Abstract
Background
The mechanisms responsible for the associations between very preterm birth and a higher risk of poor cardiovascular and metabolic health in adult life are unknown.
Methods
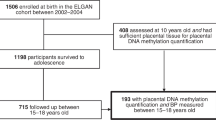
Here, we compare the clinical and molecular phenotypes of healthy, normal-weight young adults (18–27 years), born very preterm (<33 weeks gestational age (GA)) and at full-term (37–42 weeks GA). Outcomes included whole-body MRI, hepatic and muscle 1H MRS, blood pressure measurements and telomere length.
Results
We recruited 156 volunteers, 69 preterm (45 women; 24 men) and 87 born at full-term (45 women; 42 men). Preterm individuals had a significantly altered blood pressure profile, including higher systolic blood pressure (SBP mmHg: preterm men 133.4 ± 10.1, term men 23.0 ± 6.9; preterm women 124.3 ± 7.1, term women 118.4 ± 8.0, p < 0.01 for all). Furthermore, preterm men had fewer long telomeres (145–48.5 kb: preterm men 14.1 ± 0.9%, term men 17.8 ± 1.1%, p < 0.05; 48.5–8.6 kb: preterm men 28.2 ± 2.6, term men 37.0 ± 2.4%, p < 0.001) and a higher proportion of shorter telomeres (4.2–1.3 kb: preterm men 40.4 ± 3.5%, term men 29.9 ± 3.2%, p < 0.01).
Conclusion
Our data indicate that healthy young adults born very preterm manifest clinical and molecular evidence of accelerated ageing.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Saigal, S. & Doyle, L. W. An overview of mortality and sequelae of preterm birth from infancy to adulthood. Lancet 371, 261–269 (2008). 19.
Sardesai, S., Biniwale, M., Wertheimer, F., Garingo, A. & Ramanathan, R. Evolution of surfactant therapy for respiratory distress syndrome: past, present, and future. Pediatr. Res. 81, 240–248 (2017).
de Jong, F., Monuteaux, M. C., van Elburg, R. M., Gillman, M. W. & Belfort, M. B. Systematic review and meta-analysis of preterm birth and later systolic blood pressure. Hypertension 59, 226–234 (2011).
Parkinson, J. R., Hyde, M. J., Gale, C., Santhakumaran, S. & Modi, N. Preterm birth and the metabolic syndrome in adult life: a systematic review and meta-analysis. Pediatrics 131, e1240–e1263 (2013).
Crump, C., Sundquist, K., Sundquist, J. & Winkleby, M. A. Gestational age at birth and mortality in young adulthood. Jama 306, 1233–1240 (2011).
Uthaya, S. et al. Altered adiposity after extremely preterm birth. Pediatr. Res. 57, 211–215 (2005).
Thomas, E. L. et al. Aberrant adiposity and ectopic lipid deposition characterize the adult phenotype of the preterm infant. Pediatr. Res. 70, 507–512 (2011).
Despres, J. P. et al. Abdominal obesity and the metabolic syndrome: contribution to global cardiometabolic risk. Arterioscler. Thromb. Vasc. Biol. 28, 1039–1049 (2008).
Fabbrini, E. et al. Intrahepatic fat, not visceral fat, is linked with metabolic complications of obesity. Proc. Natl Acad. Sci. USA 106, 15430–15435 (2009).
Wood, N. S. et al. The EPICure study: growth and associated problems in children born at 25 weeks of gestational age or less. Arch. Dis. Child Fetal Neonatal Ed. 88, F492–F500 (2003).
Riley, K., Roth, S., Sellwood, M. & Wyatt, J. S. Survival and neurodevelopmental morbidity at 1 year of age following extremely preterm delivery over a 20-year period: a single centre cohort study. Acta Paediatr. 97, 159–165 (2008).
Matthews, D. R. et al. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28, 412–419 (1985).
Littlejohns, T. J., Sudlow, C., Allen, N. E. & Collins, R. UK Biobank: opportunities for cardiovascular research. Eur. Heart J. 40, 1158–1166 (2017).
Katz, A. et al. Quantitative insulin sensitivity check index: a simple, accurate method for assessing insulin sensitivity in humans. J. Clin. Endocrinol. Metab. 85, 2402–2410 (2000).
Odgers, C. L., Caspi, A., Bates, C. J., Sampson, R. J. & Moffitt, T. E. Systematic social observation of children’s neighborhoods using Google Street View: a reliable and cost-effective method. J. Child Psychol. Psychiatry, Allied Discip. 53, 1009–1017 (2012).
Bayrakci, U. S., Schaefer, F., Duzova, A., Yigit, S. & Bakkaloglu, A. Abnormal circadian blood pressure regulation in children born preterm. J. Pediatr. 151, 399–403 (2007).
Delaney, A., Pellizzari, M., Speiser, P. W. & Frank, G. R. Pitfalls in the measurement of the nocturnal blood pressure dip in adolescents with type 1 diabetes. Diabetes Care 32, 165–168 (2009).
Martin, C. A. & McGrath, B. P. White-coat hypertension. Clin. Exp. Pharmacol. Physiol. 41, 22–29 (2014).
Thomas, E. L. et al. Hepatic triglyceride content and its relation to body adiposity: a magnetic resonance imaging and proton magnetic resonance spectroscopy study. Gut 54, 122–127 (2005).
Harrington, T. A., Thomas, E. L., Frost, G., Modi, N. & Bell, J. D. Distribution of adipose tissue in the newborn. Pediatr. Res. 55, 437–441 (2004).
van den Boogaart, A., Howe, F. A., Rodrigues, L. M., Stubbs, M. & Griffiths, J. R. In vivo 31P MRS: absolute concentrations, signal-to-noise and prior knowledge. NMR Biomed. 8, 87–93 (1995).
Weis, J., Johansson, L., Ortiz-Nieto, F. & Ahlstrom, H. Assessment of lipids in skeletal muscle by LCModel and AMARES. J. Magn. Reson. Imaging 30, 1124–1129 (2009).
Tarry-Adkins, J. L. et al. Poor maternal nutrition followed by accelerated postnatal growth leads to telomere shortening and increased markers of cell senescence in rat islets. FASEB J. 23, 1521–1528 (2009).
Dona, A. C. et al. Precision high-throughput proton NMR spectroscopy of human urine, serum, and plasma for large-scale metabolic phenotyping. Anal. Chem. 86, 9887–9894 (2014).
Lewis, M. R. et al. Development and application of ultra-performance liquid chromatography-TOF MS for precision large scale urinary metabolic Phenotyping. Anal. Chem. 88, 9004–9013 (2016).
Vorkas, P. A. et al. Untargeted UPLC-MS profiling pipeline to expand tissue metabolome coverage: application to cardiovascular disease. Anal. Chem. 87, 4184–4193 (2015).
Dieterle, F., Ross, A., Schlotterbeck, G. & Senn, H. Probabilistic quotient normalization as robust method to account for dilution of complex biological mixtures. Application in 1H NMR metabonomics. Anal. Chem. 78, 4281–4290 (2006).
Cloarec, O. et al. Evaluation of the orthogonal projection on latent structure model limitations caused by chemical shift variability and improved visualization of biomarker changes in 1H NMR spectroscopic metabonomic studies. Anal. Chem. 77, 517–526 (2005).
Neuhauser, M. & Manly, B. F. The Fisher-Pitman permutation test when testing for differences in mean and variance. Psychol. Rep. 94, 189–194 (2004).
Mathiasen, R., Hansen, B. M., Nybo Anderson, A. M. & Greisen, G. Socio-economic achievements of individuals born very preterm at the age of 27 to 29 years: a nationwide cohort study. Dev. Med. Child Neurol. 51, 901–908 (2009).
Heidinger, B. J. et al. Telomere length in early life predicts lifespan. Proc. Natl Acad. Sci. USA 109, 1743–1748 (2012).
Moller, P. et al. Sex-related differences in length and erosion dynamics of human telomeres favor females. Aging 1, 733–739 (2009).
Despres, J. P. & Lemieux, I. Abdominal obesity and metabolic syndrome. Nature 444, 881–887 (2006).
Kuk, J. L. et al. Visceral fat is an independent predictor of all-cause mortality in men. Obesity (Silver Spring) 14, 336–341 (2006).
Balasko, M., Soos, S., Szekely, M. & Petervari, E. Leptin and aging: Review and questions with particular emphasis on its role in the central regulation of energy balance. J. Chem. Neuroanat. 61–62, 248–255 (2014).
Johansson, S. et al. Risk of high blood pressure among young men increases with the degree of immaturity at birth. Circulation 112, 3430–3436 (2005).
Kamarck, T. W. et al. Psychosocial demands and ambulatory blood pressure: a field assessment approach. Physiol. Behav. 77, 699–704 (2002).
Ritchie, L. D., Campbell, N. C. & Murchie, P. New NICE guidelines for hypertension. BMJ 343, d5644 (2011).
Kajantie, E., Osmond, C. & Eriksson, J. G. Coronary heart disease and stroke in adults born preterm—the Helsinki Birth Cohort Study. Paediatr. Perinat. Epidemiol. 29, 515–519 (2015).
Feldt, K. et al. Cardiovascular reactivity to psychological stressors in late adulthood is predicted by gestational age at birth. J. Hum. Hypertens. 21, 401–410 (2007).
Acknowledgements
We are grateful to Professor John Wyatt and Professor Neil Marlow for assistance in recruiting volunteers. This work was supported by the British Heart Foundation (PG/13/49/30307, PG/09/037/27387, FS/09/029/27902) and the MRC (MC UU12012/04).
Author information
Authors and Affiliations
Contributions
J.R.C.P. contributed to study design, data acquisition, analysis and interpretation, wrote, and revised the final manuscript and has given final approval of this version to be published. R.E. contributed to data acquisition, revised the article and has given final approval of this version to be published. J.L.T.A. contributed to data acquisition, revised the article and has given final approval of this version to be published. N.L. contributed to data analysis, revised the article and has given final approval of this version to be published. S.E.O. contributed to study design, data analysis and interpretation, revised the article and has given final approval of this version to be published. E.H. contributed to study design, data analysis and interpretation, revised the article and has given final approval of this version to be published. N.M. contributed to study design, data analysis and interpretation, and revised the final manuscript and has given final approval of this version to be published. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Parkinson, J.R.C., Emsley, R., Adkins, J.L.T. et al. Clinical and molecular evidence of accelerated ageing following very preterm birth. Pediatr Res 87, 1005–1010 (2020). https://doi.org/10.1038/s41390-019-0709-9
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-019-0709-9
This article is cited by
-
Neonatal multimorbidity and the phenotype of premature aging in preterm infants
Pediatric Research (2025)
-
From premature birth to premature kidney disease: does accelerated aging play a role?
Pediatric Nephrology (2024)
-
A feasibility randomized controlled trial of a NICU rehabilitation program for very low birth weight infants
Scientific Reports (2022)
-
Sex differences in the intergenerational inheritance of metabolic traits
Nature Metabolism (2022)
-
The future of perinatal research
European Journal of Pediatrics (2022)