Abstract
Background
Subclinical cardiovascular risks of secondhand smoke (SHS) exposure among children and adolescents remains insufficiently described.
Methods
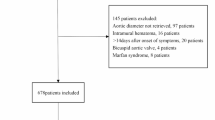
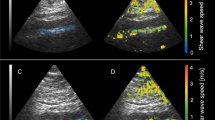
This was a cross-sectional study of 298 children and adolescents (48.0% male, body mass index: 27.0 ± 8.9 kg/m2), including 49 self-reported cases with SHS. Arterial elasticity and stiffness (distensibility, compliance, incremental elastic modulus [IEM]) were obtained via ultrasound imaging in the abdominal aorta, brachial, and carotid arteries. A one-way analysis of variance compared differences between groups, and multiple linear regression adjusted for covariates.
Results
SHS was associated with lower abdominal aorta diameter distensibility (aDD) (13.4 ± 3.6% vs. 16.0 ± 5.2%, p = 0.009) and abdominal aorta cross-sectional distensibility (aCSD) (28.8 ± 8.3% vs. 35.1 ± 12.2%, p = 0.009), as well as higher abdominal aorta IEM (aIEM) (1241 ± 794 vs. 935 ± 388 mmHg, p = 0.001). After adjustment for covariates, aDD (p = 0.047), aCSD (p = 0.040), and aIEM (p = 0.017) remained significant; this significance persisted with the additional adjustment of percent body fat. Measures of brachial and carotid compliance and distensibility were not associated with SHS.
Conclusions
SHS was associated with abdominal aorta stiffness; the majority of vascular measures within the brachial and carotid artery remained unaffected following adjustment for covariates, including hypertension and adiposity. SHS may predispose individuals to increased abdominal aorta stiffness, an artery previously reported to exhibit increased susceptibility to atherosclerosis.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Barnoya, J. & Glantz, S. A. Cardiovascular effects of secondhand smoke: nearly as large as smoking. Circulation 111, 2684–2698 (2005).
Davis, J. W., Shelton, L., Watanabe, I. S. & Arnold, J. Passive smoking affects endothelium and platelets. Arch. Intern. Med. 149, 386–389 (1989).
Otsuka, R. et al. Acute effects of passive smoking on the coronary circulation in healthy young adults. JAMA 286, 436–441 (2001).
Celermajer, D. S. et al. Passive smoking and impaired endothelium-dependent arterial dilatation in healthy young adults. N. Engl. J. Med. 334, 150–154 (1996).
Sumida, H. et al. Does passive smoking impair endothelium-dependent coronary artery dilation in women? J. Am. Coll. Cardiol. 31, 811–815 (1998).
Mack, W. J., Islam, T., Lee, Z., Selzer, R. H. & Hodis, H. N. Environmental tobacco smoke and carotid arterial stiffness. Prev. Med. 37, 148–154 (2003).
Mahmud, A. & Feely, J. Effects of passive smoking on blood pressure and aortic pressure waveform in healthy young adults—influence of gender. Br. J. Clin. Pharm. 57, 37–43 (2004).
Stefanadis, C. et al. Unfavorable effects of passive smoking on aortic function in men. Ann. Intern. Med. 128, 426–434 (1998).
Panagiotakos, D. B. et al. Effect of exposure to secondhand smoke on markers of inflammation: the ATTICA study. Am. J. Med. 116, 145–150 (2004).
Moritsugu, K. P. The 2006 Report of the Surgeon General: the health consequences of involuntary exposure to tobacco smoke. Am. J. Prev. Med. 32, 542–543 (2007).
Tsai, J. et al. Exposure to secondhand smoke among nonsmokers—United States, 1988–2014. Morb. Mortal. Wkly Rep. 67, 1342–1346 (2018).
Raghuveer, G. et al. Cardiovascular consequences of childhood secondhand tobacco smoke exposure: prevailing evidence, burden, and racial and socioeconomic disparities: a scientific statement from the american heart association. Circulation 134, e336–e359 (2016).
Bandiera, F. C., Richardson, A. K., Lee, D. J., He, J. P. & Merikangas, K. R. Secondhand smoke exposure and mental health among children and adolescents. Arch. Pediatr. Adolesc. Med. 165, 332–338 (2011).
Chen, R., Clifford, A., Lang, L. & Anstey, K. J. Is exposure to secondhand smoke associated with cognitive parameters of children and adolescents?–a systematic literature review. Ann. Epidemiol. 23, 652–661 (2013).
Kabir, Z., Connolly, G. N. & Alpert, H. R. Secondhand smoke exposure and neurobehavioral disorders among children in the United States. Pediatrics 128, 263–270 (2011).
Weitzman, M. et al. Tobacco smoke exposure is associated with the metabolic syndrome in adolescents. Circulation 112, 862–869 (2005).
Mannino, D. M., Moorman, J. E., Kingsley, B., Rose, D. & Repace, J. Health effects related to environmental tobacco smoke exposure in children in the United States: data from the Third National Health and Nutrition Examination Survey. Arch. Pediatr. Adolesc. Med. 155, 36–41 (2001).
West, H. W. et al. Exposure to parental smoking in childhood is associated with increased risk of carotid atherosclerotic plaque in adulthood: the Cardiovascular Risk in Young Finns Study. Circulation 131, 1239–1246 (2015).
Kallio, K. et al. Arterial intima-media thickness, endothelial function, and apolipoproteins in adolescents frequently exposed to tobacco smoke. Circ. Cardiovasc. Qual. Outcomes 3, 196–203 (2010).
Simonetti, G. D. et al. Determinants of blood pressure in preschool children: the role of parental smoking. Circulation 123, 292–298 (2011).
Flynn, J. T. et al. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics 140, 1–72 (2017).
Atkinson, G. & Batterham, A. M. Allometric scaling of diameter change in the original flow-mediated dilation protocol. Atherosclerosis 226, 425–427 (2013).
Lanne, T., Hansen, F., Mangell, P. & Sonesson, B. Differences in mechanical properties of the common carotid artery and abdominal aorta in healthy males. J. Vasc. Surg. 20, 218–225 (1994).
Glantz, S. A. & Parmley, W. W. Passive smoking and heart disease. Mechanisms risk. JAMA 273, 1047–1053 (1995).
Glantz, S. A. & Parmley, W. W. Passive smoking and heart disease. Epidemiol. Physiol. Biochem. Circ. 83, 1–12 (1991).
Rubenstein, D., Jesty, J. & Bluestein, D. Differences between mainstream and sidestream cigarette smoke extracts and nicotine in the activation of platelets under static and flow conditions. Circulation 109, 78–83 (2004).
Argacha, J. F. et al. Acute effects of passive smoking on peripheral vascular function. Hypertension 51, 1506–1511 (2008).
Gac, P., Poreba, M., Mazur, G. & Poreba, R. The aortic mechanical properties in patients with the essential hypertension environmentally exposed to cigaret smoke. Inhal. Toxicol. 27, 717–723 (2015).
Chen, W. et al. Secondhand smoke exposure is associated with increased carotid artery intima-media thickness: the Bogalusa Heart Study. Atherosclerosis 240, 374–379 (2015).
Peinemann, F. et al. Secondhand smoke exposure and coronary artery calcification among nonsmoking participants of a population-based cohort. Environ. Health Perspect. 119, 1556–1561 (2011).
Yankelevitz, D. F. et al. Second-hand tobacco smoke in never smokers is a significant risk factor for coronary artery calcification. JACC Cardiovasc. Imag. 6, 651–657 (2013).
Juonala, M. et al. Parental smoking in childhood and brachial artery flow-mediated dilatation in young adults: the Cardiovascular Risk in Young Finns study and the Childhood Determinants of Adult Health study. Arterioscler. Thromb. Vasc. Biol. 32, 1024–1031 (2012).
Wang, L., Mamudu, H. M., Alamian, A., Anderson, J. L. & Brooks, B. Independent and joint effects of prenatal maternal smoking and maternal exposure to second-hand smoke on the development of adolescent obesity: a longitudinal study. J. Paediatr. Child Health 50, 908–915 (2014).
Wahabi, H. A., Mandil, A. A., Alzeidan, R. A., Bahnassy, A. A. & Fayed, A. A. The independent effects of second hand smoke exposure and maternal body mass index on the anthropometric measurements of the newborn. BMC Public Health 13, 1058 (2013).
Wahabi, H. A. et al. Effects of secondhand smoke on the birth weight of term infants and the demographic profile of Saudi exposed women. BMC Public Health 13, 341 (2013).
Salmasi, G., Grady, R., Jones, J. & McDonald, S. D. Environmental tobacco smoke exposure and perinatal outcomes: a systematic review and meta-analyses. Acta Obstet. Gynecol. Scand. 89, 423–441 (2010).
Kawasaki, T., Sasayama, S., Yagi, S., Asakawa, T. & Hirai, T. Non-invasive assessment of the age related changes in stiffness of major branches of the human arteries. Cardiovasc. Res. 21, 678–687 (1987).
Homa, D. M. et al. Vital signs: disparities in nonsmokers’ exposure to secondhand smoke—United States, 1999–2012. Morb. Mortal. Wkly Rep. 64, 103–108 (2015).
Acknowledgements
Funding for this project was provided by the National Heart, Lung, and Blood Institute (R01HL110957, awarded to A.S.K.).
Author information
Authors and Affiliations
Contributions
No payment was received to produce this manuscript. M.M.H. drafted the manuscript. M.M.H. and J.R.R. developed the aims and hypothesis. A.S.K. and J.R.R. provided the funding, and contributed to the conception, design, and analysis and interpretation of the data. N.G.E. was involved with the acquisition of the data. K.D.R., A.S.K., D.R.D., N.G.E., and J.R.R. provided subject matter expertise and a critical review of the manuscript. All authors have seen this manuscript, and give approval of this version to be published.
Corresponding author
Ethics declarations
Competing interests
Dr. Kelly serves as a consultant for Novo Nordisk, WW, and Vivus Pharmaceuticals, but does not receive personal or professional income for these activities; he also receives research support (drug/placebo) from Astra Zeneca Pharmaceuticals for an NIDDK-funded clinical trial. Dr. Dengel serves as a paid consultant for Hologic Inc. Dr. Ryder receives research support (drug/placebo) from Boheringer Ingelheim for a clinical trial. The other authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Harbin, M.M., Kelly, A.S., Dengel, D.R. et al. Relation of secondhand smoke exposure to vascular phenotypes in children and adolescents. Pediatr Res 87, 760–766 (2020). https://doi.org/10.1038/s41390-019-0627-x
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-019-0627-x