Abstract
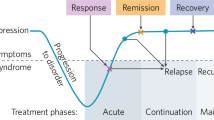
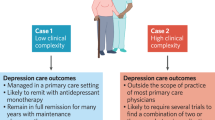
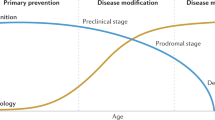
Depression is a leading cause of disease burden, disability, and distress for millions of older adults. Therefore, prevention of late-life depression (LLD) is a research and public health priority. Much of the research on depression prevention has been guided by the central framework of prevention of mental disorders that was developed by the National Academies of Medicine (NAM). This framework features three modes of prevention, centered on the group or people at risk: 1) indicated prevention, which focuses on those who have symptoms but are below the threshold of clinical disease; 2) selective prevention, which focuses on persons at higher risk to develop a disease because of having key risk factors; 3) universal prevention, which focuses on the population as a whole, regardless of risk factors or risk status. This perspective will provide illustrative examples of all three NAM modes of prevention, including one example from the author’s work that simultaneously addressed indicated, selective, and universal prevention of late-life depression in the VITamin D and OmegA-3 TriaL-Depression Endpoint Prevention (VITAL-DEP) study. This paper will also discuss next steps in research to advance LLD prevention, with a view toward ensuring that all older adults can benefit from the increasing range of prevention options available.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 13 print issues and online access
$259.00 per year
only $19.92 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Committee on Prevention of Mental Disorders: Institute of Medicine. Reducing risks for mental disorders: frontiers for preventive intervention research. Washington, DC: National Academy Press; 1994.
Centers for Disease Control. A framework for assessing the effectiveness of disease and injury prevention. MMWR. 1992;41:1–12.
Buntrock C, Harrer M, Sprenger AA, Illing S, Sakata M, Furukawa TA, et al. Psychological interventions to prevent the onset of major depression in adults: a systematic review and individual participant data meta-analysis. Lancet Psychiatry. 2024;11:990–1001.
Cuijpers P, van Straten A, Smit F, Mihalopoulos C, Beekman A. Preventing the onset of depressive disorders: a meta-analytic review of psychological interventions. Am J Psychiatry. 2008;165:1272–80.
Berk M, Woods RL, Nelson MR, Shah RC, Reid CM, Storey E, et al. Effect of aspirin vs placebo on the prevention of depression in older people: a randomized clinical trial. JAMA Psychiatry. 2020;77:1012–20.
Bot M, Brouwer IA, Roca M, Kohls E, Penninx B, Watkins E, et al. Effect of multinutrient supplementation and food-related behavioral activation therapy on prevention of major depressive disorder among overweight or obese adults with subsyndromal depressive symptoms: the MooDFOOD randomized clinical trial. JAMA. 2019;321:858–68.
Okereke OI, Reynolds CF III, Mischoulon D, Chang G, Vyas CM, Cook NR, et al. Effect of long-term vitamin D3 supplementation vs placebo on risk of depression or clinically relevant depressive symptoms and on change in mood scores: a randomized clinical trial. JAMA. 2020;324:471–80.
Okereke OI, Reynolds CF, Mischoulon D, Chang GC, Cook NR, Copeland T, et al. The VITamin D and OmegA-3 trial-depression endpoint prevention (VITAL-DEP): rationale and design of a large-scale ancillary study evaluating vitamin D and marine omega-3 fatty acid supplements for prevention of late-life depression. Contemp Clin Trials. 2018;68:133–45.
Lyness JM, Heo M, Datto CJ, Ten Have TR, Katz IR, Drayer R, et al. Outcomes of minor and subsyndromal depression among elderly patients in primary care settings. Ann Intern Med. 2006;144:496–504.
Lyness JM, Kim J, Tang W, Tu X, Conwell Y, King DA, et al. The clinical significance of subsyndromal depression in older primary care patients. Am J Geriatr Psychiatry. 2007;15:214–23.
van’t Veer-Tazelaar PJ, van Marwijk HW, van Oppen P, van Hout HP, van der Horst HE, Cuijpers P, et al. Stepped-care prevention of anxiety and depression in late life: a randomized controlled trial. Arch Gen Psychiatry. 2009;66:297–304.
Barry MJ, Nicholson WK, Silverstein M, Chelmow D, Coker TR, Davidson KW, et al. Screening for depression and suicide risk in adults: US Preventive Services Task Force Recommendation Statement. JAMA. 2023;329:2057–67.
Schoevers RA, Smit F, Deeg DJ, Cuijpers P, Dekker J, van Tilburg W, et al. Prevention of late-life depression in primary care: Do we know where to begin?. Am J Psychiatry. 2006;163:1611–21.
Chang SC, Pan A, Kawachi I, Okereke OI. Risk factors for late-life depression: a prospective cohort study among older women. Prev Med. 2016;91:144–51.
Rovner BW, Casten RJ, Hegel MT, Leiby BE, Tasman WS. Preventing depression in age-related macular degeneration. Arch Gen Psychiatry. 2007;64:886–92.
Irwin MR, Carrillo C, Sadeghi N, Bjurstrom MF, Breen EC, Olmstead R. Prevention of incident and recurrent major depression in older adults with insomnia: a randomized clinical trial. JAMA Psychiatry. 2022;79:33–41.
Sánchez-Villegas A, Martínez-González MA, Estruch R, Salas-Salvadó J, Corella D, Covas MI, et al. Mediterranean dietary pattern and depression: the PREDIMED randomized trial. BMC Med. 2013;11:208.
Robinson RG, Jorge RE. Post-stroke depression: a review. Am J Psychiatry. 2016;173:221–31.
Musselman DL, Lawson DH, Gumnick JF, Manatunga AK, Penna S, Goodkin RS, et al. Paroxetine for the prevention of depression induced by high-dose interferon alfa. N Engl J Med. 2001;344:961–6.
Sarkar S, Schaefer M. Antidepressant pretreatment for the prevention of interferon alfa-associated depression: a systematic review and meta-analysis. Psychosomatics. 2014;55:221–34.
Collins LM, Murphy SA, Nair VN, Strecher VJ. A strategy for optimizing and evaluating behavioral interventions. Ann Behav Med. 2005;30:65–73.
Baker LD, Espeland MA, Whitmer RA, Snyder HM, Leng X, Lovato L, et al. Structured vs self-guided multidomain lifestyle interventions for global cognitive function: the US POINTER randomized clinical trial. JAMA. 2025;334:681–91.
Cuijpers P. Examining the effects of prevention programs on the incidence of new cases of mental disorders: the lack of statistical power. Am J Psychiatry. 2003;160:1385–91.
Okereke OI, Lyness JM, Lotrich FE, Reynolds CF III. Depression in late-life: a focus on prevention. Focus (Am Psychiatr Publ). 2013;11:22–31.
Okereke OI, Vyas CM, Mischoulon D, Chang G, Cook NR, Weinberg A, et al. Effect of long-term supplementation with marine omega-3 fatty acids vs placebo on risk of depression or clinically relevant depressive symptoms and on change in mood scores: a randomized clinical trial. JAMA. 2021;326:2385–94.
Vyas CM, Mischoulon D, Chang G, Cook NR, Weinberg A, Copeland T, et al. Effects of vitamin D(3) and marine omega-3 fatty acids supplementation on indicated and selective prevention of depression in older adults: results from the clinical center sub-cohort of the VITamin D and omegA-3 triaL (VITAL). J Clin Psychiatry. 2023;84:22m14629.
Kroenke K, Strine TW, Spitzer RL, Williams JB, Berry JT, Mokdad AH. The PHQ-8 as a measure of current depression in the general population. J Affect Disord. 2009;114:163–73.
Huang FY, Chung H, Kroenke K, Delucchi KL, Spitzer RL. Using the Patient Health Questionnaire-9 to measure depression among racially and ethnically diverse primary care patients. J Gen Intern Med. 2006;21:547–52.
Hepner KA, Morales LS, Hays RD, Edelen MO, Miranda J. Evaluating differential item functioning of the PRIME-MD mood module among impoverished black and white women in primary care. Women's Health Issues. 2008;18:53–61.
Gilbody S, Littlewood E, McMillan D, Chew-Graham CA, Bailey D, Gascoyne S, et al. Behavioural activation to prevent depression and loneliness among socially isolated older people with long-term conditions: The BASIL COVID-19 pilot randomised controlled trial. PLoS Med. 2021;18:e1003779.
Dias A, Azariah F, Anderson SJ, Sequeira M, Cohen A, Morse JQ, et al. Effect of a lay counselor intervention on prevention of major depression in older adults living in low- and middle-income countries: a randomized clinical trial. JAMA Psychiatry. 2019;76:13–20.
Glasgow RE, Lichtenstein E, Marcus AC. Why don’t we see more translation of health promotion research to practice? Rethinking the efficacy-to-effectiveness transition. Am J Public Health. 2003;93:1261–7.
Gaugler JE, Baier RR, Baker ZG, Boltz M, Fortinsky RH, Gustavson AM, et al. Using hybrid effectiveness studies to facilitate implementation in community-based settings: three case studies in dementia care Research. J Am Med Dir Assoc. 2024;25:27–33.
Herrman H, Patel V, Kieling C, Berk M, Buchweitz C, Cuijpers P, et al. Time for united action on depression: a Lancet-World Psychiatric Association Commission. Lancet. 2022;399:957–1022.
Author information
Authors and Affiliations
Contributions
Okereke is solely responsible for the conception or design of the work; drafted the work and revised it critically for important intellectual content; approved of the final version to be published; and is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Competing interests
Okereke has received royalties from Springer Publishing for a book on late-life depression prevention.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Okereke, O.I. Prevention of late-life depression: a framework and prospectus for research. Neuropsychopharmacol. (2026). https://doi.org/10.1038/s41386-026-02339-9
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41386-026-02339-9
This article is cited by
-
Neuropsychiatric illness in the later years of life: summary and synthesis
Neuropsychopharmacology (2026)