Abstract
Background
This study aimed to determine the accuracy of a point-of-care Bilistick method for measuring total serum bilirubin (TSB) and its turn-around-time (TAT) against hospital laboratory methods.
Methods
This prospective study was carried out on 561 term-gestation jaundiced neonates in two Malaysian hospitals. Venous blood sample was collected from each neonate for contemporary measurement of TSB by hospital laboratories and Bilistick. TAT was the time interval between specimen collection and TSB result reported by each method.
Results
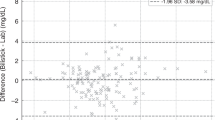
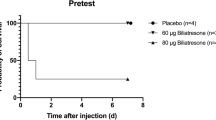
The mean laboratory-measured TSB was 194.85 (±2.844) µmol/L and Bilistick TSB was 169.37 (±2.706) µmol/L. Pearson’s correlation coefficient was: r = 0.901 (p < 0.001). The mean difference of [laboratory TSB− Bilistick TBS] was 26.48 (±29.41) µmol/L. The Bland–Altman plots show that the 95% limits of agreement (−31.1577, 84.11772) contain 94.7% (=531/561) of the difference in TSB readings. Bilistick has a 99% accuracy and 100% sensitivity to predict laboratory TSB levels of ≥80 µmol/L and ≥360 µmol/L at lower Bilistick TSB levels of ≥55 and ≥315 µmol/L, respectively. TAT of Bilistick TSB (2.0 min) was significantly shorter than TAT (105 min) of laboratory TSB (p < 0.001).
Conclusions
Bilistick has shorter TAT. The accuracy and sensitivity of Bilistick TSB for predicting laboratory TSB is high at lower cutoff levels.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Watchko, J. F. Kernicterus and the molecular mechanisms of bilirubin-induced CNS injury in newborns. Neuromolecular Med. 8, 513–529 (2006).
Hameed, N. N., Na’Ma, A. M., Vilms, R. & Bhutani, V. K. Severe neonatal hyperbilirubinemia and adverse short-term consequences in Baghdad, Iraq. Neonatology 100, 57–63 (2011).
Slusher, T. M. et al. Glucose-6-phospahte dehydrogenase deficiency and carboxyhemoglobin concentration associated with bilirubin-related morbidity and death in Nigerian infants. J. Pediatr. 126, 102–108 (1995).
Palmela, I. et al. Elevated levels of bilirubin and long-term exposure impair human brain microvascular endothelial cell integrity. Curr. Neurovasc. Res. 8, 153–169 (2011).
Watchko, J. F. & Tiribelli, C. Bilirubin-induced neurologic damage-mechanisms and management approaches. N. Engl. J. Med. 369, 2021–2030 (2013).
Mreihil, K., McDonagh, A. F., Nakstad, B. & Hansen, T. W. Early isomerization of bilirubin in phototherapy of neonatal jaundice. Pediatr. Res. 67, 656–659 (2010).
Maisels, M. J. et al. Hyperbilirubinemia in the newborn infants≥35 weeks’ gestation: an update with clarifications. Pediatrics 124, 1193–1198 (2009).
Coda Zabetta, C. D. et al. Bilistick: a low-cost point-of care system to measure total plasma bilirubin. Neonatology 103, 176–180 (2013).
Division of Family Health Development, Ministry of Health of Malaysia. Integrated plan for detection and management of neonatal jaundice, 2017 (2nd Revision). Available at https://mpaeds.my/integrated-plan-for-detection-management-of-neonatal-jaundice/ Accessed 26 September 2018.
Management of neonatal jaundice: Clinical practice guidelines, 2nd edn (Ministry of Health of Malaysia, 2014). MOH/P/PAK/278.14(GU).
Charan, J. & Biswas, T. How to calculate sample size for different study designs in medical research? Indian J. Psychol. Med. 35, 121–126 (2013).
Fawcett, T. An introduction to ROC analysis. Pattern Recognit. Lett. 27, 861–874 (2006).
Thielemans, L. et al. Laboratory validation and field usability assessment of point-of-care test for serum bilirubin levels in neonates in a tropical setting. Wellocme Open Res. 3, 110 (2018).
Greco, C., et al. Diagnostic performance analysis of the point-of-care Bilistick System in identifying severe neonatal hyperbilirubinemia by a multi-country approach. EClinicalMedicine 1, 14–20 (2018).
Horn, A. R. et al. Phototherapy and exchange transfusion for neonatal hyperbilirubinemia. S. Afr. Med. J. 96, 819–824 (2006).
Olusanya, B. O., et al. Management of late-preterm and term infants with hyperbilirubinemia in resource-constrained settings. BMC Pediatr. 15, 39 (2015).
Acknowledgements
We thank the Director General of the Ministry of Health of Malaysia for giving us the permission to publish these findings, and the following doctors in Ampang Hospital and Selayang Hospital for helping us to recruit some of the patients: Li Lian Boey, Tow Swan Chiam, Koon Hau Chong, Chin Yee Chuah, Kevin Chin Zhi En, Chyi Chyi Khoo, Laavania Ganesapiran, Soon Yap Lee, Maizatul Akmar Musa, Bee Hong Tan, Eng Teck Tan, Tze Hau Yeoh, Umar Mohd Rais, Priya Lakshmy Balasubramanium, Hana Guee, and Nethiya Vengataraman. This project was funded by a research grant from the Universiti Tunku Abdul Rahman of Malaysia (Project number: IPSR/RMC/UTARRF/2016-C2/B01).
Author information
Authors and Affiliations
Contributions
N.Y.B.: conceptualized and planed the study, analyzed the data, and prepared the manuscript. Y.F.C.: participated in planning the study, analyzed the data, and reviewed the manuscript. Y.X.L.: recruited patients in Selayang Hospital, keyed in the data, and reviewed the manuscript. Z.Y.T.: recruited patients in the Ampang Hospital, keyed in the data, and reviewed the manuscript. L.C.H.: recruited patients in the Ampang Hospital, helped keyed in some of the data, and reviewed the manuscript. S.C.C. and Z.A.L..: participated in planning the study, supervised the recruitment of patients in the Selayang Hospital, are responsible for the validity of the data, and reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Financial support
This project was funded by a research grant from the Universiti Tunku Abdul Rahman of Malaysia (Project number: IPSR/RMC/UTARRF/2016-C2/B01).
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Boo, NY., Chang, YF., Leong, YX. et al. The point-of-care Bilistick method has very short turn-around-time and high accuracy at lower cutoff levels to predict laboratory-measured TSB. Pediatr Res 86, 216–220 (2019). https://doi.org/10.1038/s41390-019-0304-0
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41390-019-0304-0
This article is cited by
-
Diagnostic methods for neonatal hyperbilirubinemia: benefits, limitations, requirements, and novel developments
Pediatric Research (2021)
-
Commentary on “The point-of-care Bilistick method has very short turn-around-time and high accuracy at lower cut-off levels to predict laboratory-measured TSB.”
Pediatric Research (2019)