Abstract
Background
Sepsis in preterm infants is associated with systemic inflammatory responses. The stress-response protein heme oxygenase-1 (HO-1) has protective anti-inflammatory properties. Recently, we reported a protective role of HO-1 using our non-surgical cecal slurry (CS) model in wild-type (WT) mouse pups. Here, we extend these findings to investigate the association of HO-1 deficiency with sepsis severity.
Methods
Adapting the Wynn model, we induced sepsis in 4-day-old HO-1-deficient (HO-1+/−, Het) pups to determine if HO-1 deficiency affected survival rates at the LD40 (2.0 mg/g) of WT pups. To see if HO-1 induction affected sepsis severity, we gave 30-μmol heme/kg subcutaneously to 3-day-old mice 24 h prior to sepsis induction.
Results
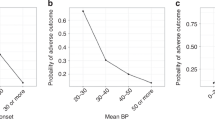
Post-sepsis induction, Het pups had a mortality of 85.0% (n = 20) and increased expression of the pro-inflammatory gene in the livers and affected hematologic profiles. Heme treatment 24 h prior to sepsis induction significantly increased liver HO activity, reduced mortality to 24.5% (n = 17), attenuated inflammatory responses, reduced spleen bacterial counts, and significantly increased peripheral neutrophils.
Conclusions
A partial deficiency in HO-1 increased the progression and mortality in sepsis. Furthermore, induction of HO-1 significantly reduced the mortality even in Het pups. Thus, we conclude that HO-1 plays an important role in the protection against preterm sepsis.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Wynn, J. L. & Wong, H. R. Pathophysiology and treatment of septic shock in neonates. Clin. Perinatol. 37, 439–479 (2010).
Wynn, J. L. et al. Increased mortality and altered immunity in neonatal sepsis produced by generalized peritonitis. Shock 28, 675–683 (2007).
Stoll, B. J. et al. Early onset neonatal sepsis: the burden of group B Streptococcal and E. coli disease continues. Pediatrics 127, 817–826 (2011).
Maines, M. D. Heme oxygenase: function, multiplicity, regulatory mechanisms, and clinical applications. FASEB J. 2, 2557–2568 (1988).
Tenhunen, R., Marver, H. S. & Schmid, R. The enzymatic conversion of heme to bilirubin by microsomal heme oxygenase. Proc. Natl Acad. Sci. USA 61, 748–755 (1968).
Stocker, R., Yamamoto, Y., Mcdonagh, A. F., Glazer, A. N. & Ames, B. N. Bilirubin is an antioxidant of possible physiological importance. Science 235, 1043–1046 (1987).
Chung, S. W., Liu, X., Macias, A. A., Baron, R. M. & Perrella, M. A. Heme oxygenase-1-derived carbon monoxide enhances the host defense response to microbial sepsis in mice. J. Clin. Invest. 118, 239–247 (2008).
Tsoyi, K. et al. Heme-oxygenase-1 induction and carbon monoxide-releasing molecule inhibit lipopolysaccharide (LPS)-induced high-mobility group box 1 release in vitro and improve survival of mice in LPS- and cecal ligation and puncture-induced sepsis model in vivo. Mol. Pharmacol. 76, 173–182 (2009).
Carchman, E. H., Rao, J., Loughran, P. A., Rosengart, M. R. & Zuckerbraun, B. S. Heme oxygenase-1-mediated autophagy protects against hepatocyte cell death and hepatic injury from infection/sepsis in mice. Hepatology 53, 2053–2062 (2011).
Czaikoski, P. G. et al. Heme oxygenase inhibition enhances neutrophil migration into the bronchoalveolar spaces and improves the outcome of murine pneumonia-induced sepsis. Shock 39, 389–396 (2013).
Takaki, S. et al. Beneficial effects of the heme oxygenase-1/carbon monoxide system in patients with severe sepsis/septic shock. Intensive Care. Med. 36, 42–48 (2010).
Vazquez-Armenta, G. et al. Short (GT)n microsatellite repeats in the heme oxygenase-1 gene promoter are associated with antioxidant and anti-inflammatory status in Mexican pediatric patients with sepsis. Tohoku. J. Exp. Med. 231, 201–209 (2013).
Fujioka, K. et al. Induction of heme oxygenase-1 attenuates the severity of sepsis in a non-surgical preterm mouse model. Shock 47, 242–250 (2017).
Starr, M. E. et al. A new cecal slurry preparation protocol with improved long-term reproducibility for animal models of sepsis. PLoS ONE 9, e115705 (2014).
Steele, A. M., Starr, M. E. & Saito, H. Late therapeutic intervention with antibiotics and fluid resuscitation allows for a prolonged disease course with high survival in a severe murine model of sepsis. Shock 47, 726–734 (2017).
Adkins, B., Leclerc, C. & Marshall-Clarke, S. Neonatal adaptive immunity comes of age. Nat. Rev. Immunol. 4, 553–564 (2004).
Zhao, H., Wong, R. J., Kalish, F. S., Nayak, N. R. & Stevenson, D. K. Effect of heme oxygenase-1 deficiency on placental development. Placenta 30, 861–868 (2009).
He, C. X. et al. Effects of zinc deuteroporphyrin bis glycol on newborn mice after heme-loading. Pediatr. Res. 70, 467–472 (2011).
Fujioka, K., Kalish, F., Wong, R. J. & Stevenson, D. K. Inhibition of heme oxygenase activity using a microparticle formulation of zinc protoporphyrin in an acute hemolytic newborn mouse model. Pediatr. Res. 79, 251–257 (2016).
Kronforst, K. D. et al. A neonatal model of intravenous Staphylococcus epidermidis infection in mice 24 h old enables characterization of early innate immune responses. PLoS ONE 7, e43897 (2012).
Ge, Y. et al. Relationship of tissue and cellular interleukin-1 and lipopolysaccharide after endotoxemia and bacteremia. J. Infect. Dis. 176, 1313–1321 (1997).
Borish, L. C. & Steinke, J. W. 2. Cytokines and chemokines. J. Allergy Clin. Immunol. 111, S460–S475 (2003).
Rot, A. & von Andrian, U. H. Chemokines in innate and adaptive host defense: basic chemokinese grammar for immune cells. Annu. Rev. Immunol. 22, 891–928 (2004).
Stoll, B. J. & Fanaroff, A. Early-onset coagulase-negative staphylococcal sepsis in preterm neonate. National Institute of Child Health and Human Development (NICHD) Neonatal Research Network. Lancet 345, 1236–1237 (1995).
Wang, R. et al. Stress-responsive heme oxygenase-1 isoenzyme participates in Toll-like receptor 4-induced inflammation during brain ischemia. Neuroreport 27, 445–454 (2016).
Liong, S. & Lappas, M. The stress-responsive heme oxygenase (HO)-1 isoenzyme is increased in labouring myometrium where it regulates contraction-associated proteins. Am. J. Reprod. Immunol. 74, 62–76 (2015).
Larsen, R. et al. A central role for free heme in the pathogenesis of severe sepsis. Sci. Transl. Med 2, 51ra71 (2010).
Wong, R. J. et al. In vitro inhibition of heme oxygenase isoenzymes by metalloporphyrins. J. Perinatol. 31(Suppl 1), S35–S41 (2011).
Takahashi, K., Nakayama, M., Takeda, K., Fujia, H. & Shibahara, S. Suppression of heme oxygenase-1 mRNA expression by interferon-gamma in human glioblastoma cells. J. Neurochem. 72, 2356–2361 (1999).
Kovacsics, C. E., Gill, A. J., Ambegaokar, S. S., Gelman, B. B. & Kolson, D. L. Degradation of heme oxygenase-1 by the immunoproteasome in astrocytes: a potential interferon-gamma-dependent mechanism contributing to HIV neuropathogenesis. Glia 65, 1264–1277 (2017).
Singh, N. et al. Antimycobacterial effect of IFNG (interferon gamma)-induced autophagy is dependent on the HMOX1 (heme oxygenase 1)-mediated increase in the intracellular calcium levels and modulation of PPP3/calcineurin-TFEB (transcription factor EB) axis. Autophagy (2018). In press. https://doi.org/10.1080/15548627.2018.1436936.
Fujioka, K. et al. Heme oxygenase-1 promoter polymorphisms and risk of spina bifida. Birth Defects Res. A Clin. Mol. Teratol. 103, 741–746 (2015).
Ono, K. et al. A promoter variant of the heme oxygenase-1 gene may reduce the incidence of ischemic heart disease in Japanese. Atherosclerosis 173, 315–319 (2004).
Exner, M., Minar, E., Wagner, O. & Schillinger, M. The role of heme oxygenase-1 promoter polymorphisms in human disease. Free Radic. Biol. Med. 37, 1097–1104 (2004).
Lopalco, L. CCR5: from natural resistance to a new anti-HIV strategy. Viruses 2, 574–600 (2010).
Prahalad, S. Negative association between the chemokine receptor CCR5-Delta32 polymorphism and rheumatoid arthritis: a meta-analysis. Genes Immun. 7, 264–268 (2006).
Yang, Y. F. et al. A non-peptide CCR5 antagonist inhibits collagen-induced arthritis by modulating T cell migration without affecting anti-collagen T cell responses. Eur. J. Immunol. 32, 2124–2132 (2002).
Schroder, C. et al. CCR5 blockade modulates inflammation and alloimmunity in primates. J. Immunol. 179, 2289–2299 (2007).
Minamino, T. et al. Targeted expression of heme oxygenase-1 prevents the pulmonary inflammatory and vascular responses to hypoxia. Proc. Natl Acad. Sci. USA 98, 8798–8803 (2001).
Schumacher, A. & Zenclussen, A. C. Effects of heme oxygenase-1 on innate and adaptive immune responses promoting pregnancy success and allograft tolerance. Front. Pharmacol. 5, 288 (2014).
Acknowledgements
We thank Dr. Hendrik J. Vreman for an invaluable advice on our experimental design. This work was supported by the Christopher Hess Research Fund, the H.M. Lui Research Fund (Hong Kong), the Mary L. Johnson Research Fund, and the Child Health Research Institute at Stanford, and the Kobe Sinryokukai Association (Japan), JSPS KAKENHI Grant Number 16H06971 (Japan), and the Mother and Child Health Foundation (Japan).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fujioka, K., Kalish, F., Zhao, H. et al. Heme oxygenase-1 deficiency promotes severity of sepsis in a non-surgical preterm mouse model. Pediatr Res 84, 139–145 (2018). https://doi.org/10.1038/s41390-018-0028-6
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41390-018-0028-6
This article is cited by
-
A neonatal mouse model of meconium peritonitis generated using human meconium slurry
Pediatric Research (2025)
-
Moderate exercise-induced dynamics on key sepsis-associated signaling pathways in the liver
Critical Care (2023)
-
Early career investigator highlight biocommentary
Pediatric Research (2021)
-
Prophylactic therapy with human amniotic fluid stem cells improved survival in a rat model of lipopolysaccharide-induced neonatal sepsis through immunomodulation via aggregates with peritoneal macrophages
Stem Cell Research & Therapy (2020)
-
Recombinant human thrombomodulin attenuated sepsis severity in a non-surgical preterm mouse model
Scientific Reports (2020)