Abstract
Background
Intestinal recovery after NEC is difficult to predict in individuals. We evaluated whether several biomarkers predict intestinal recovery after NEC in preterm infants.
Methods
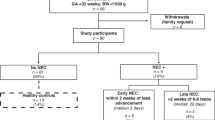
We measured intestinal tissue oxygen saturation (rintSO2) and collected urinary intestinal-fatty acid binding protein (I-FABPu) levels 0–24 h and 24–48 h after NEC onset, and before and after the first re-feed. We assessed intestinal recovery in two ways: time to full enteral feeding (FEFt; below or equal/above group’s median) and development of post-NEC complications (recurrent NEC/post-NEC stricture). We determined whether the rintSO2, its range, and I-FABPu differed between groups.
Results
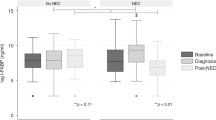
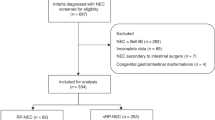
We included 27 preterm infants who survived NEC (Bell’s stage ≥ 2). Median FEFt was 14 [IQR: 12–23] days. Biomarkers only predicted intestinal recovery after the first re-feed. Mean rintSO2 ≥ 53% combined with mean rintSO2range ≥ 50% predicted FEFt < 14 days with OR 16.7 (CI: 2.3–122.2). The rintSO2range was smaller (33% vs. 51%, p < 0.01) and I-FABPu was higher (92.4 vs. 25.5 ng/mL, p = 0.03) in case of post-NEC stricture, but not different in case of recurrent NEC, compared with infants without complications.
Conclusion
The rintSO2, its range, and I-FABPu after the first re-feed after NEC predicted intestinal recovery. These biomarkers have potential value in individualizing feeding regimens after NEC.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Mϋller, M. J., Paul, T. & Seeliger, S. Necrotizing enterocolitis in premature infants and newborns. J. Neonatal Perinat. Med. 9, 233–242 (2016).
Lin, P. W. & Stoll, B. J. Necrotising enterocolitis. Lancet 368, 1271–1283 (2006).
Bohnhorst, B. et al. Early feeding after necrotizing enterocolitis in preterm infants. J. Pediatr. 143, 484–487 (2003).
Valpacos, M. et al. Diagnosis and management of necrotizing enterocolitis: an international survey of neonatologists and pediatric surgeons. Neonatology 113, 170–176 (2018).
Hock, A. M. et al. Initiation of enteral feeding after necrotizing enterocolitis. Eur. J. Pediatr. Surg. 28, 44–50 (2018).
Zani, A. et al. EUPSA Network. International survey on the management of necrotizing enterocolitis. Eur. J. Pediatr. Surg. 25, 27–33 (2015).
Patel, P. & Bhatia, J. Total parenteral nutrition for the very low birth weight infant. Semin. Fetal Neonatal Med. 22, 2–7 (2017).
Thureen, P. J. & Hay, W. W. Jr. Early aggressive nutrition in preterm infants. Semin. Neonatol. 6, 403–415 (2001).
Corvaglia, L. et al. Bolus vs. continuous feeding: Effects on splanchnic and cerebral tissue oxygenation in healthy preterm infants. Pediatr. Res. 76, 81–85 (2014).
Ehrenkranz, R. A. et al. Growth in the neonatal intensive care unit influences neurodevelopmental and growth outcomes of extremely low birth weight infants. Pediatrics 117, 1253–1261. (2006).
Franz, A. R. et al. Intrauterine, early neonatal, and postdischarge growth and neurodevelopmental outcome at 5.4 years in extremely preterm infants after intensive neonatal nutritional support. Pediatrics 123, e101–e109 (2009).
Stringer, M. D. et al. Recurrent necrotizing enterocolitis. J. Pediatr. Surg. 28, 979–981 (1993).
Thyoka, M. et al. Advanced necrotizing enterocolitis Part 2: Recurrence of necrotizing enterocolitis. Eur. J. Pediatr. Surg. 22, 13–16 (2012).
Schat, T. E. et al. Early cerebral and intestinal oxygenation in the risk assessment of necrotizing enterocolitis in preterm infants. Early Hum. Dev. 131, 75–80 (2019).
Patel, A. K. et al. Abdominal near-infrared spectroscopy measurements are lower in preterm infants at risk for necrotizing enterocolitis. Pediatr. Crit. Care Med. 15, 735–741 (2014).
Fortune, P. M., Wagstaff, M. & Petros, A. J. Cerebro-splanchnic oxygenation ratio (CSOR) using near infrared spectroscopy may be able to predict splanchnic ischaemia in neonates. Intensive Care Med. 27, 1401–1407 (2001).
Chen, Y. et al. The role of ischemia in necrotizing enterocolitis. J. Pediatr. Surg. 51, 1255–1261 (2016).
Schat, T. E. et al. Near-infrared spectroscopy to predict the course of necrotizing enterocolitis. PLoS ONE 11, e0154710 (2016).
Schat, T. E. et al. The relation between splanchnic ischaemia and intestinal damage in necrotising enterocolitis. Arch. Dis. Child Fetal Neonatal Ed. 101, F533–F539 (2016).
Thuijls, G. et al. Non-invasive markers for early diagnosis and determination of the severity of necrotizing enterocolitis. Ann. Surg. 251, 1174–1180 (2010).
Frost, B. L., Modi, B. P., Jaksic, T. & Caplan, M. S. New medical and surgical insights into neonatal necrotizing enterocolitis: a review. JAMA Pediatr. 171, 83–88 (2017).
Schurink, M. et al. Intestinal fatty acid-binding protein as a diagnostic marker for complicated and uncomplicated necrotizing enterocolitis: a prospective cohort study. PLoS ONE 10, e0121336 (2015).
Heida, F. H. et al. Intestinal fatty acid-binding protein levels in Necrotizing Enterocolitis correlate with extent of necrotic bowel: results from a multicenter study. J. Pediatr. Surg. 50, 1115–1118 (2015).
Marin, T. & Moore, J. Understanding near-infrared spectroscopy. Adv. Neonatal Care 11, 382–388 (2011).
Cortez, J. et al. Noninvasive evaluation of splanchnic tissue oxygenation using near-infrared spectroscopy in preterm neonates. J. Matern. Fetal Neonatal Med. 24, 574–582 (2011).
McNeill, S., Gatenby, J. C., McElroy, S. & Engelhardt, B. Normal cerebral, renal and abdominal regional oxygen saturations using near-infrared spectroscopy in preterm infants. J. Perinatol. 31, 51–57 (2011).
Schurink, M. et al. Intestinal fatty acid-binding protein in neonates with imminent necrotizing enterocolitis. Neonatology 106, 49–54 (2014).
Walsh, M. C. & Kliegman, R. M. Necrotizing enterocolitis: treatment based on staging criteria. Pediatr. Clin. North Am. 33, 179–201 (1986).
Kalteren, W. S. et al. Red blood cell transfusions affect intestinal and cerebral oxygenation differently in preterm infants with and without subsequent necrotizing enterocolitis. Am. J. Perinatol. 35, 1031–1037 (2018).
Corvaglia, L. et al. Splanchnic oxygenation at first enteral feeding in preterm infants: correlation with feeding intolerance. J. Pediatr. Gastroenterol. Nutr. 64, 550–554 (2017).
Bora, R., Mukhopadhyay, K., Saxena, A. K., Jain, V. & Narang, A. Prediction of feed intolerance and necrotizing enterocolitis in neonates with absent end diastolic flow in umbilical artery and the correlation of feed intolerance with postnatal superior mesenteric artery flow. J. Matern. Fetal Neonatal Med. 22, 1092–1096 (2009).
Murdoch, E. M., Sinha, A. K., Shanmugalingam, S. T., Smith, G. C. & Kempley, S. T. Doppler flow velocimetry in the superior mesenteric artery on the first day of life in preterm infants and the risk of neonatal necrotizing enterocolitis. Pediatrics 118, 1999–2003 (2006).
Oste, M. et al. Formula induces intestinal apoptosis in preterm pigs within a few hours of feeding. JPEN J. Parenter. Enter. Nutr. 34, 271–279 (2010).
Reisinger, K. W. et al. Noninvasive measurement of intestinal epithelial damage at time of refeeding can predict clinical outcome after necrotizing enterocolitis. Pediatr. Res. 73, 209–213 (2013).
Gillam-Krakauer, M. et al. Correlation of abdominal rSO2 with superior mesenteric artery velocities in preterm infants. J. Perinatol. 33, 609–612 (2013).
Bozzetti, V. et al. Evaluation of splanchnic oximetry, doppler flow velocimetry in the superior mesenteric artery and feeding tolerance in very low birth weight IUGR and non-IUGR infants receiving bolus versus continuous enteral nutrition. BMC Pediatr. 12, 106 (2012).
Acknowledgements
We would like to acknowledge the nurses, medical staff of the NICU of Beatrix Children’s Hospital in Groningen, and the medical students, for helping with data collection and for creating the opportunity to carry out this study. This study was part of the research program of the postgraduate school for Behavioural and Cognitive Neurosciences, University of Groningen. S.J.K., W.S.K., and M.J.M. were financially supported by a grant from the Junior Scientific Master Class of the University of Groningen, Groningen, the Netherlands.
Author information
Authors and Affiliations
Contributions
S.J.K., E.M.W.K., J.B.F.H., and A.F.B. conceptualized and designed the study. S.J.K., W.S.K., and M.J.M. collected the data. S.J.K. analyzed the data and drafted the initial manuscript. E.M.W.K. supervised the study. W.S.K., M.J.M., A.F.B., J.B.F.H., and E.M.W.K. reviewed and revised the manuscript critically. All authors approved the final manuscript as submitted.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kuik, S.J., Kalteren, W.S., Mebius, M.J. et al. Predicting intestinal recovery after necrotizing enterocolitis in preterm infants. Pediatr Res 87, 903–909 (2020). https://doi.org/10.1038/s41390-019-0634-y
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-019-0634-y
This article is cited by
-
Nutritional management after necrotizing enterocolitis and focal intestinal perforation in preterm infants
Pediatric Research (2024)
-
Longitudinal analysis of urinary I-FABP in extremely preterm infants that develop necrotizing enterocolitis
Pediatric Research (2024)
-
Necrotizing enterocolitis: current understanding of the prevention and management
Pediatric Surgery International (2024)
-
Predicting risk factors for postoperative intestinal stenosis in neonates with necrotizing enterocolitis: development and assessment of a predictive nomogram
Pediatric Surgery International (2024)
-
The short-term effects of RBC transfusions on intestinal injury in preterm infants
Pediatric Research (2023)