Abstract
Background
Infant adiposity is linked to both high maternal fat mass (FM) and excessive gestational FM gain, whereas the association with maternal adipokines is less clear. The aim was to determine how levels of maternal leptin, the soluble leptin receptor (sOB-R), adiponectin, and FM during pregnancy were linked to infant FM in normal-weight (NW) women and women with obesity (OB).
Methods
Body composition and serum levels of leptin, adiponectin, and sOB-R were determined three times during pregnancy in 80 NW and 46 OB women. For infants, body composition was measured at 1 and 12 weeks of age.
Results
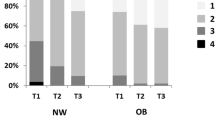
Maternal leptin and sOB-R levels increased during pregnancy. For NW women, infant FM at 1 week was inversely associated with changes in maternal leptin and at 12 weeks inversely associated with absolute maternal sOB-R levels throughout pregnancy, as well as changes in sOB-R levels in early pregnancy. For OB women, infant FM at both 1 and 12 weeks were best explained by maternal FM.
Conclusions
Leptin and sOB-R, thought to regulate leptin bioavailability, are associated with fat accumulation in infants born to NW women. In OB women, maternal FM in early pregnancy is more important than leptin in determining infant fat accumulation.
Impact
-
In normal-weight women, the regulation of maternal leptin bioavailability during pregnancy has a role in infant fat mass accumulation.
-
In women with obesity, however, pre-pregnancy maternal fat mass seems more important for infant fat mass.
-
This is the first study of maternal adipokines and fat mass including longitudinal measurements in both mothers and their children.
-
Understanding the relationship between maternal factors and infant fat mass is of great importance as obesity is programmed over the generations, and it is important to learn what regulates this programming.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Godfrey, K. M. et al. Influence of maternal obesity on the long-term health of offspring. Lancet Diabetes Endocrinol. 5, 53–64 (2017).
Patel, N., Pasupathy, D. & Poston, L. Determining the consequences of maternal obesity for offspring health. Exp. Physiol. 100, 1421–1428 (2015).
Smith, J. et al. Effects of maternal surgical weight loss in mothers on intergenerational transmission of obesity. J. Clin. Endocrinol. Metab. 94, 4275–4283 (2009).
Catalano, P. M. & Shankar, K. Obesity and pregnancy: mechanisms of short term and long term adverse consequences for mother and child. BMJ 356, j1 (2017).
Briffa, J. F., McAinch, A. J., Romano, T., Wlodek, M. E. & Hryciw, D. H. Leptin in pregnancy and development: a contributor to adulthood disease? Am. J. Physiol. Endocrinol. Metab. 308, E335–E350 (2014).
Briana, D. D. & Malamitsi‐Puchner, A. The role of adipocytokines in fetal growth. Ann. NY Acad. Sci. 1205, 82–87 (2010).
Tessier, D., Ferraro, Z. & Gruslin, A. Role of leptin in pregnancy: consequences of maternal obesity. Placenta 34, 205–211 (2013).
Andersson-Hall, U. et al. Longitudinal changes in adipokines and free leptin index during and after pregnancy in women with obesity. Int. J. Obes. 44, 675–683 (2019).
Hinkle, S. N. et al. Maternal adipokines longitudinally measured across pregnancy and their associations with neonatal size, length, and adiposity. Int. J. Obes. 43, 1422–1434 (2018).
Briana, D. D. & Malamitsi-Puchner, A. Reviews: adipocytokines in normal and complicated pregnancies. Reprod. Sci. 16, 921–937 (2009).
Howell, K. R. & Powell, T. L. Effects of maternal obesity on placental function and fetal development. Reproduction 153, R97 (2017).
Patenaude, J. et al. Associations of maternal leptin with neonatal adiposity differ according to pregravid weight. Neonatology 111, 344–352 (2017).
Valsamakis, G. et al. Neonatal birth waist is positively predicted by second trimester maternal active ghrelin, a pro-appetite hormone, and negatively associated with third trimester maternal leptin, a pro-satiety hormone. Early Hum. Dev. 90, 487–492 (2014).
Lowe, L. P. et al. Inflammatory mediators and glucose in pregnancy: results from a subset of the Hyperglycemia and Adverse Pregnancy Outcome (HAPO) Study. J. Clin. Endocrinol. Metab. 95, 5427–5434 (2010).
Josefson, J. L., Zeiss, D. M., Rademaker, A. W. & Metzger, B. E. Maternal leptin predicts adiposity of the neonate. Horm. Res. Paediatr. 81, 13–19 (2014).
Castro, N. et al. The relationship between maternal plasma leptin and adiponectin concentrations and newborn adiposity. Nutrients 9, 182 (2017).
Brunner, S. et al. Effect of reducing the n‐6/n‐3 fatty acid ratio on the maternal and fetal leptin axis in relation to infant body composition. Obesity 22, 217–224 (2014).
Svensson, H. et al. Body fat mass and the proportion of very large adipocytes in pregnant women are associated with gestational insulin resistance. Int J. Obes. 40, 646–653 (2016).
Bosaeus, M. et al. A randomized longitudinal dietary intervention study during pregnancy: effects on fish intake, phospholipids, and body composition. Nutr. J. 14, 1 (2015).
Ingelsson, E. et al. Circulating ghrelin, leptin, and soluble leptin receptor concentrations and cardiometabolic risk factors in a community-based sample. J. Clin. Endocrinol. Metab. 93, 3149–3157 (2008).
Kratzsch, J. et al. Circulating soluble leptin receptor and free leptin index during childhood, puberty, and adolescence. J. Clin. Endocrinol. Metab. 87, 4587–4594 (2002).
Niklasson, A. & Albertsson-Wikland, K. Continuous growth reference from 24th week of gestation to 24 months by gender. BMC Pediatr. 8, 8 (2008).
Bouret, S. Nutritional programming of hypothalamic development: critical periods and windows of opportunity. Int. J. Obes. Suppl. 2, S19–S24 (2012).
Yura, S. et al. Role of premature leptin surge in obesity resulting from intrauterine undernutrition. Cell Metab. 1, 371–378 (2005).
Farley, D. et al. Placental amino acid transport and placental leptin resistance in pregnancies complicated by maternal obesity. Placenta 31, 718–724 (2010).
Mohamad, M., Lim, P., Wang, Y., Soo, K. & Mohamed, H. Maternal serum and breast milk adiponectin: the association with infant adiposity development. Int. J. Environ. Res. Public Health 15, 1250 (2018).
Aye, I. L., Powell, T. L. & Jansson, T. Adiponectin—the missing link between maternal adiposity, placental transport and fetal growth? Placenta 34, S40–S45 (2013).
Harris, R. B. Direct and indirect effects of leptin on adipocyte metabolism. Biochim. Biophys. Acta 1842, 414–423 (2014).
Misra, V. K., Straughen, J. K. & Trudeau, S. Maternal serum leptin during pregnancy and infant birth weight: the influence of maternal overweight and obesity. Obesity 21, 1064–1069 (2013).
Perichart-Perera, O. et al. Metabolic markers during pregnancy and their association with maternal and newborn weight status. PLoS ONE 12, e0180874 (2017).
Jansson, N. et al. Activation of placental mTOR signaling and amino acid transporters in obese women giving birth to large babies. J. Clin. Endocrinol. Metab. 98, 105–113 (2013).
Eriksson, B., Lof, M. & Forsum, E. Body composition in full-term healthy infants measured with air displacement plethysmography at 1 and 12 weeks of age. Acta Paediatr. 99, 563–568 (2010).
Andersson-Hall, U. K. et al. Maternal obesity and gestational diabetes mellitus affect body composition through infancy: the PONCH Study. Pediatr. Res. 85, 369–377 (2018).
Young, B. E., Johnson, S. L. & Krebs, N. F. Biological determinants linking infant weight gain and child obesity: current knowledge and future directions. Adv. Nutr. 3, 675–686 (2012).
Leunissen, R. W., Kerkhof, G. F., Stijnen, T. & Hokken-Koelega, A. Timing and tempo of first-year rapid growth in relation to cardiovascular and metabolic risk profile in early adulthood. JAMA 301, 2234–2242 (2009).
Acknowledgements
We would like to thank all participating women of the PONCH study, and registered dietician Evelina Järvinen for expert care and measurements during study visits. This work was supported by grants from the Emil and Wera Cornell Foundation, the Swedish Research Council (12206), the Swedish Diabetes Association Research Foundation (2015-08), and the Swedish state under the agreement between the Swedish government and the country councils, the ALF-agreement (ALF-GBG-720851, 719041 and 812951).
Author information
Authors and Affiliations
Contributions
Conception, data acquisition, or data analysis and interpretation: U.K.A.-H., A.P., H.K.d.M., J.P.S., and A.B.H. Drafting or revising article for intellectual content: U.K.A.-H., E.C.M., K.G.A.-W., and A.B.H. Final appoval of article: U.K.A.-H., A.P., H.K.d.M., J.P.S., E.C.M., K.G.A.-W., and A.B.H.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The study was approved by the ethics committee at the University of Gothenburg (Dnr 402-08). Informed written consent was obtained from all women participating in the study. Both parents received oral and written information about the study and gave informed written consent before enrollment of their children.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Andersson-Hall, U.K., Pivodic, A., de Maré, H.K. et al. Infant body composition relationship to maternal adipokines and fat mass: the PONCH study. Pediatr Res 89, 1756–1764 (2021). https://doi.org/10.1038/s41390-020-01115-9
Received:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-020-01115-9