Abstract
Background
Heme is the prosthetic group of numerous proteins involved in vital processes such as oxygen transport, oxidative stress, and energetic mitochondrial metabolism. Free heme also plays a significant role at early stages of development and in cell differentiation processes. The metabolism of heme by the fetal placenta unit is not well-established in humans.
Methods
In a retrospective study, we measured heme precursors in the amniotic fluid (AF) of 51 healthy women, and 10 AF samples from pregnancies with either upper or lower intestinal atresia or ileus were also analyzed.
Results
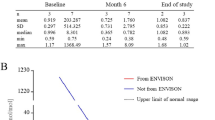
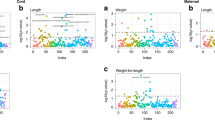
We showed that the porphyrin precursors aminolevulinic acid, porphobilinogen, and protoporphyrin IX are present at the limit of detection in the AF. Total porphyrin levels decreased progressively from week 13 to week 33 (p < 0.01). Interestingly, uroporphyrin, initially detected as traces, increased with maturation, in contrast to coproporphyrin. Uro- and coproporphyrins were type I immature isomers (>90%), suggesting a lack of maturity in the fetal compartment of the heme pathway. Finally, the differential analysis of AF from normal and pathological pregnancies demonstrated the predominant hepatic origin of fetal porphyrins excreted in the AF.
Conclusion
This study gives the first insight into heme metabolism in the AF during normal and pathological pregnancies.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Joshi, M., Kulkarni, A. & Pal, J. K. Small molecule modulators of eukaryotic initiation factor 2alpha kinases, the key regulators of protein synthesis. Biochimie 95, 1980–1990 (2013).
Sibley, C. P. Treating the dysfunctional placenta. J. Endocrinol. 234, 81–97 (2017).
George, E. M. & Granger, J. P. Heme oxygenase in pregnancy and preeclampsia. Curr. Opin. Nephrol. Hypertens. 22, 156–162 (2013).
Lenglet, H. et al. From a dominant to an oligogenic model of inheritance with environmental modifiers in acute intermittent porphyria. Hum. Mol. Genet. 27, 1164–1173 (2018).
Karim, Z. et al. Porphyrias: a 2015 update. Clin. Res. Hepatol. Gastroenterol. 39, 412–425 (2015).
Manceau, H., Gouya, L. & Puy, H. Acute hepatic and erythropoietic porphyrias: from ALA synthases 1 and 2 to new molecular bases and treatments. Curr. Opin. Hematol. 24, 198–207 (2017).
Balwani, M. & Desnick, RJ. The porphyrias: advances in diagnosis and treatment. Blood 120, 4496–4504 (2012).
Puy, H., Gouya, L. & Deybach, J. C. Porphyrias. Lancet 375, 924–937 (2010).
Pannier, E. et al. Congenital erythropoietic porphyria (Gunther’s disease): two cases with very early prenatal manifestation and cystic hygroma. Prenat. Diagn. 23, 25–30 (2003).
Beall, M. H. et al. Regulation of amniotic fluid volume. Placenta 28, 824–832 (2007).
Muller, F. et al. Amniotic fluid digestive enzymes: diagnostic value in fetal gastrointestinal obstructions. Prenat. Diagn. 14, 973–979 (1994).
Muller, F. et al. Microvillar enzyme assays in amniotic fluid and fetal tissues at different stages of development. Prenat. Diagn. 8, 189–198 (1988).
Lockwood, W. H. et al. Rapid procedure for fecal porphyrin assay. Clin. Chem. 31, 1163–1167 (1985).
Lim, C. K., Li, F. M. & Peters, T. J. High-performance liquid chromatography of porphyrins. J. Chromatogr. 429, 123–153 (1988).
Macours, P. & Cotton, F. Improvement in HPLC separation of porphyrin isomers and application to biochemical diagnosis of porphyrias. Clin. Chem. Lab Med. 44, 1433–1440 (2006).
Fikentscher, R., Schmidt, M. & Stich, W. Studies on fetal metabolism of heme. I. The pattern of the precursors of heme of human amniotic fluid. Klin. Wochenschr. 45, 353–355 (1967).
Goodlin, R. C. & Schwartz, S. Coproporphrin content of amniotic fluid in normal and diseased infants. Am. J. Obstet. Gynecol. 84, 808–811 (1962).
Wolkoff, A. W. & Arias, I. M. Coproporphyrin excretion in amniotic fluid and urine from premature infants: a possible maturation defect. Pediatr. Res. 8, 591–593 (1974).
Gourley, G. R., Kreamer, B. & Arend, R. Excremental studies in human neonates. Identification of zinc coproporphyrin as a marker for meconium. Gastroenterology 99, 1705–1709 (1990).
Usta, I. M., Mercer, B. M. & Sibai, B. M. Risk factors for meconium aspiration syndrome. Obstet. Gynecol. 86, 230–234 (1995).
Kaplowitz, N., Javitt, N. & Kappas, A. Coproporphyrin I and 3 excretion in bile and urine. J. Clin. Invest. 51, 2895–2899 (1972).
Badminton, M. N. & Deybach, J. C. Treatment of an acute attack of porphyria during pregnancy. Eur. J. Neurol. 13, 668–669 (2006).
Acknowledgements
We are very grateful to Sylvie Simonin for porphyrin quantification and to Nathalie Dessendier for ALA and PBG measurements in amniotic fluid. This study was supported by grants from Laboratory of Excellence GR-Ex, reference ANR-11-LABX-0051. The program “Investissements d’avenir” of the French National Research Agency, reference ANR-11-IDEX-0005-02, funded the labex GR-Ex.
Funding
This study was supported by grants from Laboratory of Excellence GR-Ex, reference ANR-11-LABX-0051.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Manceau, H., Puy, V., Schmitt, C.M. et al. Characterization and origin of heme precursors in amniotic fluid: lessons from normal and pathological pregnancies. Pediatr Res 84, 80–84 (2018). https://doi.org/10.1038/s41390-018-0011-2
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-018-0011-2