Abstract
Background
The impact of prenatal opioid exposure on brain development remains poorly understood.
Methods
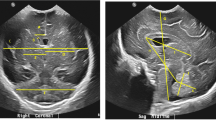
We conducted a prospective study of term-born infants with and without prenatal opioid exposure. Structural brain MRI was performed between 40 and 48 weeks postmenstrual age. T2-weighted images were processed using the Developing Human Connectome Project structural pipeline. We compared 63 relative regional brain volumes between groups.
Results
Twenty-nine infants with prenatal opioid exposure and 42 unexposed controls were included. The groups had similar demographics, except exposed infants had lower birth weights, more maternal smoking and maternal Hepatitis C, fewer mothers with a college degree, and were more likely non-Hispanic White. After controlling for sex, postmenstrual age at scan, birth weight, and maternal education, exposed infants had significantly smaller relative volumes of the deep gray matter, bilateral thalamic ventrolateral nuclei, bilateral insular white matter, bilateral subthalamic nuclei, brainstem, and cerebrospinal fluid. Exposed infants had larger relative volumes of the right cingulate gyrus white matter and left occipital lobe white matter.
Conclusions
Infants with prenatal opioid exposure had smaller brain volumes in multiple regions compared to controls, with two regions larger in the opioid-exposed group. Further research should focus on the relative contributions of maternal opioids and other exposures.
Impact
-
Prenatal opioid exposure is associated with developmental and behavioral consequences, but the direct effects of opioids on the developing human brain are poorly understood.
-
Prior small studies using MRI have shown smaller regional brain volumes in opioid-exposed infants and children.
-
After controlling for covariates, infants with prenatal opioid exposure scanned at 40–48 weeks postmenstrual age had smaller brain volumes in multiple regions compared to controls, with two regions larger in the opioid-exposed group.
-
This adds to the literature showing potential impact of prenatal opioid exposure on the developing brain.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Change history
08 December 2020
A Correction to this paper has been published: https://doi.org/10.1038/s41390-020-01297-2
References
Honein, M. A., Boyle, C. & Redfield, R. R. Public health surveillance of prenatal opioid exposure in mothers and infants. Pediatrics 143, e20183801 (2019).
Concheiro, M. et al. Maternal buprenorphine dose, placenta buprenorphine, and metabolite concentrations and neonatal outcomes. Ther. Drug Monit. 32, 206–215 (2010).
Chaves, C., Remiao, F., Cisternino, S. & Decleves, X. Opioids and the blood-brain barrier: a dynamic interaction with consequences on drug disposition in brain. Curr. Neuropharmacol. 15, 1156–1173 (2017).
Yeoh, S. L. et al. Cognitive and motor outcomes of children with prenatal opioid exposure: a systematic review and meta-analysis. JAMA Netw. Open 2, e197025 (2019).
Larson, J. J. et al. Cognitive and behavioral impact on children exposed to opioids during pregnancy. Pediatrics 144, e20190514 (2019).
Wu, V. W., Mo, Q., Yabe, T., Schwartz, J. P. & Robinson, S. E. Perinatal opioids reduce striatal nerve growth factor content in rat striatum. Eur. J. Pharmacol. 414, 211–214 (2001).
Wu, C. C. et al. Prenatal buprenorphine exposure decreases neurogenesis in rats. Toxicol. Lett. 225, 92–101 (2014).
Vestal-Laborde, A. A., Eschenroeder, A. C., Bigbee, J. W., Robinson, S. E. & Sato-Bigbee, C. The opioid system and brain development: effects of methadone on the oligodendrocyte lineage and the early stages of myelination. Dev. Neurosci. 36, 409–421 (2014).
Sanchez, E. S., Bigbee, J. W., Fobbs, W., Robinson, S. E. & Sato-Bigbee, C. Opioid addiction and pregnancy: perinatal exposure to buprenorphine affects myelination in the developing brain. Glia 56, 1017–1027 (2008).
Hu, S., Sheng, W. S., Lokensgard, J. R. & Peterson, P. K. Morphine induces apoptosis of human microglia and neurons. Neuropharmacology 42, 829–836 (2002).
Younger, J. W. et al. Prescription opioid analgesics rapidly change the human brain. Pain 152, 1803–1810 (2011).
Lin, J. C. et al. One month of oral morphine decreases gray matter volume in the right amygdala of individuals with low back pain: confirmation of previously reported magnetic resonance imaging results. Pain. Med. 17, 1497–1504 (2016).
Sirnes, E. et al. Brain morphology in school-aged children with prenatal opioid exposure: a structural MRI study. Early Hum. Dev. 106-107, 33–39 (2017).
Walhovd, K. B. et al. Volumetric cerebral characteristics of children exposed to opiates and other substances in utero. Neuroimage 36, 1331–1344 (2007).
Yuan, Q. et al. Do maternal opioids reduce neonatal regional brain volumes? A pilot study. J. Perinatol. 34, 909–913 (2014).
Makropoulos, A. et al. The developing human connectome project: a minimal processing pipeline for neonatal cortical surface reconstruction. Neuroimage 173, 88–112 (2018).
Makropoulos, A. et al. Automatic whole brain MRI segmentation of the developing neonatal brain. IEEE Trans. Med Imaging 33, 1818–1831 (2014).
Kline, J. E., Illapani, V. S. P., He, L., Altaye, M. & Parikh, N. A. Retinopathy of prematurity and bronchopulmonary dysplasia are independent antecedents of cortical maturational abnormalities in very preterm infants. Sci. Rep. 9, 19679 (2019).
Rothman, K. J. No adjustments are needed for multiple comparisons. Epidemiology 1, 43–46 (1990).
Cunha-Oliveira, T., Rego, A. C. & Oliveira, C. R. Cellular and molecular mechanisms involved in the neurotoxicity of opioid and psychostimulant drugs. Brain Res. Rev. 58, 192–208 (2008).
Brown, G. G., Jacobus, J. & McKenna, B. Structural imaging for addiction medicine: from neurostructure to neuroplasticity. Prog. Brain Res. 224, 105–127 (2016).
Tramullas, M., Martínez-Cué, C. & Hurlé, M. A. Chronic administration of heroin to mice produces up-regulation of brain apoptosis-related proteins and impairs spatial learning and memory. Neuropharmacology 54, 640–652 (2008).
Wang, Y. & Han, T. Z. Prenatal exposure to heroin in mice elicits memory deficits that can be attributed to neuronal apoptosis. Neuroscience 160, 330–338 (2009).
Eisch, A. J., Barrot, M., Schad, C. A., Self, D. W. & Nestler, E. J. Opiates inhibit neurogenesis in the adult rat hippocampus. Proc. Natl Acad. Sci. USA 97, 7579–7584 (2000).
Liao, D., Lin, H., Law, P. Y. & Loh, H. H. Mu-opioid receptors modulate the stability of dendritic spines. Proc. Natl Acad. Sci. USA 102, 1725–1730 (2005).
Liao, D. et al. Distinct effects of individual opioids on the morphology of spines depend upon the internalization of mu opioid receptors. Mol. Cell Neurosci. 35, 456–469 (2007).
Jantzie, L. L. et al. Prenatal opioid exposure: the next neonatal neuroinflammatory disease. Brain Behav. Immun. 84, 45–58 (2020).
Wollman, S. C. et al. White matter abnormalities in long-term heroin users: a preliminary neuroimaging meta-analysis. Am. J. Drug Alcohol Abus. 41, 133–138 (2015).
Grandjean, J. et al. Chronic psychosocial stress in mice leads to changes in brain functional connectivity and metabolite levels comparable to human depression. Neuroimage 142, 544–552 (2016).
Bierer, L. M. et al. White matter abnormalities in Gulf War veterans with posttraumatic stress disorder: a pilot study. Psychoneuroendocrinology 51, 567–576 (2015).
Monnelly, V. J. et al. Prenatal methadone exposure is associated with altered neonatal brain development. Neuroimage Clin. 18, 9–14 (2018).
Walhovd, K. B., Watts, R., Amlien, I. & Woodward, L. J. Neural tract development of infants born to methadone-maintained mothers. Pediatr. Neurol. 47, 1–6 (2012).
Towers, C. V. et al. Neonatal head circumference in newborns with neonatal abstinence syndrome. Pediatrics 143, e20180541 (2019).
Hytinantti, T. et al. Neonatal outcome of 58 infants exposed to maternal buprenorphine in utero. Acta Paediatr. 97, 1040–1044 (2008).
Garrison, L. et al. Fetal growth outcomes in a cohort of polydrug- and opioid-dependent patients. J. Reprod. Med. 61, 311–319 (2016).
Huang, A. S., Mitchell, J. A., Haber, S. N., Alia-Klein, N. & Goldstein, R. Z. The thalamus in drug addiction: from rodents to humans. Philos. Trans. R. Soc. Lond. B Biol. Sci. 373, 20170028 (2018).
Haber, S. & McFarland, N. R. The place of the thalamus in frontal cortical-basal ganglia circuits. Neuroscientist 7, 315–324 (2001).
Prosser, J., London, E. D. & Galynker, I. I. Sustained attention in patients receiving and abstinent following methadone maintenance treatment for opiate dependence: performance and neuroimaging results. Drug Alcohol Depend. 104, 228–240 (2009).
Wollman, S. C. et al. Gray matter abnormalities in opioid-dependent patients: a neuroimaging meta-analysis. Am. J. Drug Alcohol Abus. 43, 505–517 (2017).
Koob, G. F. & Volkow, N. D. Neurobiology of addiction: a neurocircuitry analysis. Lancet Psychiatry 3, 760–773 (2016).
Ting-A-Kee, R. & van der Kooy, D. The neurobiology of opiate motivation. Cold Spring Harb. Perspect. Med. 2, a012096 (2012).
Droutman, V., Read, S. J. & Bechara, A. Revisiting the role of the insula in addiction. Trends Cogn. Sci. 19, 414–420 (2015).
Scott, D. & Hiroi, N. Deconstructing craving: dissociable cortical control of cue reactivity in nicotine addiction. Biol. Psychiatry 69, 1052–1059 (2011).
Naqvi, N. H., Rudrauf, D., Damasio, H. & Bechara, A. Damage to the insula disrupts addiction to cigarette smoking. Science 315, 531–534 (2007).
Lyoo, I. K. et al. Prefrontal and temporal gray matter density decreases in opiate dependence. Psychopharmacology 184, 139–144 (2006).
Gardini, S. & Venneri, A. Reduced grey matter in the posterior insula as a structural vulnerability or diathesis to addiction. Brain Res. Bull. 87, 205–211 (2012).
Goldstein, R. Z. & Volkow, N. D. Dysfunction of the prefrontal cortex in addiction: neuroimaging findings and clinical implications. Nat. Rev. Neurosci. 12, 652–669 (2011).
Takemura, H. et al. Occipital white matter tracts in human and macaque. Cereb. Cortex 27, 3346–3359 (2017).
Hamilton, R. et al. Ophthalmic, clinical and visual electrophysiological findings in children born to mothers prescribed substitute methadone in pregnancy. Br. J. Ophthalmol. 94, 696–700 (2010).
McGlone, L. et al. Visual outcome in infants born to drug-misusing mothers prescribed methadone in pregnancy. Br. J. Ophthalmol. 98, 238–245 (2014).
Spiteri Cornish, K., Hrabovsky, M., Scott, N. W., Myerscough, E. & Reddy, A. R. The short- and long-term effects on the visual system of children following exposure to maternal substance misuse in pregnancy. Am. J. Ophthalmol. 156, 190–194 (2013).
El Marroun, H. et al. Prenatal tobacco exposure and brain morphology: a prospective study in young children. Neuropsychopharmacology 39, 792–800 (2014).
Nelson, L. F. et al. Cognitive outcomes of young children after prenatal exposure to medications for opioid use disorder: a systematic review and meta-analysis. JAMA Netw. Open 3, e201195 (2020).
Holz, N. E. et al. Effect of prenatal exposure to tobacco smoke on inhibitory control: neuroimaging results from a 25-year prospective study. JAMA Psychiatry 71, 786–796 (2014).
Bakhireva, L. N. et al. Prevalence of alcohol use in pregnant women with substance use disorder. Drug Alcohol Depend. 187, 305–310 (2018).
Acknowledgements
This work was funded by KL2 TR001426 (to S.L.M.), R01 NS094200 (to N.A.P.), and R01 NS096037 (to N.A.P.).
Author information
Authors and Affiliations
Contributions
S.L.M. conceptualized and designed the study, drafted the initial manuscript, and revised the manuscript for important intellectual content. J.E.K. supervised data analysis, developed the figures, and revised the manuscript for important intellectual content. A.B. performed data analysis and revised the manuscript for important intellectual content. B.M.K.-F supervised data acquisition and revised the manuscript for important intellectual content. J.A.T. implemented the MRI protocol, supervised data acquisition, and revised the manuscript for important intellectual content. M.A. performed statistical analysis and revised the manuscript for important intellectual content. L.H. collected data and revised the manuscript for important intellectual content. N.A.P. supervised data collection and analysis, interpreted the data, and revised the manuscript for important intellectual content. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent statement
Consent was required from a parent/legal guardian for this study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Merhar, S.L., Kline, J.E., Braimah, A. et al. Prenatal opioid exposure is associated with smaller brain volumes in multiple regions. Pediatr Res 90, 397–402 (2021). https://doi.org/10.1038/s41390-020-01265-w
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-020-01265-w
This article is cited by
-
Neurodevelopmental challenges at age four following fetal exposure to maternal opioid maintenance treatment
Pediatric Research (2025)
-
Real-time aggression in youth and its connection to region-specific structural brain alterations
Discover Mental Health (2025)
-
Ultrasound evaluation of brain parenchyma in preterm infants with prenatal opioid exposure
Journal of Perinatology (2024)
-
Association of medication-assisted treatment and short acting opioids with newborn head circumference and birth weight
Journal of Perinatology (2023)
-
Outcomes of Babies with Opioid Exposure (OBOE): protocol of a prospective longitudinal cohort study
Pediatric Research (2023)