Abstract
BACKGROUND
To compare the ability of ventricular morphology on cranial ultrasound (CUS) versus standard clinical variables to predict the need for temporizing cerebrospinal fluid drainage in newborns with intraventricular hemorrhage (IVH).
Method
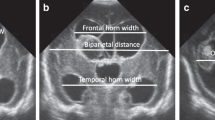
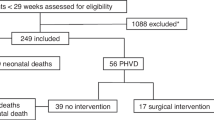
This is a retrospective study of newborns (gestational age <29 weeks) diagnosed with IVH. Clinical variables known to increase the risk for post-hemorrhagic hydrocephalus were collected. The first CUS with IVH was identified and a slice in the coronal plane was selected. The frontal horns of the lateral ventricles were manually segmented. Automated quantitative morphological features were extracted from both lateral ventricles. Predictive models of the need of temporizing intervention were compared.
Results
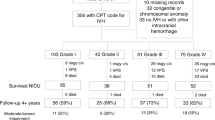
Sixty-two newborns met inclusion criteria. Fifteen out of the 62 had a temporizing intervention. The morphological features had a better accuracy predicting temporizing interventions when compared to clinical variables: 0.94 versus 0.85, respectively; p < 0.01 for both. By considering both morphological and clinical variables, our method predicts the need of temporizing intervention with positive and negative predictive values of 0.83 and 1, respectively, and accuracy of 0.97.
Conclusion
Early cranial ultrasound-based quantitative ventricular evaluation in premature newborns can predict the eventual use of a temporizing intervention to treat post-hemorrhagic hydrocephalus. This may be helpful for early monitoring and treatment.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Radic, J. A., Vincer, M. & McNeely, P. D. Outcomes of intraventricular hemorrhage and posthemorrhagic hydrocephalus in a population-based cohort of very preterm infants born to residents of Nova Scotia from 1993 to 2010. J. Neurosurg. Pediatr. 15, 580–588 (2015).
Papile, L. A. et al. Posthemorrhagic hydrocephalus in low-birth-weight infants: treatment by serial lumbar punctures. J. Pediatr. 97, 273–277 (1980).
Del Bigio, M. R., Kanfer, J. N. & Zhang, Y. W. Myelination delay in the cerebral white matter of immature rats with kaolin-induced hydrocephalus is reversible. J. Neuropathol. Exp. Neurol. 56, 1053–1066 (1997).
Del Bigio, M. R., Wilson, M. J. & Enno, T. Chronic hydrocephalus in rats and humans: white matter loss and behavior changes. Ann. Neurol. 53, 337–346 (2003).
Strahle, J. et al. Mechanisms of hydrocephalus after neonatal and adult intraventricular hemorrhage. Transl. Stroke Res. 3(Suppl 1), 25–38 (2012).
Sarkar, S. et al. Screening cranial imaging at multiple time points improves cystic periventricular leukomalacia detection. Am. J. Perinatol. 32, 973–979 (2015).
Ment, L. R. et al. Practice parameter: neuroimaging of the neonate: report of the Quality Standards Subcommittee of the American Academy of Neurology and the Practice Committee of the Child Neurology Society. Neurology 58, 1726–1738 (2002).
Davies, M. W. et al. Reference ranges for the linear dimensions of the intracranial ventricles in preterm neonates. Arch. Dis. Child. Fetal Neonatal Ed. 82, F218–F223 (2000).
Srinivasakumar, P. et al. Posthemorrhagic ventricular dilatation-impact on early neurodevelopmental outcome. Am. J. Perinatol. 30, 207–214 (2013).
Riva-Cambrin, J. et al. Center effect and other factors influencing temporization and shunting of cerebrospinal fluid in preterm infants with intraventricular hemorrhage. J. Neurosurg. Pediatr. 9, 473–481 (2012).
Randomised trial of early tapping in neonatal posthaemorrhagic ventricular dilatation. Ventriculomegaly Trial Group. Arch. Dis. Childhood. 65(1 Spec No), 3–10 (1990).
de Vries, L. S. et al. Treatment thresholds for intervention in posthaemorrhagic ventricular dilation: a randomised controlled trial. Arch. Dis. Child. Fetal Neonatal Ed. https://doi.org/10.1136/archdischild-2017-314206 (2018).
Momjian, S. & Bichsel, D. Nonlinear poroplastic model of ventricular dilation in hydrocephalus. J. Neurosurg. 109, 100–107 (2008).
Tabrizi, P. R. et al. Cranial ultrasound-based prediction of post hemorrhagic hydrocephalus outcome in premature neonates with intraventricular hemorrhage. IEEE Eng. Med. Biol. Soc. Annu. Conf. 2017, 169–172 (2017).
Adams-Chapman, I. et al. Neurodevelopmental outcome of extremely low birth weight infants with posthemorrhagic hydrocephalus requiring shunt insertion. Pediatrics 121, e1167–e1177 (2008).
Klinger, G. et al. Risk factors associated with post-hemorrhagic hydrocephalus among very low birth weight infants of 24-28 weeks gestation. J. Perinatol. 36, 557–563 (2016).
Radic, J. A., Vincer, M. & McNeely, P. D. Temporal trends of intraventricular hemorrhage of prematurity in Nova Scotia from 1993 to 2012. J. Neurosurg. Pediatr. 15, 573–579 (2015).
Levene, M. I. Measurement of the growth of the lateral ventricles in preterm infants with real-time ultrasound. Arch. Dis. Child. 56, 900–904 (1981).
Brouwer, M. J. et al. New reference values for the neonatal cerebral ventricles. Radiology 262, 224–233 (2012).
Fabijańska, A. et al. Assessment of hydrocephalus in children based on digital image processing and analysis. Int. J. Appl. Math. Comput. Sci. 24, 299–312 (2014).
Kovalevsky, V. Curvature in digital 2D images. Int. J. Pattern Recognit. Artif. Intell. 15, 1183–1200 (2001).
Cerrolaza, J. J. et al. Quantitative ultrasound for measuring obstructive severity in children with hydronephrosis. J. Urol. 195(Pt 1), 1093–1099 (2016).
Mladeni, D. et al. Feature selection using linear classifier weights: interaction with classification models. In Proc. 27th Annual International ACM SIGIR Conference on Research and Development in Information Retrieval 234–241 (ACM, New York, NY, 2004).
Deng, K. OMEGA: On-line Memory-based General Purpose System Classifier. PhD thesis, Carnegie Mellon Univ. (1998).
Scholkopf, B, & Smola, A. J. Learning with Kernels: Support Vector Machines, Regularization, Optimization, and Beyond (MIT Press, Cambridge, MA, 2002).
Kohavi, R. A study of cross-validation and bootstrap for accuracy estimation and model selection. In Proc. 14th International Joint Conference on Artificial Intelligence - Volume 2 1137–1143 (Morgan Kaufmann Publishers Inc., Burlington, MA, 1995).
DMW, P. Evaluation: from precision, recall and F-measure to ROC, informedness, markedness& correlation. J. Mach. Learn Technol. 2, 37–63 (2011).
Qiu, W. et al. Automatic segmentation approach to extracting neonatal cerebral ventricles from 3D ultrasound images. Med. Image Anal. 35, 181–191 (2017).
McLean, G. et al. Measurement of the lateral ventricles in the neonatal head: comparison of 2-D and 3-D techniques. Ultrasound Med. Biol. 38, 2051–2057 (2012).
Kishimoto, J. et al. Quantitative 3-D head ultrasound measurements of ventricle volume to determine thresholds for preterm neonates requiring interventional therapies following posthemorrhagic ventricle dilatation. J. Med. Imaging (Bellingham) 5, 026001 (2018).
Brann, B. St et al. Measurement of progressive cerebral ventriculomegaly in infants after grades III and IV intraventricular hemorrhages. J. Pediatr. 117, 615–621 (1990).
Mondal, P. et al. A robust method for ventriculomegaly detection from neonatal brain ultrasound images. J. Med. Syst. 36, 2817–2828 (2012).
Bassan, H. et al. Timing of external ventricular drainage and neurodevelopmental outcome in preterm infants with posthemorrhagic hydrocephalus. Eur. J. Paediatr. Neurol. 16, 662–670 (2012).
Acknowledgments
Thank you to Dr. Joseph Piatt MD from the Department of Neurosurgery at Nemours/A. I. DuPont Hospital for Children for his review of this manuscript and his valuable remarks.
Author contributions
R.O. conceptualized and designed the study, acquired the data, performed the technical analysis of the ultrasound images, and drafted the reviewed the manuscript. P.R.T. conceptualized and designed the study, acquired the data, performed the technical analysis of the ultrasound images, and drafted and reviewed the manuscript. She also performed the statistical analysis. M.G.L. helped conceptualizing and designing the study and critically reviewing the manuscript for important intellectual content and final approval of the version to be published. A.A.P. helped conceptualizing and designing the study and critically reviewing the manuscript for important intellectual content and final approval of the version to be published. J.J.C. helped conceptualizing and designing the study and reviewed the manuscript. A.M. helped conceptualizing and designing the study and critically reviewing the manuscript for important intellectual content and final approval of the version to be published. T.C. helped drafting the article and revising it critically for important intellectual content and final approval of the version to be published.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Obeid, R., Tabrizi, P.R., Mansoor, A. et al. Ventricular shape evaluation on early ultrasound predicts post-hemorrhagic hydrocephalus. Pediatr Res 85, 293–298 (2019). https://doi.org/10.1038/s41390-018-0252-0
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-018-0252-0