Abstract
Background
Impaired cerebral autoregulation in preterm infants makes circulatory management important to avoid cerebral hypoxic–ischemic injury. Dobutamine is frequently used as inotropic treatment in preterm neonates, but its effects on the brain exposed to cerebral hypoxia are unknown. We hypothesized that dobutamine would protect the immature brain from cerebral hypoxic injury.
Methods
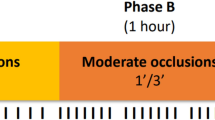
In preterm (0.6 gestation) fetal sheep, dobutamine (Dob, 10 μg/kg/min) or saline (Sal) was infused intravenously for 74 h. Two hours after the beginning of the infusion, umbilical cord occlusion (UCO) was performed to produce fetal asphyxia (Sal+UCO: n = 9, Dob+UCO: n = 7), or sham occlusion (Sal+sham: n = 7, Dob+sham: n = 6) was performed. Brains were collected 72 h later for neuropathology.
Results
Dobutamine did not induce cerebral changes in the sham UCO group. UCO increased apoptosis and microglia density in white matter, hippocampus, and caudate nucleus, and astrocyte density in the caudate nucleus. Dobutamine commenced before UCO reduced microglia infiltration in the white matter, and microglial and astrocyte density in the caudate.
Conclusion
In preterm hypoxia-induced brain injury, dobutamine decreases neuroinflammation in the white matter and caudate, and reduces astrogliosis in the caudate. Early administration of dobutamine in preterm infants for cardiovascular stabilization appears safe and may be neuroprotective against unforeseeable cerebral hypoxic injury.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Omizzolo, C. et al. Neonatal brain abnormalities and memory and learning outcomes at 7 years in children born very preterm. Memory 22, 605–615 (2014).
Back, S. A., Riddle, A. & McClure, M. M. Maturation-dependent vulnerability of perinatal white matter in premature birth. Stroke 38, 724–730 (2007).
O’Leary, H. et al. Elevated cerebral pressure passivity is associated with prematurity-related intracranial hemorrhage. Pediatrics 124, 302–309 (2009).
Lasky, T., Greenspan, J., Ernst, F. R. & Gonzalez, L. Dopamine and dobutamine use in preterm or low birth weight neonates in the premier 2008 database. Clin. Ther. 33, 2082–2088 (2011).
Rios, D. R., Moffett, B. S. & Kaiser, J. R. Trends in pharmacotherapy for neonatal hypotension. J. Pediatr. 165, 697–701 (2014).
Noori, S. & Seri, I. Neonatal blood pressure support: the use of inotropes, lusitropes, and other vasopressor agents. Clin. Perinatol. 39, 221–238 (2012).
Brew, N. et al. Dopamine treatment during acute hypoxia is neuroprotective in the developing sheep brain. Neuroscience 316, 82–93 (2016).
Subhedar N. V., Shaw N. J. Dopamine versus dobutamine for hypotensive preterm infants. Cochrane Database Syst. Rev. CD001242 (2003).
Eiby, Y. A. et al. Inotropes do not increase cardiac output or cerebral blood flow in preterm piglets. Pediatr. Res. 80, 870–879 (2016).
Ferrara, J. J. et al. Effects of dopamine and dobutamine on regional blood flow distribution in the neonatal piglet. Ann. Surg. 221, 531–540 (1995). discussion 540–532.
Junker, V. et al. Stimulation of beta-adrenoceptors activates astrocytes and provides neuroprotection. Eur. J. Pharmacol. 446, 25–36 (2002).
Drury, P. P. et al. Partial neural protection with prophylactic low-dose melatonin after asphyxia in preterm fetal sheep. J. Cereb. Blood Flow. Metab. 34, 126–135 (2014).
Jellema, R. K. et al. Cerebral inflammation and mobilization of the peripheral immune system following global hypoxia-ischemia in preterm sheep. J. Neuroinflamm. 10, 13 (2013).
Mallard, C., Welin, A. K., Peebles, D., Hagberg, H. & Kjellmer, I. White matter injury following systemic endotoxemia or asphyxia in the fetal sheep. Neurochem. Res. 28, 215–223 (2003).
Spittle, A. J. et al. Neonatal white matter abnormality predicts childhood motor impairment in very preterm children. Dev. Med. Child Neurol. 53, 1000–1006 (2011).
Abernethy, L. J., Cooke, R. W. & Foulder-Hughes, L. Caudate and hippocampal volumes, intelligence, and motor impairment in 7-year-old children who were born preterm. Pediatr. Res. 55, 884–893 (2004).
Beauchamp, M. H. et al. Preterm infant hippocampal volumes correlate with later working memory deficits. Brain 131, 2986–2994 (2008).
Johnson J. The Sheep Brain Atlas (online). (Mishigan State University Brain Biodiversity Bank, 2008).Available: http://www.msu.edu/brains/sheep/index.html
Hutton, L. C., Castillo-Melendez, M. & Walker, D. W. Uteroplacental inflammation results in blood brain barrier breakdown, increased activated caspase 3 and lipid peroxidation in the late gestation ovine fetal cerebellum. Dev. Neurosci. 29, 341–354 (2007).
Yawno, T. et al. Human amnion epithelial cells protect against white matter brain injury after repeated endotoxin exposure in the preterm ovine fetus. Cell Transplant. 26, 541–553 (2017).
Nachar, R. A. et al. Dose-dependent hemodynamic and metabolic effects of vasoactive medications in normotensive, anesthetized neonatal piglets. Pediatr. Res. 70, 473–479 (2011).
Robel-Tillig, E., Knupfer, M., Pulzer, F. & Vogtmann, C. Cardiovascular impact of dobutamine in neonates with myocardial dysfunction. Early Hum. Dev. 83, 307–312 (2007).
Kawamura, S. & Yasui, N. Effects of dobutamine on brain surface microvessels in rats. Neurol. Med. Chir. 38, 137–141 (1998).
Bennet, L., Roelfsema, V., Pathipati, P., Quaedackers, J. S. & Gunn, A. J. Relationship between evolving epileptiform activity and delayed loss of mitochondrial activity after asphyxia measured by near-infrared spectroscopy in preterm fetal sheep. J. Physiol. 572, 141–154 (2006).
Penny, D. J., Sano, T. & Smolich, J. J. Increased systemic oxygen consumption offsets improved oxygen delivery during dobutamine infusion in newborn lambs. Intensive Care Med. 27, 1518–1525 (2001).
Markus, T. et al. beta-Adrenoceptor activation depresses brain inflammation and is neuroprotective in lipopolysaccharide-induced sensitization to oxygen-glucose deprivation in organotypic hippocampal slices. J. Neuroinflamm. 7, 94 (2010).
Hagberg, H., Peebles, D. & Mallard, C. Models of white matter injury: comparison of infectious, hypoxic-ischemic, and excitotoxic insults. Ment. Retard. Dev. Disabil. Res. Rev. 8, 30–38 (2002).
Hodges-Savola, C., Rogers, S. D., Ghilardi, J. R., Timm, D. R. & Mantyh, P. W. Beta-adrenergic receptors regulate astrogliosis and cell proliferation in the central nervous system in vivo. Glia 17, 52–62 (1996).
Madrigal, J. L., Kalinin, S., Richardson, J. C. & Feinstein, D. L. Neuroprotective actions of noradrenaline: effects on glutathione synthesis and activation of peroxisome proliferator activated receptor delta. J. Neurochem. 103, 2092–2101 (2007).
Gleason, C. A., Robinson, R., Harris, A. P., Mayock, D. E. & Traystman, R. J. Cerebrovascular effects of intravenous dopamine infusions in fetal sheep. J. Appl. Physiol. 92, 717–724 (2002).
Kim, M. Y. et al. Expression of adrenoceptor subtypes in preterm piglet heart is different to term heart. PLoS ONE 9, e92167 (2014).
Olhager, E. et al. Preterm lambs given intravenous dopamine show increased dopamine in their cerebrospinal fluid. Acta Paediatr. 103, 337–342 (2014).
Creasy, R. K., Drost, M., Green, M. V. & Morris, J. A. Determination of fetal, placental and neonatal blood volumes in the sheep. Circ. Res. 27, 487–494 (1970).
Crossley, K. J. et al. Dynamic changes in the direction of blood flow through the ductus arteriosus at birth. J. Physiol. 587, 4695–4704 (2009).
Bravo, M. C. et al. Randomized, placebo-controlled trial of dobutamine for low superior vena cava flow in infants. J. Pediatr. 167, 572–578 (2015).
Osborn, D., Evans, N. & Kluckow, M. Randomized trial of dobutamine versus dopamine in preterm infants with low systemic blood flow. J. Pediatr. 140, 183–191 (2002).
Noori, S. et al. Hemodynamic changes after low-dosage hydrocortisone administration in vasopressor-treated preterm and term neonates. Pediatrics 118, 1456–1466 (2006).
Hausdorff, W. P., Caron, M. G. & Lefkowitz, R. J. Turning off the signal: desensitization of beta-adrenergic receptor function. FASEB J. 4, 2881–2889 (1990).
Drury, P. P. et al. Dopamine infusion for postresuscitation blood pressure support after profound asphyxia in near-term fetal sheep. Exp. Physiol. 98, 699–709 (2013).
Dempsey, E. M. Challenges in treating low blood pressure in preterm infants. Children 2, 272–288 (2015).
Acknowledgements
We thank Ms Meghan Boomgardt for technical assistance with the immunohistochemistry. This research was supported by funding from National Health and Medical Research Council (NHMRC project Grant APP 1025626) of Australia and the Victorian Government’s Operational Infrastructure Support Program. F.Y.W. is supported by the NHMRC/Cerebral Palsy Alliance Career Development Fellowship (APP 1084254).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Brew, N., Nakamura, S., Hale, N. et al. Dobutamine treatment reduces inflammation in the preterm fetal sheep brain exposed to acute hypoxia. Pediatr Res 84, 442–450 (2018). https://doi.org/10.1038/s41390-018-0045-5
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41390-018-0045-5
This article is cited by
-
Nocturnal hypoxia moderates the relationship between rapid eye movement sleep and anxiety
BMC Psychiatry (2025)
-
Utility of Localized Surface Plasmon Resonance of Gold Nanoparticles for Spectrophotometric Determination of Dobutamine in Pharmaceutical Formulations
Plasmonics (2024)
-
Dobutamine-induced alternations in cerebral blood flow of healthy adults: a 3D pseudocontinuous arterial spin labeling study
BMC Medicine (2023)