Abstract
Background
Intellectual disability (ID) is a prevalent chronic disability affecting up to 1–3% of the general population. Small head circumference at birth, a surrogate measure of foetal cerebral growth, may be a risk factor for ID. We aimed to investigate the association between the full distribution of head circumference at birth and ID.
Methods
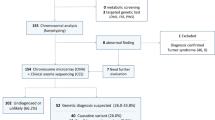
This cohort study was based on Danish nationwide registries and included all Danish singletons born alive from 1997 to 2013. Follow-up ended at October 2015. The data was analysed using a Cox proportional hazards regression model adjusted for a large number of potential confounders.
Results
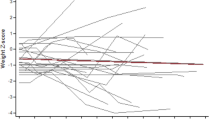
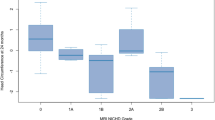
The cohort comprised 986,909 infants. Neither microcephaly nor macrocephaly at birth was consistently associated with the risk of ID. Within the normal range of head circumference, larger head circumference was associated with a decreased risk of ID (HR per standard deviation increase in head circumference z score 0.85, 95% CI 0.81–0.88). The association detected within the normal range was consistent in all sensitivity analyses.
Conclusions
Intrauterine brain growth restriction may be a risk factor for ID.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Maulik, P. K., Mascarenhas, M. N., Mathers, C. D., Dua, T. & Saxena, S. Prevalence of intellectual disability: a meta-analysis of population-based studies. Res Dev. Disabil. 32, 419–436 (2011).
Katz, G. & Lazcano-Ponce, E. Intellectual disability: definition, etiological factors, classification, diagnosis, treatment and prognosis. Salud Publica Mex. 50, s132–s141 (2008).
Shea, S. E. Intellectual disability (mental retardation). Pediatr. Rev. 33, 110–121 (2012). Quiz 120–121.
Huang, J., Zhu, T., Qu, Y. & Mu, D. Prenatal, perinatal and neonatal risk factors for intellectual disability: a systemic review and meta-analysis. PLoS ONE 11, e0153655 (2016).
Dolk, H. The predictive value of microcephaly during the first year of life for mental retardation at seven years. Dev. Med. Child Neurol. 33, 974–983 (1991).
Cooke, R. W., Lucas, A., Yudkin, P. L. & Pryse-Davies, J. Head circumference as an index of brain weight in the fetus and newborn. Early Hum. Dev. 1, 145–149 (1977).
Cheong, J. L. et al. Head growth in preterm infants: correlation with magnetic resonance imaging and neurodevelopmental outcome. Pediatrics 121, e1534–e1540 (2008).
Munakata, S. et al. Gray matter volumetric MRI differences late-preterm and term infants. Brain Dev. 35, 10–16 (2013).
Bliddal, M., Broe, A., Pottegard, A., Olsen, J. & Langhoff-Roos, J. The Danish Medical Birth Register. Eur. J. Epidemiol. 33, 27–36 (2018).
Harris, S. R. Measuring head circumference: update on infant microcephaly. Can. Fam. Physician 61, 680–684 (2015).
Lundgren, E. M., Cnattingius, S., Jonsson, B. & Tuvemo, T. Intellectual and psychological performance in males born small for gestational age with and without catch-up growth. Pediatr. Res. 50, 91–96 (2001).
Flensborg-Madsen, T. & Mortensen, E. L. Birth weight and intelligence in young adulthood and midlife. Pediatrics 139, e20163161 (2017).
Eide, M. G., Oyen, N., Skjaerven, R. & Bjerkedal, T. Associations of birth size, gestational age, and adult size with intellectual performance: evidence from a cohort of Norwegian men. Pediatr. Res. 62, 636–642 (2007).
Bergvall, N., Iliadou, A., Tuvemo, T. & Cnattingius, S. Birth characteristics and risk of low intellectual performance in early adulthood: are the associations confounded by socioeconomic factors in adolescence or familial effects? Pediatrics 117, 714–721 (2006).
Langridge, A. T. et al. Maternal conditions and perinatal characteristics associated with autism spectrum disorder and intellectual disability. PLoS ONE 8, e50963 (2013).
Leonard, H. et al. Relation between intrauterine growth and subsequent intellectual disability in a ten-year population cohort of children in Western Australia. Am. J. Epidemiol. 167, 103–111 (2008).
Bilder, D. A. et al. Prenatal and perinatal factors associated with intellectual disability. Am. J. Intellect. Dev. Disabil. 118, 156–176 (2013).
Aagaard, K., Bach, C. C., Henriksen, T. B., Larsen, R. T. & Matthiesen, N. B. Head circumference at birth and childhood developmental disorders in a nationwide cohort in Denmark. Paediatr. Perinat. Epidemiol. 32, 458–466 (2018).
Schmidt, M., Pedersen, L. & Sorensen, H. T. The Danish Civil Registration System as a tool in epidemiology. Eur. J. Epidemiol. 29, 541–549 (2014).
Jorgensen, F. S. Ultrasonography of pregnant women in Denmark 1999-2000. Description of the development since 1980-1990. Ugeskr. Laege. 165, 4409–4415 (2003).
Matthiesen, N. B. et al. Congenital heart defects and indices of placental and fetal growth in a nationwide study of 924 422 liveborn infants. Circulation 134, 1546–1556 (2016).
Talge, N. M., Mudd, L. M., Sikorskii, A. & Basso, O. United States birth weight reference corrected for implausible gestational age estimates. Pediatrics 133, 844–853 (2014).
Munk-Jorgensen, P. & Mortensen, P. B. The Danish Psychiatric Central Register. Dan. Med. Bull. 44, 82–84 (1997).
Lynge, E., Sandegaard, J. L. & Rebolj, M. The Danish National Patient Register. Scand. J. Public Health 39, 30–33 (2011).
Kildemoes, H. W., Sorensen, H. T. & Hallas, J. The Danish National Prescription Registry. Scand. J. Public Health 39, 38–41 (2011).
Olesen, J. B. et al. Validation of risk stratification schemes for predicting stroke and thromboembolism in patients with atrial fibrillation: nationwide cohort study. BMJ 342, d124 (2011).
Molgaard-Nielsen, D., Pasternak, B. & Hviid, A. Oral fluconazole during pregnancy and risk of birth defects. N. Engl. J. Med. 369, 2061–2062 (2013).
Olsen, M., Sorensen, H. T., Hjortdal, V. E., Christensen, T. D. & Pedersen, L. Congenital heart defects and developmental and other psychiatric disorders: a Danish nationwide cohort study. Circulation 124, 1706–1712 (2011).
Thygesen, L. C., Daasnes, C., Thaulow, I. & Bronnum-Hansen, H. Introduction to Danish (nationwide) registers on health and social issues: structure, access, legislation, and archiving. Scand. J. Public Health 39, 12–16 (2011).
Greenland, S., Pearl, J. & Robins, J. M. Causal diagrams for epidemiologic research. Epidemiology 10, 37–48 (1999).
Susser, E., Eide, M. G. & Begg, M. Invited commentary: the use of sibship studies to detect familial confounding. Am. J. Epidemiol. 172, 537–539 (2010).
Obel, C., et al. The risk of attention deficit hyperactivity disorder in children exposed to maternal smoking during pregnancy - a reexamination using a sibling design. J. Child Psychol. Psychiatry 57, 532–537 (2015).
Sterne, J. A. et al. Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ 338, b2393 (2009).
Committee to Evaluate the Supplemental Security Income Disability Program for Children with Mental Disorders et al. (eds Boat, T. F. & Wu, J. T.) Mental Disorders and Disabilities Among Low-Income Children (National Academies Press, Washington, DC, 2015).
Schieve, L. A., Clayton, H. B., Durkin, M. S., Wingate, M. S. & Drews-Botsch, C. Comparison of perinatal risk factors associated with autism spectrum disorder (ASD), intellectual disability (ID), and co-occurring ASD and ID. J. Autism Dev. Disord. 45, 2361–2372 (2015).
Neece, C. L., Baker, B. L. & Lee, S. S. ADHD among adolescents with intellectual disabilities: pre-pathway influences. Res. Dev. Disabil. 34, 2268–2279 (2013).
Jepsen, J. R., Fagerlund, B. & Mortensen, E. L. Do attention deficits influence IQ assessment in children and adolescents with ADHD? J. Atten. Disord. 12, 551–562 (2009).
Bolte, S., Dziobek, I. & Poustka, F. Brief report: The level and nature of autistic intelligence revisited. J. Autism Dev. Disord. 39, 678–682 (2009).
Gilmore, E. C. & Walsh, C. A. Genetic causes of microcephaly and lessons for neuronal development. Wiley Interdiscip. Rev. Dev. Biol. 2, 461–478 (2013).
West, J., Manchester, B., Wright, J., Lawlor, D. A. & Waiblinger, D. Reliability of routine clinical measurements of neonatal circumferences and research measurements of neonatal skinfold thicknesses: findings from the Born in Bradford study. Paediatr. Perinat. Epidemiol. 25, 164–171 (2011).
Acknowledgements
The Perinatal Epidemiology Research Unit, Aarhus University Hospital, Denmark provided financial support covering salaries and purchase of data.
Author information
Authors and Affiliations
Contributions
All authors met the Pediatric Research authorship requirements. N.B.M. was responsible for acquisition of data. T.B.H., N.B.M., and C.C.B. were mainly responsible for the conception and design of the study. K.A. and R.T.L. were mainly responsible for data analysis. All authors contributed to the interpretation of the data. K.A. was responsible for the initial draft of the article. Finally, all authors critically revised the article for important intellectual content and approved the final version prior to submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Aagaard, K., Matthiesen, N.B., Bach, C.C. et al. Head circumference at birth and intellectual disability: a nationwide cohort study. Pediatr Res 87, 595–601 (2020). https://doi.org/10.1038/s41390-019-0593-3
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-019-0593-3
This article is cited by
-
Effectiveness of the support program of providing food baskets for needy undernourished pregnant and lactating mothers in Iran: a case study of population level intervention
BMC Pregnancy and Childbirth (2025)
-
Altered head size at birth is associated with maternal 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD) exposure in Vietnamese infants
Scientific Reports (2025)
-
Decreased head circumference at birth associated with maternal tobacco smoke exposure during pregnancy on the Japanese prospective birth cohort study
Scientific Reports (2021)