Abstract
Background
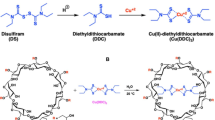
Menkes disease is a copper metabolism disorder caused by mutations in ATP7A, a copper-transporting P-type ATPase. In this study, oral copper supplementation via glyoxal-bis(N(4)-methylthiosemicarbazonato)-copper(II) (CuGTSM), a lipophilic copper complex, was investigated in male hemizygous macular (MoMl/y) mice, a mouse model of Menkes disease.
Methods
CuGTSM was administered by oral gavage on postnatal days 5, 8, 11, 17, 23, and 32. The copper levels in the organs and serum, copper-dependent enzyme activities in the brain, and ceruloplasmin (Cp) activity in the serum were measured at 15 days and 3 and 8 months of age. Histological analysis of the intestines and the rotarod test were also performed.
Results
CuGTSM treatment extended the lifespan of MoMl/y mice and partly restored the copper concentrations and cytochrome oxidase and DBH activities in the brain; however, the rotarod test showed impaired motor performance. The treatment also increased copper concentrations and Cp activity in the serum. In suckling MoMl/y mice, CuGTSM treatment transiently induced diarrhea accompanied by copper accumulation and altered villus morphology in the ileum.
Conclusion
Oral administration of CuGTSM extended the lifespan of MoMl/y mice. Oral administration is attractive, but pharmaceutical studies are needed to reduce the adverse enteral effects.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Tümer, Z. & Møller, L. B. Menkes disease. Eur. J. Hum. Genet 18, 511–518 (2010).
Lutsenko, S. et al. Function and regulation of human copper-transporting ATPases. Physiol. Rev. 87, 1011–1046 (2007).
Choi, B. S. & Zheng, W. Copper transport to the brain by the blood-brain barrier and blood-CSF barrier. Brain Res. 1248, 14–21 (2009).
Sarkar, B., Lingertat-Walsh, K. & Clarke, J. T. Copper-histidine therapy for Menkes disease. J. Pediatr. 123, 828–830 (1993).
Kodama, H. et al. Effect of copper and diethyldithiocarbamate combination therapy on the macular mouse, an animal model of Menkes disease. J. Inherit. Metab. Dis. 28, 971–978 (2005).
Lenartowicz, M. et al. Prenatal treatment of mosaic mice (Atp7a mo-ms) mouse model for Menkes disease, with copper combined by dimethyldithiocarbamate (DMDTC). PLoS ONE 7, e40400 (2012).
Tanaka, K. et al. Effects of chelators on copper therapy of macular mouse, a model animal of Menkes’ kinky disease. Res. Commun. Chem. Pathol. Pharmacol. 69, 217–227 (1990).
Crouch, P. J. et al. Increasing Cu bioavailability inhibits Aβ oligomers and tau phosphorylation. Proc. Natl Acad. Sci. USA 106, 381–386 (2009).
Paterson, B. M. & Donnelly, P. S. Copper complexes of bis(thiosemicarbazones): from chemotherapeutics to diagnostic and therapeutic radiopharmaceuticals. Chem. Soc. Rev. 40, 3005–3018 (2011).
Speer, A. et al. Copper-boosting compounds: a novel concept for antimycobacterial drug discovery. Antimicrob. Agents Chemother. 57, 1089–1091 (2013).
Munakata, M. et al. Copper-trafficking efficacy of copper-pyruvaldehyde bis(N 4- methylthiosemicarbazone) on the macular mouse, an animal model of Menkes disease. Pediatr. Res. 72, 270–276 (2012).
Murata, Y. et al. Mutation analysis and expression of the mottled gene in the macular mouse model of Menkes disease. Pediatr. Res. 42, 436–442 (1997).
Kim, B. E. & Petris, M. J. Phenotypic diversity of Menkes disease in mottled mice is associated with defects in localisation and trafficking of the ATP7A protein. J. Med Genet 44, 641–646 (2007).
Yamano, T. et al. Clinico-pathological study on macular mutant mouse. Acta Neuropathol. 72, 256–260 (1987).
Gingras, B., Suprunchuk, T. & Bayley, C. H. The preparation of some thiosemicarbazones and their copper complexes: Part III. Can. J. Chem. 40, 1053–1059 (1962).
Hunt, D. M. A study of copper treatment and tissue copper levels in the murine congenital copper deficiency, mottled. Life Sci. 19, 1913–1919 (1976).
Gonzalez-Lima, F. & Jones, D. Quantitative mapping of cytochrome oxidase activity in the central auditory system of the gerbil: a study with calibrated activity standards and metal-intensified histochemistry. Brain Res 660, 34–49 (1994).
Wong-Riley, M. T. Cytochrome oxidase: an endogenous metabolic marker for neuronal activity. Trends Neurosci. 12, 94–101 (1989).
Kanarik, M. et al. Changes in regional long-term oxidative metabolism induced by partial serotonergic denervation and chronic variable stress in rat brain. Neurochem Int 52, 432–437 (2008).
Curzon, G. & Vallet, L. The purification of human caeruloplasmin. Biochem J. 74, 279–287 (1960).
Brooks, S. P. & Dunnett, S. B. Tests to assess motor phenotype in mice: a user’s guide. Nat. Rev. Neurosci. 10, 519–529 (2009).
Kanda, Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 48, 452–458 (2013).
Dearling, J. L. et al. Copper bis(thiosemicarbazone) complexes as hypoxia imaging agents: structure-activity relationships. J. Biol. Inorg. Chem. 7, 249–259 (2002).
Hunt, D. M. & Johnson, D. R. An inherited deficiency in noradrenaline biosynthesis in the brindled mouse. J. Neurochem 19, 2811–2819 (1972).
Satoh, J. et al. Neurochemical and immunocytochemical studies of catecholamine system in the brindled mouse. J. Neuropathol. Exp. Neurol. 50, 793–808 (1991).
Meguro, Y. et al. Changes of copper level and cytochrome c oxidase activity in the macular mouse with age. Brain Dev. 13, 184–186 (1991).
Wenk, G. & Suzuki, K. Congenital copper deficiency: copper therapy and dopamine-beta-hydroxylase activity in the mottled (brindled) mouse. J. Neurochem 41, 1648–1652 (1983).
Widdowson, E. M. Trace elements in foetal and early postnatal development. Proc. Nutr. Soc. 33, 275–284 (1974).
Lönnerdal, B. Intestinal regulation of copper homeostasis: a developmental perspective. Am. J. Clin. Nutr. 88, 846s–850ss (2008).
Hardman, B., Luff, S. & Ackland, M. L. Differential intracellular localisation of the Menkes and Wilson copper transporting ATPases in the third trimester human placenta. Placenta 32, 79–85 (2011).
Musci, G., Polticelli, F. & Bonaccorsi di Patti, M. C. Ceruloplasmin-ferroportin system of iron traffic in vertebrates. World J. Biol. Chem. 5, 204–215 (2014).
Prohaska, J. R. Changes in tissue growth, concentrations of copper, iron, cytochrome oxidase and superoxide dismutase subsequent to dietary or genetic copper deficiency in mice. J. Nutr. 113, 2048–2058 (1983).
Patel, B. N. et al. Ceruloplasmin regulates iron levels in the CNS and prevents free radical injury. J. Neurosci. 22, 6578–6586 (2002).
Ozawa, H. et al. Renal function in patients with Menkes disease. Eur. J. Pediatr. 162, 51–52 (2003).
Mann, J. R. et al. Copper metabolism in mottled mouse mutants: copper therapy of brindled (Mobr) mice. Biochem J. 180, 605–612 (1979).
Camakaris, J., Mann, J. R. & Danks, D. M. Copper metabolism in mottled mouse mutants: copper concentrations in tissues during development. Biochem J. 180, 597–604 (1979).
Darwich, A. S. et al. Meta-analysis of the turnover of intestinal epithelia in preclinical animal species and humans. Drug Metab. Dispos. 42, 2016–2022 (2014).
Fry, R. S. et al. Amount and source of dietary copper affects small intestine morphology, duodenal lipid peroxidation, hepatic oxidative stress, and mRNA expression of hepatic copper regulatory proteins in weanling pigs. J. Anim. Sci. 90, 3112–3119 (2012).
Yoshii, Y. et al. Controlled administration of penicillamine reduces radiation exposure in critical organs during 64Cu-ATSM internal radiotherapy: a novel strategy for liver protection. PLoS ONE 9, e86996 (2014).
Hedemann, M. S., Jensen, B. B. & Poulsen, H. D. Influence of dietary zinc and copper on digestive enzyme activity and intestinal morphology in weaned pigs. J. Anim. Sci. 84, 3310–3320 (2006).
Acknowledgements
We thank Yukari Takase, Yuko Hino, Tomoyo Yamanobe, Kumiko Kurosaki, Yoko Chiba, Kumi Itoh, Tomoko Hiroki, and Masashi Funakoshi for providing technical assistance. We also acknowledge the support of the Animal Pathology Platform at the Biomedical Research Core of Tohoku University Graduate School of Medicine. This research was supported by a Grant-in-Aid for Scientific Research to Mitsutoshi Munakata from The Ministry of Education, Culture, Sports, Science and Technology of Japan (16K09959).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Munakata, M., Kodama, H., Tani, N. et al. Menkes disease: Oral administration of glyoxal-bis(N(4)-methylthiosemicarbazonato)-copper(II) rescues the macular mouse. Pediatr Res 84, 770–777 (2018). https://doi.org/10.1038/s41390-018-0116-7
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-018-0116-7
This article is cited by
-
Pharmacokinetics of CuGTSM, a Novel Drug Candidate, in a Mouse Model of Menkes Disease
Pharmaceutical Research (2021)