate. Brain Res. 2000;887:203–10.
Borsook D, Maleki N, Burstein RM. Migraine. In: Zigmond MJ, Rowland LP, Coyle JT. Neurobiology of brain disorders. San Diego: Academic Press; 2015. p. 693–708.
Pourrahimi AM, Abbasnejad M, Raoof M, Esmaeili-Mahani S, Kooshki R. The involvement of orexin 1 and cannabinoid 1 receptors within the ventrolateral periaqueductal gray matter in the modulation of migraine-induced anxiety and social behavior deficits of rats. Peptides. 2021;146:170651.
Snoer AH, Høst C, Dømgaard M, Hansen JM. Frequent or chronic migraine negatively impacts personal, social and professional life. Dan Med J. 2021, 68:A08200592.
Noseda R, Burstein R. Migraine pathophysiology: anatomy of the trigeminovascular pathway and associated neurological symptoms, cortical spreading depression, sensitization, and modulation of pain. Pain. 2013;154:S44–S53.
Yücel Y. Effects of retinal ganglion cell loss on magno-, parvo-, koniocellular pathways in the lateral geniculate nucleus and visual cortex in glaucoma. Prog Retin Eye Res. 2003;22:465–81.
Öhman A. The role of the amygdala in human fear: automatic detection of threat. Psychoneuroendocrinology. 2005;30:953–8.
Christensen S, Petersen S, Sørensen DB, Olesen J, Jansen-Olesen I. Cilostazol induces C-fos expression in the trigeminal nucleus caudalis and behavioural changes suggestive of headache with the migraine-like feature photophobia in female rats. Cephalalgia. 2018;38:452–65.
Wu S, Ren X, Zhu C, Wang W, Zhang K, Li Z, et al. A c-Fos activation map in nitroglycerin/levcromakalim-induced models of migraine. J Headache Pain. 2022;23:128.
Knyihár-Csillik E, Tajti J, Samsam M, Sáry G, Buzás P, Vécsei L. Depletion of calcitonin gene-related peptide from the caudal trigeminal nucleus of the rat after electrical stimulation of the Gasserian ganglion. Exp Brain Res. 1998;118:111–4.
Harris JA, Hirokawa KE, Sorensen SA, Gu H, Mills M, Ng LL, et al. Anatomical characterization of Cre driver mice for neural circuit mapping and manipulation. Front Neural Circuits. 2014;8:76.
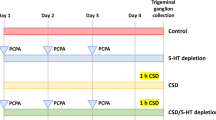
Targowska-Duda KM, Peters D, Marcus JL, Zribi G, Toll L, Ozawa A. Functional and anatomical analyses of active spinal circuits in a mouse model of chronic pain. Pain. 2024;165:685.
Allen WE, DeNardo LA, Chen MZ, Liu CD, Loh KM, Fenno LE, et al. Thirst-associated preoptic neurons encode an aversive motivational drive. Science. 2017;357:1149–55.
Corder G, Ahanonu B, Grewe BF, Wang D, Schnitzer MJ, Scherrer G. An amygdalar neural ensemble that encodes the unpleasantness of pain. Science. 2019;363:276–81.
Guenthner CJ, Miyamichi K, Yang HH, Heller HC, Luo L. Permanent genetic access to transiently active neurons via TRAP: targeted recombination in active populations. Neuron. 2013;78:773–84.
DeNardo LA, Liu CD, Allen WE, Adams EL, Friedmann D, Fu L, et al. Temporal evolution of cortical ensembles promoting remote memory retrieval. Nat Neurosci. 2019;22:460–9.
Stirling DR, Swain-Bowden MJ, Lucas AM, Carpenter AE, Cimini BA, Goodman A. CellProfiler 4: improvements in speed, utility and usability. BMC Bioinform. 2021;22:433.
Schindelin J, Arganda-Carreras I, Frise E, Kaynig V, Longair M, Pietzsch T, et al. Fiji: an open-source platform for biological-image analysis. Nat Methods. 2012;9:676–82.
De Logu F, Landini L, Janal MN, Li Puma S, De Cesaris F, Geppetti P, et al. Migraine-provoking substances evoke periorbital allodynia in mice. J Headache Pain. 2019;20:18.
Chaplan SR, Bach FW, Pogrel JW, Chung JM, Yaksh TL. Quantitative assessment of tactile allodynia in the rat paw. J Neurosci Methods. 1994;53:55–63.
Jabarin R, Netser S, Wagner S. Beyond the three-chamber test: toward a multimodal and objective assessment of social behavior in rodents. Mol Autism. 2022;13:41.
Bates E, Nikai T, Brennan K, Fu Y-H, Charles A, Basbaum A, et al. Sumatriptan alleviates nitroglycerin-induced mechanical and thermal allodynia in mice. Cephalalgia. 2010;30:170–8.
Kaufmann D, Brennan KC. The effects of chronic stress on migraine relevant phenotypes in male mice. Front Cell Neurosci. 2018;12:294.
Ratcliffe GE, Enns MW, Jacobi F, Belik S-L, Sareen J. The relationship between migraine and mental disorders in a population-based sample. Gen Hosp Psychiatry. 2009;31:14–19.
Hoffmann J, Charles A. Glutamate and its receptors as therapeutic targets for migraine. Neurotherapeutics. 2018;15:361–70.
Stamford JA. Descending control of pain. Br J Anaesth. 1995;75:217–27.
Hughes EM, Calcagno P, Sanchez C, Smith K, Kelly JP, Finn DP, et al. Mu-opioid receptor agonism differentially alters social behaviour and immediate early gene expression in male adolescent rats prenatally exposed to valproic acid versus controls. Brain Res Bull. 2021;174:260–7.
Ramachandran R, Bhatt DK, Ploug KB, Olesen J, Jansen-Olesen I, Hay-Schmidt A, et al. A naturalistic glyceryl trinitrate infusion migraine model in the rat. Cephalalgia. 2012;32:73–84.
Tassorelli C, Joseph SA. Systemic nitroglycerin induces Fos immunoreactivity in brainstem and forebrain structures of the rat. Brain Res. 1995;682:167–81.
Kagan R, Kainz V, Burstein R, Noseda R. Hypothalamic and basal ganglia projections to the posterior thalamus: Possible role in modulation of migraine headache and photophobia. Neuroscience. 2013;248:359–68.
Chen Z, Chen X, Liu M, Dong Z, Ma L, Yu S. Altered functional connectivity of amygdala underlying the neuromechanism of migraine pathogenesis. J Headache Pain. 2017;18:7.
Hadjikhani N, Ward N, Boshyan J, Napadow V, Maeda Y, Truini A, et al. The missing link: enhanced functional connectivity between amygdala and visceroceptive cortex in migraine. Cephalalgia. 2013;33:1264–8.
Acknowledgements
We thank the Nikon Center of Excellence at the Florida Atlantic University, Stiles-Nicholson Brain Institute for the use of the microscope. In addition, we want to thank all the husbandry and veterinary staff for the care of our animal subjects at the Medical University of Lublin (Experimental Medicine Center) and the Florida Atlantic University.
Funding
This work was supported by grant from the Polish National Science Center (SONATA BIS 11 funding 2021/42/E/NZ7/00191) to KMT-D; NIH grant (R34NS121875) to AO, and DoD grant (W81XWH2110410) to LT. AM.’s internship at Florida Atlantic University was funded by SONATA BIS 11.
Author information
Authors and Affiliations
Contributions
All of the authors listed in this manuscript have read the final version of the manuscript. The contributions of each author are: KMT-D, AO, and LT designed the study; AM, OW-D, MM, DP, IS, D.P-M and KMT-D performed experiments; AM, KMT-D, OW-D, AO and M. Maj analyzed data. AM, KMT-D, AO and LT wrote the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
41386_2025_2187_MOESM1_ESM.docx
Table S1 Statistical analysis for all treatments with reference to total time spent in chamber with familiar and non-familiar mice, and after sumatriptan co-injection with NTG using social test
41386_2025_2187_MOESM2_ESM.docx
Table S2 Statistical values for neuronal activation with treatment in various brain regions in male and female TRAP2/Ai9 mice
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mudgal, A., Wronikowska-Denysiuk, O., Martinez, M. et al. Ro 64-6198, a selective NOP receptor agonist attenuates social impairments associated with NTG-induced migraine pain. Neuropsychopharmacol. (2025). https://doi.org/10.1038/s41386-025-02187-z
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41386-025-02187-z