Abstract
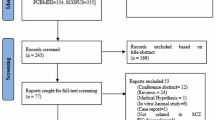
The high energy demand of the human brain obligates robust mitochondrial energy metabolism, while mitochondrial dysfunctions have been linked to neuropsychiatric disorders, including schizophrenia spectrum disorders (SSD). However, in vivo assessments that can directly inform brain mitochondrial functioning and its etiopathophysiological path to SSD remain difficult to obtain. We hypothesized that system and brain mitochondrial dysfunctions in SSD may be indexed by elevated cell-free mitochondrial DNA (cf-mtDNA) levels in the blood and in neuronal extracellular vesicles (nEVs). We also explored if these mtDNA marker elevations were associated with brain metabolites as measured by magnetic resonance spectroscopy (MRS). We examined blood cf-mtDNA in 58 SSD patients and 33 healthy controls, followed by assessing nEV mtDNA and metabolite levels using MRS in a subgroup of patients and controls. We found that people with SSD had significantly elevated cf-mtDNA levels in both the blood (p = 0.0002) and neuronal EVs (p = 0.003) compared to controls. These mtDNA abnormalities can be linked back to brain lactate+ levels such that higher blood and nEV mtDNA levels were significantly associated with higher lactate+ levels measured at the anterior cingulate cortex (r = 0.53, 0.53; p = 0.008, 0.03, respectively) in SSD patients. Furthermore, higher developmental stress and trauma were significantly associated with higher cf-mtDNA levels in both the blood and neuronal EVs in SSD patients (r = 0.29, 0.49; p = 0.01, 0.03, respectively). In conclusion, if replicated and fully developed, blood and neuronal EV-based cell-free mtDNA may provide a clinically accessible biomarker to more directly evaluate the mitochondrial hypothesis and the abnormal bioenergetics pathways in schizophrenia.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 13 print issues and online access
$259.00 per year
only $19.92 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
The datasets generated and analyzed here are currently not publicly available, but we will strive to honor data request on case-by-case basis.
References
Whatley SA, Curti D, Marchbanks RM. Mitochondrial involvement in schizophrenia and other functional psychoses. Neurochem Res. 1996;21:995–1004.
Srivastava R, Faust T, Ramos A, Ishizuka K, Sawa A. Dynamic changes of the mitochondria in psychiatric illnesses: new mechanistic insights from human neuronal models. Biol Psychiatry. 2018;83:751–60.
Whitehurst T, Howes O. The role of mitochondria in the pathophysiology of schizophrenia: a critical review of the evidence focusing on mitochondrial complex one. Neurosci Biobehav Rev. 2022;132:449–64.
Chouinard V-A, Du F, Chen X, Tusuzian E, Ren B, Anderson J, et al. Cognitive impairment in psychotic disorders is associated with brain reductive stress and impaired energy metabolism as measured by 31P Magnetic Resonance Spectroscopy. Schizophr Bull. 2025:sbaf003. https://doi.org/10.1093/schbul/sbaf003.
Du F, Cooper AJ, Thida T, Sehovic S, Lukas SE, Cohen BM, et al. In Vivo Evidence for cerebral bioenergetic abnormalities in schizophrenia measured using 31p magnetization transfer spectroscopy. JAMA Psychiatry. 2014;71:19–27.
Roberts RC. Mitochondrial dysfunction in schizophrenia: With a focus on postmortem studies. Mitochondrion. 2021;56:91–101.
DiMauro S, Schon EA. Mitochondrial respiratory-chain diseases. New Engl J Med. 2003;348:2656–68.
Rollins B, Martin MV, Sequeira PA, Moon EA, Morgan LZ, Watson SJ, et al. Mitochondrial variants in schizophrenia, bipolar disorder, and major depressive disorder. PLoS One. 2009;4:e4913.
Bulduk BK, Tortajada J, Valiente-Pallejà A, Callado LF, Torrell H, Vilella E, et al. High number of mitochondrial DNA alterations in postmortem brain tissue of patients with schizophrenia compared to healthy controls. Psychiatry Res. 2024;337:115928.
Kumar P, Efstathopoulos P, Millischer V, Olsson E, Wei YBin, Brüstle O, et al. Mitochondrial DNA copy number is associated with psychosis severity and anti-psychotic treatment. Sci Rep. 2018;8:12743.
Verge B, Alonso Y, Valero J, Miralles C, Vilella E, Martorell L. Mitochondrial DNA (mtDNA) and schizophrenia. European Psychiatry. 2011;26:45–56.
Robicsek O, Karry R, Petit I, Salman-Kesner N, Müller FJ, Klein E, et al. Abnormal neuronal differentiation and mitochondrial dysfunction in hair follicle-derived induced pluripotent stem cells of schizophrenia patients. Mol Psychiatry. 2013;18:1067–76.
Bertholet AM, Delerue T, Millet AM, Moulis MF, David C, Daloyau M, et al. Mitochondrial fusion/fission dynamics in neurodegeneration and neuronal plasticity. Neurobiol Dis. 2016;90:3–19.
Shi R, Guberman M, Kirshenbaum LA. Mitochondrial quality control: the role of mitophagy in aging. Trends Cardiovasc Med. 2018;28:246–60.
Stephens OR, Grant D, Frimel M, Wanner N, Yin M, Willard B, et al. Characterization and origins of cell-free mitochondria in healthy murine and human blood. Mitochondrion. 2020;54:102–12.
Stier A. Human blood contains circulating cell-free mitochondria, but are they really functional?. American J Physiol-Endocrinol Metab. 2021;320:E859–E863.
Pérez-Treviño P, Velásquez M, García N. Mechanisms of mitochondrial DNA escape and its relationship with different metabolic diseases. Biochimica et Biophys. Acta (BBA) - Mol Basis Dis. 2020;1866:165761.
García-De La Cruz DD, Juárez-Rojop IE, Tovilla-Zárate CA, Martínez-Magaña JJ, Genis-Mendoza AD, Nicolini H, et al. Association between mitochondrial DNA and cognitive impairment in schizophrenia: Study protocol for a Mexican population. Neuropsychiatr Dis Treat. 2019;15:1717–22.
Li S, Jiang J, Zhu W, Wang D, Dong C, Bu Y, et al. Increased cell-free DNA is associated with oxidative damage in patients with schizophrenia. J Psychiatr Res. 2024;175:20–28.
Ouyang H, Huang M, Xu Y, Yao Q, Wu X, Zhou D. Reduced cell-free mitochondrial DNA levels were induced by antipsychotics treatment in first-episode patients with schizophrenia. Front Psychiatry. 2021;12:652314.
Yáñez-Mó M, Siljander PR-M, Andreu Z, Bedina Zavec A, Borràs FE, Buzas EI, et al. Biological properties of extracellular vesicles and their physiological functions. J Extracell Vesicles. 2015;4:27066.
Xue T, Liu W, Wang L, Shi Y, Hu Y, Yang J, et al. Extracellular vesicle biomarkers for complement dysfunction in schizophrenia. Brain. 2024;147:1075–86.
Melentijevic I, Toth ML, Arnold ML, Guasp RJ, Harinath J, Nguyen KC, et al. C. Elegans neurons jettison protein aggregates and mitochondria under neurotoxic stress. Nature. 2017;542:367–71.
Goetzl EJ, Srihari VH, Guloksuz S, Ferrara M, Tek C, Heninger GR. Neural cell-derived plasma exosome protein abnormalities implicate mitochondrial impairment in first episodes of psychosis. FASEB J. 2021;35:e21339.
Benarroch E. What Is the role of lactate in brain metabolism, plasticity, and neurodegeneration?. Neurology. 2024;102:e209378.
Karagiannis A, Gallopin T, Lacroix A, Plaisier F, Piquet J, Geoffroy H, et al. Lactate is an energy substrate for rodent cortical neurons and enhances their firing activity. 2021. 2021. https://doi.org/10.7554/eLife.
Chiappelli J, Savransky A, Ma Y, Gao S, Kvarta MD, Kochunov P, et al. Impact of lifetime stressor exposure on neuroenergetics in schizophrenia spectrum disorders. Schizophr Res. 2024;269:58–63.
Dogan AE, Yuksel C, Du F, Chouinard VA, Öngür D. Brain lactate and pH in schizophrenia and bipolar disorder: A systematic review of findings from magnetic resonance studies. Neuropsychopharmacology. 2018;43:1681–90.
Rowland LM, Pradhan S, Korenic S, Wijtenburg SA, Hong LE, Edden RA, et al. Elevated brain lactate in schizophrenia: A 7T magnetic resonance spectroscopy study. Transl Psychiatry. 2016;6,e967.
Liu S, Zhang L, Fan X, Wang G, Liu Q, Yang Y, et al. Lactate levels in the brain and blood of schizophrenia patients: A systematic review and meta-analysis. Schizophr Res. 2024;264:29–38.
Sullivan CR, Mielnik CA, Funk A, O’Donovan SM, Bentea E, Pletnikov M, et al. Measurement of lactate levels in postmortem brain, iPSCs, and animal models of schizophrenia. Sci Rep. 2019;9,5087.
Nugent KL, Chiappelli J, Rowland LM, Daughters SB, Hong LE. Distress intolerance and clinical functioning in persons with schizophrenia. Psychiatry Res. 2014;220:31–36.
Da Silva T, Wu A, Laksono I, Prce I, Maheandiran M, Kiang M, et al. Mitochondrial function in individuals at clinical high risk for psychosis. Sci Rep. 2018;8,6216.
Roberts RC, Barksdale KA, Roche JK, Lahti AC. Decreased synaptic and mitochondrial density in the postmortem anterior cingulate cortex in schizophrenia. Schizophr Res. 2015;168:543–53.
Akter M, Hasan M, Ramkrishnan AS, Iqbal Z, Zheng X, Fu Z, et al. Astrocyte and L-lactate in the anterior cingulate cortex modulate schema memory and neuronal mitochondrial biogenesis. Elife. 2023;12:e85751.
Zemirli N, Morel E, Molino D. Mitochondrial dynamics in basal and stressful conditions. Int J Mol Sci. 2018;19:564.
Picard M, McEwen BS. Psychological stress and mitochondria: a conceptual framework. Biopsychosocial Sci Med. 2018;80:126–40.
Van Os J, Selten J-P. Prenatal exposure to maternal stress and subsequent schizophrenia: the May 1940 invasion of the Netherlands. British J Psychiatry. 1998;172:324–6.
Khashan AS, Abel KM, McNamee R, Pedersen MG, Webb RT, Baker PN, et al. Higher risk of offspring schizophrenia following antenatal maternal exposure to severe adverse life events. Arch Gen Psychiatry. 2008;65:146–52.
Varese F, Smeets F, Drukker M, Lieverse R, Lataster T, Viechtbauer W, et al. Childhood adversities increase the risk of psychosis: a meta-analysis of patient-control, prospective-and cross-sectional cohort studies. Schizophr Bull. 2012;38:661–71.
Docherty NM, St-Hilaire A, Aakre JM, Seghers JP. Life events and high-trait reactivity together predict psychotic symptom increases in schizophrenia. Schizophr Bull. 2009;35:638–45.
Beards S, Gayer-Anderson C, Borges S, Dewey ME, Fisher HL, Morgan C. Life events and psychosis: a review and meta-analysis. Schizophr Bull. 2013;39:740–7.
Tripathi A, Bartosh A, Whitehead C, Pillai A. Activation of cell-free mtDNA-TLR9 signaling mediates chronic stress-induced social behavior deficits. Mol Psychiatry. 2023;28:3806–15.
Krolow R, Noschang C, Weis SN, Pettenuzzo LF, Huffell AP, Arcego DM, et al. Isolation stress during the prepubertal period in rats induces long-lasting neurochemical changes in the prefrontal cortex. Neurochem Res. 2012;37:1063–73.
Ridout KK, Coe JL, Parade SH, Marsit CJ, Kao H-T, Porton B, et al. Molecular markers of neuroendocrine function and mitochondrial biogenesis associated with early life stress. Psychoneuroendocrinology. 2020;116:104632.
Ruigrok SR, Yim K, Emmerzaal TL, Geenen B, Stöberl N, den Blaauwen JL, et al. Effects of early-life stress on peripheral and central mitochondria in male mice across ages. Psychoneuroendocrinology. 2021;132:105346.
Woods SW. Chlorpromazine equivalent doses for the newer atypical antipsychotics. J Clin Psychiatry. 2003;64:663–7.
Overall JE, Gorham DR. The brief psychiatric rating scale. Psychol Rep. 1962;10:799–812.
Kirkpatrick B, Strauss GP, Nguyen L, Fischer BA, Daniel DG, Cienfuegos A, et al. The brief negative symptom scale: psychometric properties. Schizophr Bull. 2011;37:300–5.
Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, et al. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abus Negl. 2003;27:169–90.
Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–96.
Mullins PG, McGonigle DJ, O’Gorman RL, Puts NAJ, Vidyasagar R, Evans CJ, et al. Current practice in the use of MEGA-PRESS spectroscopy for the detection of GABA. Neuroimage. 2014;86:43–52.
Yoon SH, Park CM, Lee CH, Song I-C, Lee HJ, Goo JM. Feasibility of In vivo proton magnetic resonance spectroscopy for lung cancer. Journal Korean Soc Magn Reson Med. 2012;16:40–46.
Rowland LM, Pradhan S, Korenic S, Wijtenburg SA, Hong LE, Edden RA, et al. Elevated brain lactate in schizophrenia: a 7 T magnetic resonance spectroscopy study. Transl Psychiatry. 2016;6:e967.
Erbay MF, Zayman EP, Erbay LG, Ünal S. Evaluation of transcranial magnetic stimulation efficiency in major depressive disorder patients: A magnetic resonance spectroscopy study. Psychiatry Investig. 2019;16:745–50.
Soeiro-De-Souza MG, Pastorello BF, Leite DaCosta, Henning C, Moreno A, Otaduy RA. MCG. Dorsal anterior cingulate lactate and glutathione levels in euthymic bipolar i disorder: 1H-MRS study. Int J Neuropsychopharmacol. 2016;19:1–8.
Batistuzzo MC, Sottili BA, Shavitt RG, Lopes AC, Cappi C, de Mathis MA, et al. Lower ventromedial prefrontal cortex glutamate levels in patients with obsessive–compulsive disorder. Front Psychiatry. 2021;12:668304.
Koush Y, de Graaf RA, Kupers R, Dricot L, Ptito M, Behar KL, et al. Metabolic underpinnings of activated and deactivated cortical areas in human brain. Journal Cereb Blood Flow Metab. 2021;41:986–1000.
Xu J, Dydak U, Harezlak J, Nixon J, Dzemidzic M, Gunn AD, et al. Neurochemical abnormalities in unmedicated bipolar depression and Mania: A 2D 1H MRS Investigation. Psychiatry Res. 2013;213:235.
Quadrelli S, Mountford C, Ramadan S. Hitchhiker’S Guide to Voxel Segmentation for Partial Volume Correction of in Vivo Magnetic Resonance Spectroscopy. Magn Reson Insights. 2016;9:MRI.S32903.
Near J, Harris AD, Juchem C, Kreis R, Marjańska M, Öz G, et al. Preprocessing, analysis and quantification in single-voxel magnetic resonance spectroscopy: experts’ consensus recommendations. NMR Biomed. 2021;34:e4257.
Regenold WT, Phatak P, Marano CM, Sassan A, Conley RR, Kling MA. Elevated cerebrospinal fluid lactate concentrations in patients with bipolar disorder and schizophrenia: implications for the mitochondrial dysfunction hypothesis. Biol Psychiatry. 2008;65:489.
Provencher SW. Automatic quantitation of localized in vivo 1H spectra with LCModel. NMR Biomed. 2001;14:260–4.
Zöllner HJ, Davies-Jenkins CW, Murali-Manohar S, Gong T, Hui SCN, Song Y, et al. Feasibility and implications of using subject-specific macromolecular spectra to model short-TE MRS data. NMR Biomed. 2022;36:e4854.
Trumpff C, Michelson J, Lagranha CJ, Taleon V, Karan KR, Sturm G, et al. Stress and circulating cell-free mitochondrial DNA: A systematic review of human studies, physiological considerations, and technical recommendations. Mitochondrion. 2021;59:225–45.
Maggo S, North LY, Ozuna A, Ostrow D, Grajeda YR, Hakimjavadi H, et al. A method for measuring mitochondrial DNA copy number in pediatric populations. Front Pediatr. 2024;12:1401737.
Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2-ΔΔCT method. Methods. 2001;25:402–8.
Zhang L, Deng S, Zhao S, Ai Y, Zhang L, Pan P, et al. Intra-peritoneal administration of mitochondrial DNA provokes acute lung injury and systemic inflammation via toll-like receptor 9. Int J Mol Sci. 2016;17:1425.
Wiersma M, van Marion DMS, Bouman EJ, Li J, Zhang D, Ramos KS, et al. Cell-free circulating mitochondrial dna: A potential blood-based marker for atrial fibrillation. Cells. 2020;9:1159.
Sprenger H-G, Langer T. The good and the bad of mitochondrial breakups. Trends Cell Biol. 2019;29:888–900.
Neustadt J, Pieczenik SR. Medication-induced mitochondrial damage and disease. Mol Nutr Food Res. 2008;52:780–8.
Chan ST, McCarthy MJ, Vawter MP. Psychiatric drugs impact mitochondrial function in brain and other tissues. Schizophr Res. 2019;217:136.
Cakir Y, Yang Z, Knight CA, Pompilius M, Westbrook D, Bailey SM, et al. Effect of alcohol and tobacco smoke on mtDNA damage and atherogenesis. Free Radic Biol Med. 2007;43:1279–88.
Yang Z, Harrison CM, Chuang GC, Ballinger SW. The role of tobacco smoke induced mitochondrial damage in vascular dysfunction and atherosclerosis. Mutation Res/Fundam Mol Mech Mutagen. 2007;621:61–74.
Norman M, Ter-Ovanesyan D, Trieu W, Lazarovits R, Kowal EJK, Lee JH, et al. L1CAM is not associated with extracellular vesicles in human cerebrospinal fluid or plasma. Nat Methods. 2021;18:631–4.
Nogueras-Ortiz CJ, Eren E, Yao P, Calzada E, Dunn C, Volpert O, et al. Single-extracellular vesicle (EV) analyses validate the use of L1 cell adhesion molecule (L1CAM) as a reliable biomarker of neuron-derived EVs. J Extracell Vesicles. 2024;13:e12459.
Santos C, Martinez M, Lima M, Hao Y-J, Simoes N, Montiel R. Mitochondrial DNA mutations in cancer: a review. Curr Top Med Chem. 2008;8:1351–66.
Smith ALM, Whitehall JC, Greaves LC. Mitochondrial DNA mutations in ageing and cancer. Mol Oncol. 2022;16:3276–94.
Khotina VA, Vinokurov AY, Sinyov VV, Zhuravlev AD, Popov DY, Sukhorukov VN, et al. Mitochondrial dysfunction associated with mtDNA mutation: mitochondrial genome editing in atherosclerosis research. Curr Med Chem. 2024. 2024.
Risi B, Imarisio A, Cuconato G, Padovani A, Valente EM, Filosto M. Mitochondrial DNA (mtDNA) as fluid biomarker in neurodegenerative disorders: A systematic review. Eur J Neurol. 2025;32:e70014.
Fuke S, Kametani M, Kato T. Quantitative analysis of the 4977-bp common deletion of mitochondrial DNA in postmortem frontal cortex from patients with bipolar disorder and schizophrenia. Neurosci Lett. 2008;439:173–7.
Mamdani F, Rollins B, Morgan L, Sequeira PA, Vawter MP. The somatic common deletion in mitochondrial DNA is decreased in schizophrenia. Schizophr Res. 2014;159:370–5.
Win PW, Singh SM, Castellani CA. Mitochondrial DNA Copy Number and Heteroplasmy in Monozygotic Twins Discordant for Schizophrenia. Twin Res Hum Genet. 2023;26:280–9.
San-Millan I, Sparagna GC, Chapman HL, Warkins VL, Chatfield KC, Shuff SR, et al. Chronic lactate exposure decreases mitochondrial function by inhibition of fatty acid uptake and cardiolipin alterations in neonatal rat cardiomyocytes. Front Nutr. 2022;9.
Glancy B, Kane DA, Kavazis AN, Goodwin ML, Willis WT, Gladden LB. Mitochondrial lactate metabolism: history and implications for exercise and disease. J Physiol. 2021;599:863–88.
Takahashi K, Tamura Y, Kitaoka Y, Matsunaga Y, Hatta H. Effects of lactate administration on mitochondrial respiratory function in mouse skeletal muscle. Front Physiol. 2022;13.
Brooks GA, Dubouchaud H, Brown M, Sicurello JP, Butz CE. Role of mitochondrial lactate dehydrogenase and lactate oxidation in the intracellular lactate shuttle. 1999;96:1129–34.
Kochunov P, Ma Y, Hatch KS, Gao S, Acheson A, Jahanshad N, et al. Ancestral, pregnancy, and negative early-life risks shape children’s brain (Dis)similarity to Schizophrenia. Biol Psychiatry. 2023;94:332–40.
Robison RK, Haynes JR, Ganji SK, Nockowski CP, Kovacs Z, Pham W, et al. J-Difference editing (MEGA) of lactate in the human brain at 3T. Magn Reson Med. 2023;90:852–62.
Maier S, Nickel K, Lange T, Oeltzschner G, Dacko M, Endres D, et al. Increased cerebral lactate levels in adults with autism spectrum disorders compared to non-autistic controls: a magnetic resonance spectroscopy study. Mol Autism. 2023;14.
Mustapic M, Eitan E, Werner JK, Berkowitz ST, Lazaropoulos MP, Tran J, et al. Plasma extracellular vesicles enriched for neuronal origin: A potential window into brain pathologic processes. Front Neurosci. 2017;11:278.
Funding
Funding support was received from NIH grants R01MH133812, R01MH116948, R01MH112180 (LEH), MH120876 and MH128771 (AP).
Author information
Authors and Affiliations
Contributions
AA, AT, AKP and LEH wrote the paper; LEH and AKP obtained funding. AA, AT, BP, YM, JJC, SI, BA, and PK contributed to data collection, processing, and/or analysis, all contributed to manuscript editing, critical revision, and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
LEH has received or plans to receive research funding or consulting fees on research projects from Mitsubishi, Your Energy Systems LLC, Neuralstem, Taisho, Heptares, Pfizer, Luye Pharma, IGC Pharma, Sound Pharma, Regeneron, Takeda, and Alto Neuroscience. Other authors declare no conflicts of interest with respect to this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ankeeta, A., Tripathi, A., Pillai, B. et al. Blood and neuronal extracellular vesicle mitochondrial disruptions in schizophrenia. Neuropsychopharmacol. (2025). https://doi.org/10.1038/s41386-025-02204-1
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41386-025-02204-1