Abstract
Background
Early life stress has enduring effects on physical and mental health. Hair cortisol concentrations (HCCs) reflect exposures to contextual stressors in early life, but are understudied in preschool children.
Methods
Hair samples from children (N = 693) during clinic visits (CVs) scheduled at 1–4 years (CV1–CV4) were measured using validated assay methods for HCC.
Results
HCCs were highest at CV1 and decreased at CV2–CV4, with no sex differences. Black children had higher HCC than White/other children; these differences persisted even after adjusting for socioeconomic factors. Bivariable analyses showed significant effects on HCC for Black race, with specific demographic and psychosocial factors at different ages. Multivariable analyses showed that higher HCC at CV1 were associated with Black race and male sex; at CV2 with Black race, lower maternal self-esteem, socioeconomic adversity, and the child’s risk for developmental delay; at CV3 with Black race; at CV4 with maternal depression and the child’s prior HCC values.
Conclusions
HCCs were higher in Black children than White/other races; differences were related to maternal factors, socioeconomic adversity, and the child’s risk for developmental delay. Public health measures to reduce disparities between Blacks and other races must also consider the long-term effects of chronic stress in early life.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Kalmakis, K. A. et al. Adverse childhood experiences and chronic hypothalamic-pituitary-adrenal activity. Stress 18, 446–450 (2015).
Levine, A. et al. Measuring cortisol in human psychobiological studies. Physiol. Behav. 90, 43–53 (2007).
Vanaelst, B. et al. Epidemiological approaches to measure childhood stress. Paediatr. Perinat. Epidemiol. 26, 280–297 (2012).
Xie, Q. et al. Correlation of cortisol in 1-cm hair segment with salivary cortisol in human: hair cortisol as an endogenous biomarker. Clin. Chem. Lab Med. 49, 2013–2019 (2011).
Gray, N. A. et al. Determinants of hair cortisol concentration in children: a systematic review. Psychoneuroendocrinology 87, 204–214 (2018).
Groeneveld, M. G. et al. Children’s hair cortisol as a biomarker of stress at school entry. Stress 16, 711–715 (2013).
Vanaelst, B. et al. Intercorrelations between serum, salivary, and hair cortisol and child-reported estimates of stress in elementary school girls. Psychophysiology 49, 1072–1081 (2012).
Loussouarn, G. et al. Diversity in human hair growth, diameter, colour and shape. An in vivo study on young adults from 24 different ethnic groups observed in the five continents. Eur. J. Dermatol. 26, 144–154 (2016).
Liu, C. H. & Doan, S. N. Innovations in biological assessments of chronic stress through hair and nail cortisol: conceptual, developmental, and methodological issues. Dev. Psychobiol. 61, 465–476 (2019).
Garner, A. S. & Shonkoff, J. P. Committee on Psychosocial Aspects of Child and Family Health, Committee on Early Childhood, Adoption, and Dependent Care; Section on Developmental and Behavioral Pediatrics. Early childhood adversity, toxic stress, and the role of the pediatrician: translating developmental science into lifelong health. Pediatrics 129, e224–231 (2012).
Slominski, R., Rovnaghi, C. R. & Anand, K. J. S. Methodological considerations for hair cortisol measurements in children. Ther. Drug Monit. 37, 812–820 (2015).
Palmer, F. B. et al. Early adversity, social–emotional development, and stress in urban 1-year-old children. J. Pediatr. 163, 1733–1739 e1731 (2013).
Rippe, R. C. et al. Splitting hair for cortisol? Associations of socio-economic status, ethnicity, hair color, gender and other child characteristics with hair cortisol and cortisone. Psychoneuroendocrinology 66, 56–64 (2016).
Bates, D. et al. Fitting Linear Mixed-Effects Models using lme4. J. Stat. Softw. 67, 1–48 (2015).
Anand, K. J. S. et al. Measuring socioeconomic adversity in early life. Acta Paediatr. 108, 1267–1277 (2019).
Chen, Q. & Wang, S. Variable selection for multiply-imputed data with application to dioxin exposure study. Stat. Med. 32, 3646–3659 (2013).
Hothorn, T., Hornik, K. & Zeileis, A. Unbiased recursive partitioning: a conditional inference framework. J. Comput. Graph. Stat. 15, 651–674 (2006).
Karlen, J. et al. Maternal influence on child HPA axis: a prospective study of cortisol levels in hair. Pediatrics 132, e1333–1340 (2013).
Noppe, G. et al. Validation and reference ranges of hair cortisol measurement in healthy children. Horm. Res. Paediatr. 82, 97–102 (2014).
Vaghri, Z. et al. Hair cortisol reflects socio-economic factors and hair zinc in preschoolers. Psychoneuroendocrinology 38, 331–340 (2013).
Shin, D. et al. Pre-pregnancy body mass index is associated with dietary inflammatory index and C-reactive protein concentrations during pregnancy. Nutrients 9, E351 (2017).
Shavers, V. L. & Shavers, B. S. Racism and health inequity among Americans. J. Natl. Med. Assoc. 98, 386–396 (2006).
Jawahar, M. C. et al. Epigenetic alterations following early postnatal stress: a review on novel aetiological mechanisms of common psychiatric disorders. Clin. Epigenet. 7, 122 (2015).
Lester, B. M. et al. Epigenetic programming by maternal behavior in the human infant. Pediatrics 142, e20171890 (2018).
Wosu, A. C. et al. Hair cortisol in relation to sociodemographic and lifestyle characteristics in a multiethnic US sample. Ann. Epidemiol. 25, 90–95 (2015). 95 e91-92.
O’Brien, K. M., Tronick, E. Z. & Moore, C. L. Relationship between hair cortisol and perceived chronic stress in a diverse sample. Stress Health 29, 337–344 (2013).
Schreier, H. M. et al. Lifetime exposure to traumatic and other stressful life events and hair cortisol in a multi-racial/ethnic sample of pregnant women. Stress 19, 45–52 (2016).
Schreier, H. M. et al. Childhood abuse is associated with increased hair cortisol levels among urban pregnant women. J. Epidemiol. Community Health 69, 1169–1174 (2015).
Blair, C. et al. Key Investigators Family Life Project. Allostasis and allostatic load in the context of poverty in early childhood. Dev. Psychopathol. 23, 845–857 (2011).
Bush, N. R. et al. Kindergarten stressors and cumulative adrenocortical activation: the “first straws” of allostatic load? Dev. Psychopathol. 23, 1089–1106 (2011).
Blair, C. et al. Maternal and child contributions to cortisol response to emotional arousal in young children from low-income, rural communities. Dev. Psychol. 44, 1095–1109 (2008).
Finegood, E. D. et al. for the Family Life Project. Exploring longitudinal associations between neighborhood disadvantage and cortisol levels in early childhood. Dev. Psychopathol. 29, 1649–1662 (2017).
Russell, J., Grant, C. C. &n Morton S. M. B. Multimorbidity in early childhood and socioeconomic disadvantage: findings from a large New Zealand child cohort. Acad. Pediatr. pii: S1876-2859(19)30390-0. (2019). https://doi.org/10.1016/j.acap.2019.09.007. [Epub ahead of print].
Lehrer, H. M. et al. Hair cortisol concentration and glycated hemoglobin in African American adults. Psychoneuroendocrinology 72, 212–218 (2016).
Struber, N., Struber, D. & Roth, G. Impact of early adversity on glucocorticoid regulation and later mental disorders. Neurosci. Biobehav Rev. 38, 17–37 (2014).
Gerber, M. et al. In 6- to 8-year-old children, hair cortisol is associated with body mass index and somatic complaints, but not with stress, health-related quality of life, blood pressure, retinal vessel diameters, and cardiorespiratory fitness. Psychoneuroendocrinology 76, 1–10 (2017).
Essex, M. J. et al. Exploring risk factors for the emergence of children’s mental health problems. Arch. Gen. Psychiatry 63, 1246–1256 (2006).
Marti, M. et al. The influence of hair lipids in ethnic hair properties. Int. J. Cosmet. Sci. 38, 77–84 (2016).
Salinas-Miranda, A. A. et al. Adverse childhood experiences and health-related quality of life in adulthood: revelations from a community needs assessment. Health Qual. Life Outcomes 13, 123 (2015).
Mersky, J. P., Topitzes, J. & Reynolds, A. J. Impacts of adverse childhood experiences on health, mental health, and substance use in early adulthood: a cohort study of an urban, minority sample in the U.S. Child Abus. Negl. 37, 917–925 (2013).
Noonan, A. S., Velasco-Mondragon, H. E. & Wagner, F. A. Improving the health of African Americans in the USA: an overdue opportunity for social justice. Public Health Rev. 37, 12 (2016).
Acknowledgements
Grant Somes, Ph.D. (University of Tennessee Health Science Center [UTHSC]) conceived of the CANDLE study and obtained initial funding. We gratefully acknowledge the participants, particularly the mothers who consented to participate in the CANDLE study; the cognitive examiners from the UTHSC Boling Center for Developmental Disabilities: Sacha Bliss, Ph.D., Lauren Gardner, Ph.D., Bruce Keisling, Ph.D., Cynthia Klubnik, Ph.D., Kerrie Murphy, Ph.D., Jessica Myszak, Ph.D., Nichol Pritchard, Ph.D., Colby Reed, Ph.D., Christina Warner-Metzger, Ph.D.; and other individuals from UTHSC who participated in the design and execution of the study: Phyllis Richey, Ph.D., Wonsuk Yoo, Ph.D., D. Pamela Connor, Ph.D., Marion Hare, M.D., M.S., and Anand Kulkarni, M.D.; Karmen McPherson and Aaron Kala (UTHSC medical students) for helping with hair cortisol analyses performed in the Pain/Stress Neurobiology Laboratory at the University of Tennessee Neuroscience Institute; data collection, processing and editing by the CANDLE staff; Amy Scheck, M.S., CANDLE science coordinator and Maureen Sorrells, MPH CANDLE study coordinator at UTHSC. We also acknowledge helpful comments from Drs. Nicole Bush, Ph.D. (UCSF), Kaja LeWinn, Sc.D. (UCSF) and Robert Davis, M.D., MPH (UTHSC) on earlier drafts of this manuscript. Grants from The Urban Child Institute to the University of Tennessee Department of Preventive Medicine supported the CANDLE study (Principal Investigator (P.I.) Tylavsky). The current studies received funding from the Maternal & Child Health Research Institute at Stanford University (P.I. Anand), NIH/National Institute for Drug Abuse (R41 DA046983, P.I. Anand), NIH/Eunice Kennedy Shriver National Institute for Child Health & Human Development (R01 HD099296, P.I. Anand; R21 HD090493, P.I. Gotlib); NIH/National Institute of Mental Health (R37 MH101495, P.I. Gotlib), and the Oxnard Foundation to UTHSC (P.I. Anand). Study sponsors had no role in the design and conduct of the study; the collection, management, analysis, or interpretation of the data; the preparation, review, approval, or decision to publish this manuscript. Authors received no honoraria, grants, or other payments for writing this manuscript.
Author information
Authors and Affiliations
Contributions
K.J.S.A. provided the concept and study design, obtained funding, designed data analysis and data interpretation, initially drafted the article, made critical revisions of the article, and approved the final version to be published; C.R.R. contributed to research design, sample analyses, data analysis and interpretation, critical revisions of the article, and approved the final version to be published; J.R. performed all data analyses and interpretation, drafted and critically revised the article, and approved the final version to be published; F.F.Q. and S.T. contributed to data analysis and interpretation, critical revisions of the article, and approved the final version to be published; L.E.M., D.A.B., and I.H.G. helped with data interpretation, critical revisions of the article, and approved the final version to be published; and F.A.T. contributed to conception and study design, research regulatory compliance, data collection, critical revisions of the article, and approved the final version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Anand, K.J.S., Rovnaghi, C.R., Rigdon, J. et al. Demographic and psychosocial factors associated with hair cortisol concentrations in preschool children. Pediatr Res 87, 1119–1127 (2020). https://doi.org/10.1038/s41390-019-0691-2
Received:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-019-0691-2
This article is cited by
-
Linear hair growth rates in preschool children
Pediatric Research (2024)
-
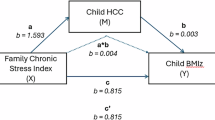
Association between maternal psychological factors and offspring executive function: analysis of African-American mother–child dyads
Pediatric Research (2022)
-
The social ecology of childhood and early life adversity
Pediatric Research (2021)