Abstract
Background
We investigated a costimulatory molecule OX40–OX40L acting as an upstream regulator to regulate the nuclear factor of activated T cell (NFAT) in the acute phase of Kawasaki disease (KD).
Methods
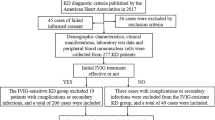
One hundred and one samples were collected and divided into six groups: coronary artery lesion (KD-CAL) before intravenous immunoglobulin (IVIG), KD-CAL after IVIG, KD without CAL (KD-nCAL) before IVIG, KD-nCAL after IVIG, fever of unknown (Fou), and Healthy. In vitro OX40-stimulating and OX40L-inhibiting tests were conducted in Healthy and KD groups, respectively. Both the messenger RNA (mRNA) and protein expression levels of OX40, OX40L, NFAT1, and NFAT2 were investigated using quantitative reverse transcription PCR and immunoblotting assay, respectively.
Results
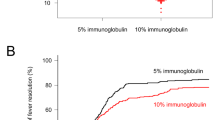
The mRNA and protein expression levels of NFAT1, NFAT2, OX40, and OX40L were significantly increased in KD-CAL and KD-nCAL groups before IVIG compared with Fou and Healthy groups and decreased after IVIG. A positive correlation was found between them in KD. In vitro OX40-stimulating test demonstrated the significantly increased mRNA and protein expression levels of NFAT1 and NFAT2 in the peripheral blood mononuclear cells of the Healthy group. Meanwhile, OX40L-inhibiting test showed significantly decreased expression levels of NFAT1 and NFAT2 in the KD group.
Conclusion
OX40–OX40L acts as an upstream regulator in the NFAT signaling pathway involved in KD.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Saguil, A., Fargo, M. & Grogan, S. Diagnosis and management of kawasaki disease. Am. Fam. Physician 91, 365–371 (2015).
Dietz, S. M. et al. Dissecting Kawasaki disease: a state-of-the-art review. Eur. J. Pediatr. 176, 995–1009 (2017).
McCrindle, B. W. et al. American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee of the Council on Cardiovascular Disease in the Young; Council on Cardiovascular and Stroke Nursing; Council on Cardiovascular Surgery and Anesthesia; and Council on Epidemiology and Prevention. Diagnosis, Treatment, and Long-Term Management of Kawasaki Disease: A Scientific Statement for Health Professionals From the American Heart Association. Circulation 135, e927–e999 (2017).
Pilania, R. K., Bhattarai, D. & Singh, S. Controversies in diagnosis and management of Kawasaki disease. World J. Clin. Pediatr. 7, 27–35 (2018).
Newburger, J. W., Takahashi, M. & Burns, J. C. Kawasaki disease. J. Am. Coll. Cardiol. 67, 1738–1749 (2016).
Kuo, H. C. et al. Wireless optical monitoring system dentifies limb induration characteristics in Kawasaki disease. J Allergy Clin. Immunol. pii: S0091-6749(18)30631-6 (2018).
Lv, Y. W. et al. Understanding the pathogenesis of Kawasaki disease by network and pathway analysis. Comput. Math. Methods Med. 2013, 989307 (2013).
Kim, K. Y. et al. ITPKC and SLC11A1 gene polymorphisms and gene–gene interactions in Korean patients with Kawasaki disease. Yonsei. Med. J. 59, 119–127 (2018).
Khor, C. C. et al. Genome-wide association study identifies FCGR2A as a susceptibility locus for Kawasaki disease. Nat. Genet. 43, 1241–1246 (2011).
Onouchi, Y. et al. A genome-wide association study identifies three new risk loci for Kawasaki disease. Nat. Genet. 44, 517–521 (2012).
Onouchi, Y. The genetics of Kawasaki disease. Int J. Rheum. Dis. 21, 26–30 (2018).
Renauer, P., Coit, P. & Sawalha, A. H. Epigenetics and vasculitis: a comprehensive review. Clin. Rev. Allergy Immunol. 50, 357–366 (2016).
Lee, J. U., Kim, L. K. & Choi, J. M. Revisiting the concept of targeting NFAT to control T cell immunity and autoimmune diseases. Front. Immunol. 9, 2747 (2018).
Chang, Y. K. et al. Association of BANK1 and TNFSF4 with systemic lupus erythematosus in Hong Kong Chinese. Genes Immun. 10, 414–420 (2009).
Nuebling, T. et al. The immune checkpoint modulator OX40 and its ligand OX40L in NK-cell immunosurveillance and acute myeloid leukemia. Cancer Immunol. Res. 6,209-221 (2018)
Jin-chuan, Y. OX40-OX40L interaction promotes proliferation and activation of lymphocytes via NFATc1 in ApoE-deficient mice. PLoS ONE 8, e60854 (2013).
Yan, J., Wang, C., Du, R., Liu, P. & Chen, G. OX40-OX40L ligand interaction may activate phospholipase C signal transduction pathway in human umbilical vein endothelial cells. Chem. Biol. Interact. 180, 460–464 (2009).
Wang, W. et al. The roles of Ca2 +/NFAT signaling genes in Kawasaki disease: single- and multiple-risk genetic variants. Sci. Rep. 6, 5208 (2014).
Onouchi, Y. et al. ITPKC functional polymorphism associated with Kawasaki disease susceptibility and formation of coronary artery aneurysms. Nat. Genet. 40, 35–42 (2008).
Li, P. et al. PPP3CC feedback regulates IP3-Ca2 + pathway through preventing ITPKC degradation. Front Biosci. (Landmark Ed.) 18, 919–927 (2013).
Onouchi, Y. et al. Variations in ORAI1 gene associated with Kawasaki disease. PLoS ONE 11, e0145486 (2016).
Burns, J. C. et al. Found in translation: international initiatives pursuing interleukin-1 blockade for treatment of acute Kawasaki disease. Arthritis Rheumatol. 69, 268–276 (2017).
Wakita, Daiko et al. The role of IL-1 signaling in a mouse model of Kawasaki disease-associated abdominal aortic aneurysm. Arterioscler. Thromb. Vasc. Biol. 36, 886–897 (2016).
Lee, Y. et al. Interleukin-1β is crucial for the induction of coronary artery inflammation in a mouse model of Kawasaki disease. Circulation 125, 1542–1550 (2012).
Alphonse, M. P. et al. Response in Kawasaki disease inflammasome activation and treatment inositol-triphosphate 3-kinase C mediates. J. Immunol. 197, 3481–3489 (2016).
Adcock, I. M., Caramori, G. & Chung, K. F. New targets for drug development in asthma. Lancet 372, 1073–1087 (2008).
Hanania, N. A. Targeting airway inflammation in asthma: current and future therapies. Chest 133, 989–998 (2008).
Cavanagh, M. M. & Hussell, T. Is it wise to target the late costimulatory molecule OX40 as a therapeutic target? Arch. Immunol. Ther. Exp. (Warsz.) 56, 291–297 (2008).
Fujita et al. Functional characterization of OX40 expressed on human CD8+ T cells. Immunol. Lett. 106, 27–33 (2006).
So, T., Lee, S. W. & Croft, M. Immune regulation and control of regulatory T cells by OX40 and 4-1BB. Cytokine Growth Factor Rev. 19, 253–262 (2008).
Marschner, A. et al. CpG ODN enhance antigen-specific NKT cell activation via plasmacytoid dendritic cells. Eur. J. Immunol. 35, 2347–2357 (2005).
Zaini, J. et al. OX40 ligand expressed by DCs costimulates NKT and CD4+ Th cell antitumor immunity in mice. J. Clin. Invest. 117, 3330–3338 (2007).
Croft, M., So, T. & duan, W. The significance of OX40 and OX40L to T-cell biology and immune disease. Immunol. Rev. 229, 173–191 (2009).
Beier, K. C., Kallinich, T. & Hamelmann, E. Master switches of T-cell activation and differentiation. Eur. Respir. J. 29, 804–812 (2007).
Jin-chuan, Y. et al. Effects of OX40–OX40L interaction on the nuclear factor of activated T cells c1 in ApoE-deficient mice. Inflammation 37, 205–213 (2014).
Latza, U. et al. The human OX40 homolog: eDNA structure, expression and chromosomal assignment of the ACT35 antigen. Eur. J. Immunol. 24, 677–683 (1994).
Mallett, S., Fossum, S. & Barclay, A. N. Characterization of the MRC OX40 antigen of activated CD4 positive T lymphocytes-a molecule related to nerve growth factor receptor. EMBO J. 9, 1063–1068 (1990).
Acknowledgements
This work was supported by the grants from the National Natural Science Foundation of China (Nos. 81570455, 31600695, and 8187021691), the Natural Science Foundation of Young (Nos. 81600391, 81400222, 81570439, and 81800437), the Jiangsu Province Science Foundation (No. BE2017660), the Talent Foundation of Jiangsu Province (No. WSN-070 and ZDRCA2016049), the Jiangsu Provincial Medical Young Talents (QNRC2016756 and QNRC2016764), the Universities Natural Science Foundation of Jiangsu Province (16KJB310014), and the Applied Foundational Research of Medical and Health Care of Suzhou City (SYS201642 and SYS201633).
Author information
Authors and Affiliations
Contributions
Y.-W.L. carried out the studies and wrote the paper and Y.C. participated in its design and wrote the paper. H.-T.L. helped to design the manuscript and wrote the paper. X.L., Y.-J.T., W.-G.Q., Q.-Q.X., and L.S. participated in the collection of clinical cases. G.-H.Q., as the co-corresponding author, participated in the experimental process. Y.-Y.D., as the first corresponding author, participated in the design of the whole study and wrote the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lv, YW., Chen, Y., Lv, HT. et al. Kawasaki disease OX40–OX40L axis acts as an upstream regulator of NFAT signaling pathway. Pediatr Res 85, 835–840 (2019). https://doi.org/10.1038/s41390-019-0312-0
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41390-019-0312-0
This article is cited by
-
Chrysin improves endothelial inflammation via the NFAT pathway in Kawasaki disease
Molecular Biology Reports (2025)