Abstract
Background
Long-chain polyunsaturated fatty acids (LCPUFAs) play a critical role in neonatal health. We hypothesized that LCPUFAs play an essential role in priming postnatal gut development. We studied the effect of LCPUFAs on postnatal gut development using fat-1 transgenic mice, which are capable of converting n-6 to n-3 LCPUFAs, and wild-type (WT) C57BL/6 mice.
Methods
Distal ileum sections were collected from fat-1 and WT mice on days 3, 14, and 28. Fatty acid analyses, histology, RT-qPCR and intestinal permeability were performed.
Results
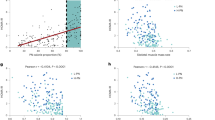
Fat-1 mice, relative to WT mice, showed increased n-3 LCPUFAs levels (α-linolenic acid, docosahexaenoic acid, and eicosapentaenoic acid, p < 0.05) and decreased arachidonic acid levels (p < 0.05) in the ileum. Preweaning fat-1 mice, compared to WT, showed >50% reduced muc2, Tff3, TLR9, and Camp expression (p < 0.05), markers of the innate immune response. There was a >two-fold increased expression of Fzd5 and EphB2, markers of cell differentiation (p < 0.05), and Fabp2 and 6, regulators of fatty acid transport and metabolism (p < 0.05). Despite reduced expression of tight junction genes, intestinal permeability in fat-1 was comparable to WT mice.
Conclusions
Our data support the hypothesis that fatty acid profiles early in development modulate intestinal gene expression in formative domains, such as cell differentiation, tight junctions, other innate host defenses, and lipid metabolism.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Neu, J. & Walker, W. A. Necrotizing enterocolitis. N. Engl. J. Med. 364, 255–264 (2011).
Lin, P. W. & Stoll, B. J. Necrotising enterocolitis. Lancet 368, 1271–1283 (2006).
Tanner, S. M. et al. Pathogenesis of necrotizing enterocolitis: modeling the innate immune response. Am. J. Pathol. 185, 4–16 (2015).
Gribar, S. C. et al. Reciprocal expression and signaling of TLR4 and TLR9 in the pathogenesis and treatment of necrotizing enterocolitis. J. Immunol. 182, 636–646 (2009).
Martin, C. R. et al. Decreased postnatal docosahexaenoic and arachidonic acid blood levels in premature infants are associated with neonatal morbidities. J. Pediatr. 159, 743–749 (2011). e1–2.
Löfqvist, C. A. et al. Association of retinopathy of prematurity with low levels of arachidonic acid: a secondary analysis of a randomized clinical trial. JAMA Ophthalmol. 136, 271–277 (2018).
Marion-Letellier, R., Savoye, G., Beck, P. L., Panaccione, R. & Ghosh, S. Polyunsaturated fatty acids in inflammatory bowel diseases: a reappraisal of effects and therapeutic approaches. Inflamm. Bowel Dis. 19, 650–661 (2013).
Wijendran, V. et al. Long-chain polyunsaturated fatty acids attenuate the IL-1β-induced proinflammatory response in human fetal intestinal epithelial cells. Pediatr. Res. 78, 626–633 (2015).
Ohtsuka, Y. et al. ω-3 fatty acids attenuate mucosal inflammation in premature rat pups. J. Pediatr. Surg. 46, 489–495 (2011).
Lu, J., Jilling, T., Li, D. & Caplan, M. S. Polyunsaturated fatty acid supplementation alters proinflammatory gene expression and reduces the incidence of necrotizing enterocolitis in a neonatal rat model. Pediatr. Res. 61, 427–432 (2007).
Kang, J. X., Wang, J., Wu, L. & Kang, Z. B. Transgenic mice: fat-1 mice convert n-6 to n-3 fatty acids. Nature 427, 504 (2004).
McElroy, S. J. & Weitkamp, J.-H. Innate immunity in the small intestine of the preterm infant. Neoreviews 12, e517–e526 (2011).
Freedman, S. D. et al. A membrane lipid imbalance plays a role in the phenotypic expression of cystic fibrosis in cftr(-/-) mice. Proc. Natl. Acad. Sci. USA 96, 13995–14000 (1999).
Economopoulos, K. P. et al. Prevention of antibiotic-associated metabolic syndrome in mice by intestinal alkaline phosphatase. Diabetes Obes. Metab. 18, 519–527 (2016).
Coorens, M., Scheenstra, M. R., Veldhuizen, E. J. A. & Haagsman, H. P. Interspecies cathelicidin comparison reveals divergence in antimicrobial activity, TLR modulation, chemokine induction and regulation of phagocytosis. Sci. Rep. 7, 40874 (2017).
MMAL, Pelsers, Hermens, W. T. & Glatz, J. F. C. Fatty acid-binding proteins as plasma markers of tissue injury. Clin. Chim. Acta 352, 15–35 (2005).
Furuhashi, M. & Hotamisligil, G. S. Fatty acid-binding proteins: role in metabolic diseases and potential as drug targets. Nat. Rev. Drug Discov. 7, 489–503 (2008).
Ng, E. W. Y. et al. Gut-associated biomarkers L-FABP, I-FABP, and TFF3 and LIT score for diagnosis of surgical necrotizing enterocolitis in preterm infants. Ann. Surg. 258, 1111–1118 (2013).
Li, Y., Wang, X., Li, N. & Li, J. The study of n-3PUFAs protecting the intestinal barrier in rat HS/R model. Lipids Health Dis. 13, 146 (2014).
Wang, X., Pan, L., Lu, J., Li, N. & Li, J. N-3 PUFAs attenuate ischemia/reperfusion induced intestinal barrier injury by activating I-FABP-PPARγ pathway. Clin. Nutr. 31, 951–957 (2012).
Otte, J.-M. et al. Effects of the cathelicidin LL-37 on intestinal epithelial barrier integrity. Regul. Pept. 156, 104–117 (2009).
Rachmilewitz, D. et al. Toll-like receptor 9 signaling mediates the anti-inflammatory effects of probiotics in murine experimental colitis. Gastroenterology 126, 520–528 (2004).
Ii, W. A. R., Sakamoto, K. & Leifer, C. A. TLR9 is important for protection against intestinal damage and for intestinal repair. Sci. Rep. 2, 574 (2012).
Lee, J., Rachmilewitz, D. & Raz, E. Homeostatic effects of TLR9 signaling in experimental colitis. Ann. NY Acad. Sci. 1072, 351–355 (2006).
Jiang, W. et al. Differential regulation of human cathelicidin LL-37 by free fatty acids and their analogs. Peptides 50, 129–138 (2013).
Lee, J. et al. Maintenance of colonic homeostasis by distinctive apical TLR9 signalling in intestinal epithelial cells. Nat. Cell Biol. 8, 1327–1336 (2006).
Taylor, S. N., Basile, L. A., Ebeling, M. & Wagner, C. L. Intestinal permeability in preterm infants by feeding type: mother’s milk versus formula. Breastfeed. Med. 4, 11–15 (2009).
Moore, S. A. et al. Intestinal barrier dysfunction in human necrotizing enterocolitis. J. Pediatr. Surg. 51, 1907–1913 (2016).
Usami, M. et al. Effect of eicosapentaenoic acid (EPA) on tight junction permeability in intestinal monolayer cells. Clin. Nutr. 20, 351–359 (2001).
Willemsen, L. E. M. et al. Polyunsaturated fatty acids support epithelial barrier integrity and reduce IL-4 mediated permeability in vitro. Eur. J. Nutr. 47, 183–191 (2008).
Beguin, P., Errachid, A., Larondelle, Y. & Schneider, Y.-J. Effect of polyunsaturated fatty acids on tight junctions in a model of the human intestinal epithelium under normal and inflammatory conditions. Food Funct. 4, 923 (2013).
Pendyala, S., Walker, J. M. & Holt, P. R. A high-fat diet is associated with endotoxemia that originates from the gut. Gastroenterology 142, 1100–1.e2 (2012).
Lippestad, M., Hodges, R. R., Utheim, T. P., Serhan, C. N. & Dartt, D. A. Resolvin D1 increases mucin secretion in cultured rat conjunctival goblet cells via multiple signaling pathways. Invest. Ophthalmol. Vis. Sci. 58, 4530–4544 (2017).
Zhao, J. et al. Preferential generation of 15-HETE-PE induced by IL-13 regulates goblet cell differentiation in human airway epithelial cells. Am. J. Respir. Cell Mol. Biol. 57, 692–701 (2017).
Phillips, T. E., Stenson, W. F. & Neutra, M. R. Lipoxygenase metabolites of arachidonic acid do not induce mucus secretion from rabbit intestinal goblet cells in vitro. Prostaglandins Leukot. Essent. Fat. Acids 37, 51–55 (1989).
Najm, S. et al. Effects of a lipid emulsion containing fish oil on polyunsaturated fatty acid profiles, growth and morbidities in extremely premature infants: a randomized controlled trial. Clin. Nutr. ESPEN 20, 17–23 (2017).
Yu, H.-N. et al. Effects of fish oil with a high content of n-3 polyunsaturated fatty acids on mouse gut microbiota. Arch. Med. Res. 45, 195–202 (2014).
Ghosh, S. et al. Fish oil attenuates omega-6 polyunsaturated fatty acid-induced dysbiosis and infectious colitis but impairs LPS dephosphorylation activity causing sepsis. PLoS ONE 8, e55468 (2013).
Acknowledgements
We are grateful to Dr. Jing X. Kang (Massachusetts General Hospital, Boston, MA) for providing us the fat-1 transgenic mice. Our study was supported by Charles H. and Judy Hood Family Infant Health Research Program and NIH R01 DK104346.
Author contributions
Substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data: all the authors. Drafting the article or revising it critically for important intellectual content: P.S., C.R.M., S.D.F. and G.P. Final approval of the version to be published. P.S., C.R.M., and S.D.F.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Singh, P., Ochoa-Allemant, P., Brown, J. et al. Effect of polyunsaturated fatty acids on postnatal ileum development using the fat-1 transgenic mouse model. Pediatr Res 85, 556–565 (2019). https://doi.org/10.1038/s41390-019-0284-0
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-019-0284-0
This article is cited by
-
Human placenta mesenchymal stromal cells alleviate intestinal inflammation and repair intestinal barrier function by activating AMPK-FXR pathway
Communications Biology (2025)
-
Single-step genome-wide association study for carcass quality traits in Angus beef cattle
Tropical Animal Health and Production (2025)