Abstract
Background
Innovation is important to improve patient care, but few studies have explored the factors that initiate change in healthcare organizations.
Methods
As part of the European project EPICE on evidence-based perinatal care, we carried out semi-structured interviews (N = 44) with medical and nursing staff from 11 randomly selected neonatal intensive care units in 6 countries. The interviews focused on the most recent clinical or organizational change in the unit relevant to the care of very preterm infants. Thematic analysis was performed using verbatim transcripts of recorded interviews.
Results
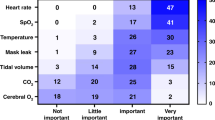
Reported changes concerned ventilation, feeding and nutrition, neonatal sepsis, infant care, pain management and care of parents. Six categories of drivers to change were identified: availability of new knowledge or technology; guidelines or regulations from outside the unit; need to standardize practices; participation in research; occurrence of adverse events; and wish to improve care. Innovations originating within the unit, linked to the availability of new technology and seen to provide clear benefit for patients were more likely to achieve consensus and rapid implementation.
Conclusions
Innovation can be initiated by several drivers that can impact on the success and sustainability of change.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
West, M. A. The social psychology of innovation in groups. In: Innovation and Creativity at Work: Psychological and Organizational Strategies (eds West, M. A. & Farr, J. L.) 309−333 (John Wiley & Sons, Oxford, UK, 1990).
Länsisalmi, H., Kivimäki, M., Aalto, P. & Ruoranen, R. Innovation in healthcare: a systematic review of recent research. Nurs. Sci. Q. 19, 66–72 (2006).
Greenhalgh, T., Robert, G., Macfarlane, F., Bate, P. & Kyriakidou, O. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q. 82, 581–629 (2004).
Prasad, V. & Ioannidis, J. P. Evidence-based de-implementation for contradicted, unproven, and aspiring healthcare practices. Implement. Sci. 9, 1 (2014).
Balas, E. A. & Chapman, W. W. Road map for diffusion of innovation in health care. Health Aff. (Millwood) 37, 198–204 (2018).
Berwick, D. M. Disseminating innovation in health care. JAMA 289, 1969–1975 (2003).
Donaldson, N. E., Rutledge, D. N. & Ashley, J. Outcomes of adoption: measuring evidence uptake by individuals and organizations. Worldviews Evid. Based Nurs. 1, S41–S51 (2004).
Lewin, K. Field Theory in Social Science (Harper & Row, New York, NY, 1951).
Kotter, J. P. Leading change. Why transformation efforts fail. Harv. Bus. Rev. 85, 92–107 (2007).
Rogers, E. M. Diffusion of Innovation 1st edn. (Free Press of Glencoe, New York, NY, 1962).
Panzano, P. C. & Roth, D. The decision to adopt evidence-based and other innovative mental health practices: risky business? Psychiatr. Serv. 57, 1153–1161 (2006).
Damschroder, L. J. et al. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement. Sci. 4, 50 (2009).
Stevens, B., Lee, S. K., Law, M. P. & Yamada, J., Canadian Neonatal Network EPIC Study Group. A qualitative examination of changing practice in Canadian neonatal intensive care units. J. Eval. Clin. Pr. 13, 287–294 (2007).
Zeitlin, J. et al. Use of evidence based practices to improve survival without severe morbidity for very preterm infants: results from the EPICE population based cohort. BMJ 354, i2976 (2016).
Pettigrew, A. M. Context and action in the transformation of the firm. J. Manag. Stud. 24, 649–670 (1987).
Guest, G. Applied Thematic Analysis (Sage Publications, Thousand Oaks, CA, 2012).
Berwick, D. M. Broadening the view of evidence-based medicine. Qual. Saf. Health Care 14, 315–316 (2005).
Baker, G. R. Strengthening the contribution of quality improvement research to evidence based health care. Qual. Saf. Health Care 15, 150–151 (2006).
Salter, K. L. & Kothari, A. Knowledge ‘translation’ as social learning: negotiating the uptake of research-based knowledge in practice. BMC Med. Educ. 16, 76 (2016).
Profetto-McGrath, J., Smith, K. B., Hugo, K., Taylor, M. & El-Hajj, H. Clinical nurse specialists' use of evidence in practice: a pilot study. Worldviews Evid. Based Nurs. 4, 86–96 (2007).
Yarcheski, A., Mahon, N. E. & Yarcheski, T. J. A descriptive study of research published in scientific nursing journals from 1985 to 2010. Int. J. Nurs. Stud. 49, 1112–1121 (2012).
Kolb, D. A. Experiential Learning Experience as a Source of Learning and Development (Prentice Hall, Englewood Cliffs, NJ, 1984).
Snijders, C. et al. Specialty-based, voluntary incident reporting in neonatal intensive care: description of 4846 incident reports. Arch. Dis. Child Fetal Neonatal Ed. 94, F210–F215 (2009).
de Feijter, J. M., de Grave, W. S., Muijtjens, A. M., Scherpbier, A. J. & Koopmans, R. P. A comprehensive overview of medical error in hospitals using incident-reporting systems, patient complaints and chart review of inpatient deaths. PLoS ONE 7, e31125 (2012).
Bradley, E. H., Schlesinger, M., Webster, T. R., Baker, D. & Inouye, S. K. Translating research into clinical practice: making change happen. J. Am. Geriatr. Soc. 52, 1875–1882 (2004).
Bloom, S. L. & Leveno, K. J. Unproven technologies in maternal-fetal medicine and the high cost of US health care. JAMA 317, 1025 (2017).
Godlee, F. Putting innovation to the test. BMJ 359, j5539 (2017).
Acknowledgements
We are grateful to all the physicians and nurses who participated in the interviews and shared their experiences with us. We thank Nikola Jeck for carrying out the interviews in Germany. The EPICE project was funded by the European Union's Seventh Framework Programme [FP7/2007−2013] (grant no. 259882). In Portugal, this study was also funded by FEDER through the Operational Programme Competitiveness and Internationalization and from the Foundation for Science and Technology—FCT (Portuguese Ministry of Science, Technology and Higher Education), under the Unidade de Investigação em Epidemiologia—Instituto de Saúde Pública da Universidade do Porto (EPIUnit) (POCI-01-0145-FEDER-006862; ref.UID/DTP/04750/2013) and the Ph.D. Grant SFRH/BD/111794/2015 (Carina Rodrigues), co-funded by the FCT and the POCH/FSE Program.
Author information
Authors and Affiliations
Contributions
M.C. designed the study, drafted the study protocol, coordinated data analyses and prepared the manuscript. E.F. coordinated data acquisition and analyses across the participating regions, carried out and transcribed the interviews in Italy and performed the overall second-stage data analyses. C.R., E.S.D., R.F.M. and M.B. participated in the finalization of the study protocol and materials, supervised data acquisition in their region and contributed to the manuscript for important aspects related to the interpretation of results and the discussion. A.F.M., A.L., J.W., A.H. carried out and transcribed the interviews in their region and performed first-stage data analyses; they contributed to the paper as regards the validity of data reporting and interpretation. I.C. prepared and maintained the quantitative database of the study, prepared the tables and figure, and performed the literature review. J.Z. initiated and coordinated the EPICE project, participated in the definition of this study aims, protocol and instrument, and substantially contributed to the manuscript for important aspects. All authors have read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cuttini, M., Forcella, E., Rodrigues, C. et al. What drives change in neonatal intensive care units? A qualitative study with physicians and nurses in six European countries. Pediatr Res 88, 257–264 (2020). https://doi.org/10.1038/s41390-019-0733-9
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41390-019-0733-9
This article is cited by
-
Multidimensional assessment of infant, parent and staff outcomes during a family centered care enhancement project in a tertiary neonatal intensive care unit: study protocol of a longitudinal cohort study
BMC Pediatrics (2023)
-
Initial surgical treatment of necrotizing enterocolitis: a meta-analysis of peritoneal drainage versus laparotomy
European Journal of Pediatrics (2022)