Abstract
Background
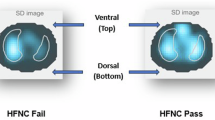
Nasal continuous positive airway pressure (NCPAP) and high flow nasal cannula (HFNC) are modes of non-invasive respiratory support commonly used after extubation in extremely preterm infants. However, the cardiorespiratory physiology of these infants on each mode is unknown.
Methods
Prospective, randomized crossover study in infants with birth weight ≤1250 g undergoing their first extubation attempt. NCPAP and HFNC were applied randomly for 45 min each, while ribcage and abdominal movements, electrocardiogram, oxygen saturation, and fraction of inspired oxygen (FiO2) were recorded. Respiratory signals were analyzed using an automated method, and differences between NCPAP and HFNC features and changes in FiO2 were analyzed.
Results
A total of 30 infants with median [interquartile range] gestational age of 27 weeks [25.7, 27.9] and birth weight of 930 g [780, 1090] were studied. Infants were extubated at 5 days [2, 13] of life with 973 g [880, 1170] and three failed (10%). No differences in cardiorespiratory behavior were noted, except for longer respiratory pauses (9.2 s [5.0, 11.5] vs. 7.3 s [4.6, 9.3]; p = 0.04) and higher FiO2 levels (p = 0.02) during HFNC compared to NCPAP.
Conclusions
In extremely preterm infants studied shortly after extubation, the use of HFNC was associated with longer respiratory pauses and higher FiO2 requirements.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Ferguson, K. N., Roberts, C. T., Manley, B. J. & Davis, P. G. Interventions to improve rates of successful extubation in preterm infants: a systematic review and meta-analysis. JAMA Pediatr. 171, 165–174 (2017).
Al-Mandari, H. et al. International survey on periextubation practices in extremely preterm infants. Arch. Dis. Child. Fetal Neonatal Ed. 100, F428–F431 (2015).
Gupta, S. & Donn, S. M. Continuous positive airway pressure: physiology and comparison of devices. Semin. Fetal Neonatal Med. 21, 204–211 (2016).
Dysart, K. C. Physiologic basis for nasal continuous positive airway pressure, heated and humidified high-flow nasal cannula, and nasal ventilation. Clin. Perinatol. 43, 621–631 (2016).
Manley, B. J. & Owen, L. S. High-flow nasal cannula: mechanisms, evidence and recommendations. Semin. Fetal Neonatal Med. 21, 139–145 (2016).
Wilkinson, D., Andersen, C., O’Donnell, C. P., De Paoli, A. G. & Manley, B. J. High flow nasal cannula for respiratory support in preterm infants. Cochrane Database Syst. Rev. 2, CD006405 (2016).
Saslow, J. G. et al. Work of breathing using high-flow nasal cannula in preterm infants. J. Perinatol. 26, 476–480 (2006).
Shetty, S., Sundaresan, A., Hunt, K., Desai, P. & Greenough, A. Changes in the use of humidified high flow nasal cannula oxygen. Arch. Dis. Child. Fetal Neonatal Ed. 101, F371–F372 (2016).
Lavizzari, A. et al. Respiratory mechanics during NCPAP and HHHFNC at equal distending pressures. Arch. Dis. Child. Fetal neonatal Ed. 99, F315–F320 (2014).
Sreenan, C., Lemke, R. P., Hudson-Mason, A. & Osiovich, H. High-flow nasal cannulae in the management of apnea of prematurity: a comparison with conventional nasal continuous positive airway pressure. Pediatrics 107, 1081–1083 (2001).
Manley, B. J. Nasal high-flow therapy for preterm infants. Clin. Perinatol. 43, 673–691 (2016).
Robles-Rubio, C. A., Brown, K. A. & Kearney, R. E. Automated unsupervised respiratory event analysis. Conf Proc IEEE Eng Med Biol Soc. 2011, 3201–3204 (2011).
Precup, D. et al. Prediction of extubation readiness in extreme preterm infants based on measures of cardiorespiratory variability. Conf Proc IEEE Eng Med Biol Soc. 2012, 5630–5633 (2012).
Robles-Rubio, C. A. et al. Automated analysis of respiratory behavior in extremely preterm infants and extubation readiness. Pediatr Pulmonol. 50, 479–486 (2015).
Robles-Rubio, C. A., Brown, K. A. & Kearney, R. E. A new movement artifact detector for photoplethysmographic signals. Conf Proc IEEE Eng Med Biol Soc. 2013, 2295–2299 (2013).
de Jongh, B. E. et al. Work of breathing indices in infants with respiratory insufficiency receiving high-flow nasal cannula and nasal continuous positive airway pressure. J. Perinatol. 34, 27–32 (2014).
Campbell, D. M., Shah, P. S., Shah, V. & Kelly, E. N. Nasal continuous positive airway pressure from high flow cannula versus infant flow for preterm infants. J. Perinatol. 26, 546–549 (2006).
Manley, B. J., Doyle, L. W., Owen, L. S. & Davis, P. G. Extubating extremely preterm infants: predictors of success and outcomes following failure. J. Pediatr. 173, 45–49 (2016).
Acknowledgements
We are indebted to the babies and their families for their consent to participate in this study. L.J.K., R.E.K., K.A.B., and G.S.A. were funded by the Canadian Institutes of Health Research. L.J.K. was also funded by the Natural Sciences and Engineering Research Council of Canada. K.A.B. was also funded by the Queen Elizabeth Hospital of Montreal Foundation Chair in Pediatric Anesthesia. The funding bodies had no role in the design, collection, analysis, or interpretation of the data.
Author information
Authors and Affiliations
Contributions
L.J.K. contributed to the development of the protocol and study design, assisted in acquiring the recordings, analyzed the data, and wrote the manuscript. W.S. participated in the development of the protocol and study design, and was responsible for patient screening, enrollment, data collection, and recordings. S.L. assisted in patient screening, enrollment, data collection, and recordings. S.R. assisted in patient screening, enrollment, data collection, and recordings. K.A.B. participated in the development of the protocol, and provided critical input into study design, data analyses, and writing of the manuscript. R.E.K. participated in the development of the protocol, and provided critical input into study design, data analyses, and writing of the manuscript. G.M.S. supervised the design and execution of the study, and provided critical input into the final data analyses, and writing of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kanbar, L.J., Shalish, W., Latremouille, S. et al. Cardiorespiratory behavior of preterm infants receiving continuous positive airway pressure and high flow nasal cannula post extubation: randomized crossover study. Pediatr Res 87, 62–68 (2020). https://doi.org/10.1038/s41390-019-0494-5
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41390-019-0494-5
This article is cited by
-
Changes in lung aeration with high-flow nasal cannula compared to nasal CPAP in preterm infants
Journal of Perinatology (2025)
-
Automated prediction of extubation success in extremely preterm infants: the APEX multicenter study
Pediatric Research (2023)
-
Adjustment of high flow nasal cannula rates using real-time work of breathing indices in premature infants with respiratory insufficiency
Journal of Perinatology (2021)
-
Continuous positive airway pressure and high flow nasal cannula: the search for effectiveness continues
Pediatric Research (2020)