Abstract
Background
We aimed to identify potential risk factors for recurrent respiratory tract infection among Chinese preschool-aged children, and further to construct a nomogram prediction model.
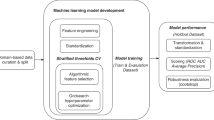
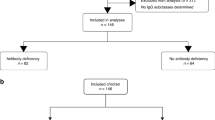
Methods
This is a cross-sectional survey conducted in Beijing. Utilizing a stratified cluster random sampling strategy, a total of 7222 children from 20 kindergartens were enrolled. Data are analyzed by STATA software and R language.
Results
Five independent factors were identified to be significantly associated with recurrent respiratory tract infection risk overall and by pathogenic sites. The significant odds of recurrent respiratory tract infection was 8.31 (95% confidence interval [CI]: 5.69–12.12, P < 0.001), 2.31 (2.06–2.58, P < 0.001), 1.72 (1.48–1.99, P < 0.001), 1.24 (1.08–1.43, P = 0.002), and 1.19 (1.09–1.31, P < 0.001) for asthma, allergy, initial use of antibiotics <6 months, breastfeeding duration <6 months, and maternal body mass index, respectively. Besides the leading role played by asthma, allergy, initial use of antibiotics, and breastfeeding might exert a graded, dose-dependent effect on recurrent respiratory tract infection susceptibility.
Conclusions
We have identified five potential risk factors for the risk of recurrent respiratory tract infection from 7222 preschool-aged Chinese children. Notably, asthma plays a leading role, and allergy, initial use of antibiotics, and breastfeeding might exert a graded, dose-dependent effect on recurrent respiratory tract infection susceptibility.
Impact
-
This is the first report of examining the joint contribution of multiple potential risk factors to recurrent respiratory tract infection among Chinese preschool-aged children.
-
We have identified five potential risk factors for the risk of recurrent respiratory tract infection via analyzing survey data from 7222 preschool-aged Chinese children.
-
Asthma plays a leading role, and allergy, initial use of antibiotics, and breastfeeding might exert a graded, dose-dependent effect on recurrent respiratory tract infection susceptibility.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Walker, C. L. F. et al. Global burden of childhood pneumonia and diarrhoea. Lancet 381, 1405–1416 (2013).
Marengo, R., Ortega Martell, J. A. & Esposito, S. Paediatric recurrent ear, nose and throat infections and complications: can we do more? Infect. Dis. Ther. 9, 275–290 (2020).
Collaborators, G. B. D. L. R. I. Estimates of the global, regional, and national morbidity, mortality, and aetiologies of lower respiratory infections in 195 countries, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Infect. Dis. 18, 1191–1210 (2018).
Liu, L. et al. Global, regional, and national causes of child mortality in 2000-13, with projections to inform post-2015 priorities: an updated systematic analysis. Lancet 385, 430–440 (2015).
Rudan, I. et al. Epidemiology and etiology of childhood pneumonia in 2010: estimates of incidence, severe morbidity, mortality, underlying risk factors and causative pathogens for 192 countries. J. Glob. Health 3, 010401 (2013).
Shi, T. et al. Risk factors for respiratory syncytial virus associated with acute lower respiratory infection in children under five years: systematic review and meta-analysis. J. Glob. Health 5, 020416 (2015).
Patria, M. F. & Esposito, S. Recurrent lower respiratory tract infections in children: a practical approach to diagnosis. Paediatr. Respir. Rev. 14, 53–60 (2013).
Karevold, G., Kvestad, E., Nafstad, P. & Kvaerner, K. J. Respiratory infections in schoolchildren: co-morbidity and risk factors. Arch. Dis. Child 91, 391–395 (2006).
Forssell, G., Hakansson, A. & Mansson, N. O. Risk factors for respiratory tract infections in children aged 2-5 years. Scand. J. Prim. Health Care 19, 122–125 (2001).
Ruskamp, J. et al. Neonatal total IgE and respiratory tract infections in children with intrauterine smoke exposure. Arch. Dis. Child 95, 427–431 (2010).
Duijts, L. et al. Maternal smoking in prenatal and early postnatal life and the risk of respiratory tract infections in infancy. The Generation R study. Eur. J. Epidemiol. 23, 547–555 (2008).
de Benedictis, F. M. & Bush, A. Recurrent lower respiratory tract infections in children. BMJ 362, k2698 (2018).
de Martino, M. & Ballotti, S. The child with recurrent respiratory infections: normal or not? Pediatr. Allergy Immunol. 18(Suppl. 18), 13–18 (2007).
Li, H., Ji, C. Y., Zong, X. N. & Zhang, Y. Q. Body mass index growth curves for Chinese children and adolescents aged 0 to 18 years. Zhonghua Er Ke Za Zhi 47, 493–498 (2009).
Oldroyd, J., Renzaho, A. & Skouteris, H. Low and high birth weight as risk factors for obesity among 4 to 5-year-old Australian children: does gender matter? Eur. J. Pediatr. 170, 899–906 (2011).
Altman, D. G. & Bland, J. M. Interaction revisited: the difference between two estimates. BMJ 326, 219 (2003).
Vickers, A. J. & Elkin, E. B. Decision curve analysis: a novel method for evaluating prediction models. Med. Decis. Making 26, 565–574 (2006).
Zhou, B. F. & Cooperative Meta-Analysis Group of the Working Group on Obesity in C. Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults-study on optimal cut-off points of body mass index and waist circumference in Chinese adults. Biomed. Environ. Sci. 15, 83–96 (2002).
World Health Organization. The Optimal Duration of Exclusive Breastfeeding: Report of an Expert Consultation (World Health Organization, Geneva, 2001).
Kummeling, I. et al. Early life exposure to antibiotics and the subsequent development of eczema, wheeze, and allergic sensitization in the first 2 years of life: the KOALA Birth Cohort Study. Pediatrics 119, e225–e231 (2007).
Toivonen, L. et al. Burden of recurrent respiratory tract infections in children: a prospective cohort study. Pediatr. Infect. Dis. J. 35, e362–e369 (2016).
Ciftci, E. et al. Underlying causes of recurrent pneumonia in Turkish children in a university hospital. J. Trop. Pediatr. 49, 212–215 (2003).
Cabezuelo Huerta, G., Vidal Mico, S., Abeledo, Gomez, A. & Frontera Izquierdo, P. Underlying causes of recurrent pneumoni. Pediatrics 63, 409–412 (2005).
Hoving, M. F. & Brand, P. L. Causes of recurrent pneumonia in children in a general hospital. J. Paediatr. Child Health 49, E208–E212 (2013).
Heffelfinger, J. D. et al. Evaluation of children with recurrent pneumonia diagnosed by World Health Organization criteria. Pediatr. Infect. Dis. J. 21, 108–112 (2002).
de Oliveira, T. B., Klering, E. A. & da Veiga, A. B. G. Is recurrent respiratory infection associated with allergic respiratory disease? J. Asthma 56, 160–166 (2019).
Dellepiane, R. M. et al. Atopy in preschool Italian children with recurrent respiratory infections. Pediatr. Med. Chir. 31, 161–164 (2009).
Ciprandi, G., Tosca, M. A. & Fasce, L. Allergic children have more numerous and severe respiratory infections than non-allergic children. Pediatr. Allergy Immunol. 17, 389–391 (2006).
Rantala, A., Jaakkola, J. J. & Jaakkola, M. S. Respiratory infections in adults with atopic disease and IgE antibodies to common aeroallergens. PLoS ONE 8, e68582 (2013).
Bartlett, N. W. et al. Mouse models of rhinovirus-induced disease and exacerbation of allergic airway inflammation. Nat. Med. 14, 199–204 (2008).
Bossios, A. et al. Rhinovirus infection and house dust mite exposure synergize in inducing bronchial epithelial cell interleukin-8 release. Clin. Exp. Allergy 38, 1615–1626 (2008).
Laoukili, J. et al. IL-13 alters mucociliary differentiation and ciliary beating of human respiratory epithelial cells. J. Clin. Invest. 108, 1817–1824 (2001).
Chantry, C. J., Howard, C. R. & Auinger, P. Full breastfeeding duration and associated decrease in respiratory tract infection in US children. Pediatrics 117, 425–432 (2006).
Lopez-Alarcon, M., Villalpando, S. & Fajardo, A. Breast-feeding lowers the frequency and duration of acute respiratory infection and diarrhea in infants under six months of age. J. Nutr. 127, 436–443 (1997).
Kovar, M. G., Serdula, M. K., Marks, J. S. & Fraser, D. W. Review of the epidemiologic evidence for an association between infant feeding and infant health. Pediatrics 74, 615–638 (1984).
Nutrition, E. C. O. et al. Breast-feeding: a commentary by the ESPGHAN Committee on Nutrition. J. Pediatr. Gastroenterol. Nutr. 49, 112–125 (2009).
Freinkel, N. Banting Lecture 1980. Of pregnancy and progeny. Diabetes 29, 1023–1035 (1980).
Barker, D. J. The origins of the developmental origins theory. J. Intern. Med. 261, 412–417 (2007).
Alfaradhi, M. Z. & Ozanne, S. E. Developmental programming in response to maternal overnutrition. Front. Genet. 2, 27 (2011).
Versporten, A. et al. The Worldwide Antibiotic Resistance and Prescribing in European Children (ARPEC) point prevalence survey: developing hospital-quality indicators of antibiotic prescribing for children. J. Antimicrob. Chemother. 71, 1106–1117 (2016).
Ahmadizar, F. et al. Early life antibiotic use and the risk of asthma and asthma exacerbations in children. Pediatr. Allergy Immunol. 28, 430–437 (2017).
O’Dwyer, D. N., Dickson, R. P. & Moore, B. B. The lung microbiome, immunity, and the pathogenesis of chronic lung disease. J. Immunol. 196, 4839–4847 (2016).
Gollwitzer, E. S. & Marsland, B. J. Impact of early-life exposures on immune maturation and susceptibility to disease. Trends Immunol. 36, 684–696 (2015).
McFadden, J. P. et al. T helper cell 2 immune skewing in pregnancy/early life: chemical exposure and the development of atopic disease and allergy. Br. J. Dermatol 172, 584–591 (2015).
Jordan, S., Storey, M. & Morgan, G. Antibiotics and allergic disorders in childhood. Open Nurs. J. 2, 48–57 (2008).
Jedrychowski, W. et al. Wheezing and asthma may be enhanced by broad spectrum antibiotics used in early childhood. Concept and results of a pharmacoepidemiology study. J. Physiol. Pharmacol. 62, 189–195 (2011).
Acknowledgements
We are grateful to all participating children and their parents or guardians for their cooperation and willingness, as well as kindergarten teachers and health physicians for their great help.
Author information
Authors and Affiliations
Contributions
Z.Z. planned and designed the study, and directed its implementation. Z.Z. drafted the protocol. B.Z., K.W., Y.Y., J.Z., and Z.Z. obtained statutory and ethics approvals. B.Z. and W.N. contributed to data acquisition. B.Z., F.L., and W.N. conducted statistical analyses. B.Z., K.W., Y.Y., Y.W., J.Z., F.L., and W.N. did the data preparation and quality control. B.Z. and W.N. wrote the manuscript. All authors read and approved the final manuscript prior to submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Patient consent
Written informed consent was obtained from the parents or guardians of study children prior to participation.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Zhou, B., Niu, W., Liu, F. et al. Risk factors for recurrent respiratory tract infection in preschool-aged children. Pediatr Res 90, 223–231 (2021). https://doi.org/10.1038/s41390-020-01233-4
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-020-01233-4
This article is cited by
-
Preparation of spleen aminopeptide-loaded pH-responsive oral hydrogel microspheres for improving recurrent respiratory infection in children
Scientific Reports (2026)
-
Factors associated with allergic diseases in Chinese children aged 6-14 years
BMC Public Health (2025)
-
Recurrent upper respiratory tract infections in early childhood: a newly defined clinical condition
Italian Journal of Pediatrics (2024)
-
“She mimicked the manipulations on my hand”: fostering embodied care among children with recurrent acute respiratory tract infections in Southern China
BMC Complementary Medicine and Therapies (2024)
-
Association of low physical activity with higher respiratory tract infections frequency among pre-school children
Pediatric Research (2023)