Abstract
Background
Neonatal intensive care practices have resulted in marked improvements in the survival of premature infants; however, they remain at significant risk for adverse neurodevelopmental outcomes. The impact of current nutritional practices on brain development following early extra-uterine exposure in premature infants is not well known.
Methods
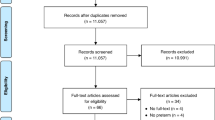
We performed a systematic review to investigate nutritional effects on postnatal brain development in healthy term and prematurely born infants utilizing advanced magnetic resonance imaging tools.
Results
Systematic screen yielded 595 studies for appraisal. Of these, 22 total studies were selected for inclusion in the review, with findings summarized in a qualitative, descriptive fashion.
Conclusion
Fat and energy intake are associated with improved brain volume and development in premature infants. While breast milk intake and long-chain polyunsaturated fatty acid supplementation has been proven beneficial in term infants, the impact in preterm infants is less well understood.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Aarnoudse-Moens, C. S., Weisglas-Kuperus, N., van Goudoever, J. B. & Oosterlaan, J. Meta-analysis of neurobehavioral outcomes in very preterm and/or very low birth weight children. Pediatrics 124, 717–728 (2009).
Sammallahti, S. et al. Nutrition after preterm birth and adult neurocognitive outcomes. PLoS ONE 12, e0185632 (2017).
Walker, S. M. Biological and neurodevelopmental implications of neonatal pain. Clin. Perinatol. 40, 471–491 (2013).
Patra, A., Huang, H., Bauer, J. A. & Giannone, P. J. Neurological consequences of systemic inflammation in the premature neonate. Neural Regen. Res. 12, 890–896 (2017).
Lu, J. & Claud, E. C. Connection between gut microbiome and brain development in preterm infants. Dev. Psychobiol. 15, 739–751 (2019).
Franz, A. R. et al. Intrauterine, early neonatal, and postdischarge growth and neurodevelopmental outcome at 5.4 years in extremely preterm infants after intensive neonatal nutritional support. Pediatrics 123, e101–e109 (2009).
Schneider, N. & Garcia-Rodenas, C. L. Early nutritional interventions for brain and cognitive development in preterm infants: A review of the literature. Nutrients 9, E187 (2017).
Keunen, K., van Elburg, R. M., van Bel, F. & Benders, M. J. Impact of nutrition on brain development and its neuroprotective implications following preterm birth. Pediatr. Res. 77, 148–155 (2015).
Anderson, P. J., Cheong, J. L. & Thompson, D. K. The predictive validity of neonatal MRI for neurodevelopmental outcome in very preterm children. Semin. Perinatol. 39, 147–158 (2015).
Rose, J. et al. Neonatal brain microstructure correlates of neurodevelopment and gait in preterm children 18–22 mo of age: an MRI and DTI study. Pediatr. Res. 78, 700–708 (2015).
Woodward, L. J., Clark, C. A., Bora, S. & Inder, T. E. Neonatal white matter abnormalities an important predictor of neurocognitive outcome for very preterm children. PLoS ONE 7, e51879 (2012).
Kendall, G. S. et al. White matter NAA/cho and cho/cr ratios at MR spectroscopy are predictive of motor outcome in preterm infants. Radiology 271, 230–238 (2014).
Moher, D., Liberati, A., Tetzlaff, J. & Altman, D. G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J. Surg. 8, 336–341 (2010).
VonVille, H. M. Excel Workbooks for Systematic Reviews (2018). https://shwca.se/Excel-SR-workbooks-guides (2018).
Wells, G. A. et al. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality f Nonrandomised Studies in Meta-analyses (2019). http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
Higgins, J. T. et al. A revised tool for assessing risk of bias in randomized trials. Cochrane Database Syst. Rev. 10, 29–31 (Suppl. 1) (2016).
Hillen, M. A., Medendorp, N. M., Daams, J. G. & Smets, E. M. A. Patient-driven second opinions in oncology: a systematic review. Oncologist 22, 1197–1211 (2017).
Deoni, S. C. et al. Breastfeeding and early white matter development: a cross-sectional study. Neuroimage 82, 77–86 (2013).
Ou, X. et al. Voxel-based morphometry and fMRI revealed differences in brain gray matter in breastfed and milk formula-fed children. Am. J. Neuroradiol. 37, 713–719 (2016).
Kafouri, S. et al. Breastfeeding and brain structure in adolescence. Int. J. Epidemiol. 42, 150–159 (2013).
Ou, X. et al. Sex-specific association between infant diet and white matter integrity in 8-y-old children. Pediatr. Res. 76, 535–543 (2014).
Luby, J. L., Belden, A. C., Whalen, D., Harms, M. P. & Barch, D. M. Breastfeeding and childhood IQ: the mediating role of gray matter volume. J. Am. Acad. Child Adolesc. Psychiatry 55, 367–375 (2016).
Belfort, M. B. et al. Breast milk feeding, brain development, and neurocognitive outcomes: a 7-year longitudinal study in infants born at less than 30 weeks’ gestation. J. Pediatr. 177, 133–139.e1 (2016).
Isaacs, E. B. et al. Impact of breast milk on intelligence quotient, brain size, and white matter development. Pediatr. Res. 67, 357–362 (2010).
Pogribna, U. et al. Perinatal clinical antecedents of white matter microstructural abnormalities on diffusion tensor imaging in extremely preterm infants. PLoS ONE 8, e72974 (2013).
Vasu, V. et al. Preterm nutritional intake and MRI phenotype at term age: a prospective observational study. BMJ Open 4, e005390 (2014).
Schneider, J. et al. Nutrient intake in the first two weeks of life and brain growth in preterm neonates. Pediatrics 141, e20172169 (2018).
Coviello, C. et al. Effects of early nutrition and growth on brain volumes, white matter microstructure, and neurodevelopmental outcome in preterm newborns. Pediatr. Res. 83, 102–110 (2018).
Almaas, A. N. et al. Diffusion tensor imaging and behavior in premature infants at 8 years of age, a randomized controlled trial with long-chain polyunsaturated fatty acids. Early Hum. Dev. 95, 41–46 (2016).
Almaas, A. N. et al. Long-chain polyunsaturated fatty acids and cognition in VLBW infants at 8 years: an RCT. Pediatrics 135, 972–980 (2015).
Lepping, R. J. et al. Long-chain polyunsaturated fatty acid supplementation in the first year of life affects brain function, structure, and metabolism at age nine years. Dev. Psychobiol. 61, 5–16 (2019).
van Wezel-Meijler, G. et al. Dietary supplementation of long-chain polyunsaturated fatty acids in preterm infants: efects on cerebral maturation. Acta Paediatr. 91, 942–950 (2002).
Tam, E. W. et al. Early postnatal docosahexaenoic acid levels and improved preterm brain development. Pediatr. Res. 79, 723–730 (2016).
Beauport, L. et al. Impact of early nutritional intake on preterm brain: a magnetic resonance imaging study. J. Pediatr. 181, 29–36.e1 (2017).
Hansen-Pupp, I. et al. Postnatal decrease in circulating insulin-like growth factor-I and low brain volumes in very preterm infants. J. Clin. Endocrinol. Metab. 96, 1129–1135 (2011).
Isaacs, E. B. et al. The effect of early human diet on caudate volumes and IQ. Pediatr. Res. 63, 308–314 (2008).
Paviotti, G. et al. Higher growth, fat and fat-free masses correlate with larger cerebellar volumes in preterm infants at term. Acta Paediatr. 106, 918–925 (2017).
Strommen, K. et al. Enhanced nutrient supply to very low birth weight infants is associated with improved white matter maturation and head growth. Neonatology 107, 68–75 (2015).
Tan, M., Abernethy, L. & Cooke, R. Improving head growth in preterm infants—a randomised controlled trial II: MRI and developmental outcomes in the first year. Arch. Dis. Child Fetal Neonatal Ed. 93, F342–F346 (2008).
Kidokoro, H., Neil, J. J. & Inder, T. E. New MR imaging assessment tool to define brain abnormalities in very preterm infants at term. Am. J. Neuroradiol. 34, 2208–2214 (2013).
Author information
Authors and Affiliations
Contributions
Each author made a substantial contribution to this systematic review and met the Pediatric Research authorship requirements. K.M.O. contributed to systematic review conception and design, study screening, data acquisition and interpretation, and article drafting and revisions. S.K. aided in systematic review conception and design, study screening, and article drafting and revisions. N.A. participated in study conception and design, data interpretation, and article drafting and revisions. C.L. contributed to study conception and design, data interpretation, and revising it critically for important intellectual content. All authors have approved the final submitted version.
Corresponding author
Ethics declarations
Competing interests
The contents of this article are solely the responsibility of the authors and do not reflect the official policy or position of the US Air Force, Department of Defense, or the US Government. The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ottolini, K.M., Andescavage, N., Keller, S. et al. Nutrition and the developing brain: the road to optimizing early neurodevelopment: a systematic review. Pediatr Res 87, 194–201 (2020). https://doi.org/10.1038/s41390-019-0508-3
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-019-0508-3
This article is cited by
-
Medium-chain triglycerides tricaprin TC10 and tricaprylin TC8 attenuated HFD-induced cognitive decline in a manner dependent on or independent of GLP-1
Scientific Reports (2025)
-
Donor human milk and structural brain development in very preterm infants
Pediatric Research (2025)
-
Effect of breast milk intake volume on early behavioral neurodevelopment of extremely preterm infants
International Breastfeeding Journal (2024)
-
Probiotic supplementation and risk of necrotizing enterocolitis and mortality among extremely preterm infants—the Probiotics in Extreme Prematurity in Scandinavia (PEPS) trial: study protocol for a multicenter, double-blinded, placebo-controlled, and registry-based randomized controlled trial
Trials (2024)
-
Dolphin CONTINUE: a multi-center randomized controlled trial to assess the effect of a nutritional intervention on brain development and long-term outcome in infants born before 30 weeks of gestation
BMC Pediatrics (2024)