Abstract
Background
Though prenatal antidepressant exposure has been associated with adverse developmental outcomes, the extent to which the effects are due to prenatal drug exposure or underlying maternal mood disturbances is unclear.
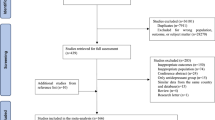
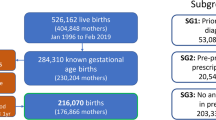
Methods
This was a population-based retrospective cohort study using administrative data from British Columbia, Canada (n = 94,712). Analyses were designed to remove confounding effects of prenatal antidepressant exposure from maternal mood. First, children prenatally exposed to antidepressants were matched to unexposed children using high-dimensional propensity scores (HDPS). Second, children whose mothers had used antidepressants throughout pregnancy were compared against those whose mothers discontinued treatment.
Results
In all, 3.87% (n = 3661) of children in the overall study population were prenatally exposed to antidepressants. In both analyses, we report increased odds for lower levels of physical independence (HDPS: OR, 1.14; 95% CI, 1.00–1.30; continuers/discontinuers: OR, 1.14; 95% CI, 0.99–1.32), and higher levels of anxious behaviors (HDPS: OR, 1.30; 95% CI, 1.01–1.66; continuers/discontinuers: OR, 1.32; 95% CI, 1.01–1.72) associated with antidepressant use in pregnancy. All other relationships were not significant using these methods.
Conclusions
Prenatal antidepressant exposure was selectively associated with worse anxious behaviors and physical independence at kindergarten age, with no effects on other developmental domains. Effects are also likely attributable to maternal mental illness severity or other unmeasured confounding factors.
Impact
-
Selective associations between prenatal antidepressant exposure and children’s anxiety and physical independence at kindergarten were identified, with no impact on other developmental domains.
-
Contradictory reports have emerged regarding the association of adverse child outcomes with prenatal antidepressant exposure. These inconsistencies may be due to differences in control for confounding.
-
Effects of prenatal antidepressant exposure on anxious behaviors and physical independence are likely also attributable to severity of underlying maternal mood disorders, highlighting the importance of maternal mental health for developmental health.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Underwood, L., Waldie, K., D’Souza, S., Peterson, E. R. & Morton, S. A review of longitudinal studies on antenatal and postnatal depression. Arch. Womens Ment. Health 19, 711–720 (2016).
Smolina, K., Hanley, G. E., Mintzes, B., Oberlander, T. F. & Morgan, S. Trends and determinants of prescription drug use during pregnancy and postpartum in British Columbia, 2002-2011: a population-based cohort study. PLoS ONE 10, e0128312 (2015).
Hanley, G. E. & Mintzes, B. Patterns of psychotropic medicine use in pregnancy in the United States from 2006 to 2011 among women with private insurance. BMC Pregnancy Childbirth 14, 242 (2014).
Cohen, L. S. et al. Relapse of major depression during pregnancy in women who maintain or discontinue antidepressant treatment. JAMA 295, 499–507 (2006).
Roca, A. et al. Unplanned pregnancy and discontinuation of SSRIs in pregnant women with previously treated affective disorder. J. Affect. Disord. 150, 807–813 (2013).
Bonari, L. et al. Perinatal risks of untreated depression during pregnancy. Can. J. Psychiatry 49, 726–735 (2004).
Rotem-Kohavi, N. & Oberlander, T. F. Variations in neurodevelopmental outcomes in children with prenatal SSRI antidepressant exposure. Birth Defects Res. 109, 909–923 (2017).
Boukhris, T., Sheehy, O., Mottron, L. & Berard, A. Antidepressant use during pregnancy and the risk of autism spectrum disorder in children. JAMA Pediatr. 170, 117–124 (2016).
Man, K. K. C. et al. Prenatal antidepressant use and risk of attention-deficit/hyperactivity disorder in offspring: population based cohort study. BMJ 357, j2350 (2017).
Handal, M. et al. Motor development in children prenatally exposed to selective serotonin reuptake inhibitors: a large population-based pregnancy cohort study. BJOG 123, 1908–1917 (2016).
Skurtveit, S., Selmer, R., Roth, C., Hernandez-Diaz, S. & Handal, M. Prenatal exposure to antidepressants and language competence at age three: results from a large population-based pregnancy cohort in Norway. BJOG 121, 1621–1631 (2014).
Hurault-Delarue, C. et al. Psychomotor developmental effects of prenatal exposure to psychotropic drugs: a study in EFEMERIS database. Fundam. Clin. Pharmacol. 30, 476–482 (2016).
Brown, H. K., Hussain-Shamsy, N., Lunsky, Y., Dennis, C. E. & Vigod, S. N. The association between antenatal exposure to selective serotonin reuptake inhibitors and autism: a systematic review and meta-analysis. J. Clin. Psychiatry 78, e48–e58 (2017).
Grzeskowiak, L. E. et al. Prenatal antidepressant exposure and child behavioural outcomes at 7 years of age: a study within the Danish National Birth Cohort. BJOG 123, 1919–1928 (2016).
Liu, X. et al. Antidepressant use during pregnancy and psychiatric disorders in offspring: Danish nationwide register based cohort study. BMJ 358, j3668 (2017).
Jarde, A. et al. Neonatal outcomes in women with untreated antenatal depression compared with women without depression: a systematic review and meta-analysis. JAMA Psychiatry 73, 826–837 (2016).
Bennett, I. M., Marcus, S. C., Palmer, S. C. & Coyne, J. C. Pregnancy-related discontinuation of antidepressants and depression care visits among Medicaid recipients. Psychiatr. Serv. 61, 386–391 (2010).
Cheng, T. L. & Goodman, E. Race, ethnicity, and socioeconomic status in research on child health. Pediatrics 135, e225–e237 (2015).
Brown, H. K. et al. Association between serotonergic antidepressant use during pregnancy and autism spectrum disorder in children. JAMA 317, 1544–1552 (2017).
Sujan, A. C. et al. Associations of maternal antidepressant use during the first trimester of pregnancy with preterm birth, small for gestational age, autism spectrum disorder, and attention-deficit/hyperactivity disorder in offspring. JAMA 317, 1553–1562 (2017).
Hviid, A., Melbye, M. & Pasternak, B. Use of selective serotonin reuptake inhibitors during pregnancy and risk of autism. N. Engl. J. Med. 369, 2406–2415 (2013).
Viktorin, A., Uher, R., Reichenberg, A., Levine, S. Z. & Sandin, S. Autism risk following antidepressant medication during pregnancy. Psychol. Med. 47, 2787–2796 (2017).
Guhn, M. et al. Examining the social determinants of children’s developmental health: protocol for building a pan-Canadian population-based monitoring system for early childhood development. BMJ Open 6, e012020 (2016).
Janus, M. & Offord, D. R. Development and psychometric properties of the Early Development Instrument (EDI): a measure of children’s school readiness. Can. J. Behav. Sci. 39, 1–22 (2007).
Brinkman, S. et al. Associations between the early development instrument at age 5, and reading and numeracy skills at ages 8, 10 and 12: a prospective linked data study. Child Indic. Res. 6, 695–708 (2013).
Forer, B. & Zumbo, B. Validation of multilevel constructs: validation methods and empirical findings for the EDI. Soc. Indic. Res. 103, 231 (2011).
Janus, M., Walsh, C., & Duku, E. Early Development Instrument: Factor structure, sub-domains and Multiple Challenge Index (Offord Centre for Child Studies, McMaster University, Hamilton, ON, 2005).
Schneeweiss, S. et al. High-dimensional propensity score adjustment in studies of treatment effects using health care claims data. Epidemiology 20, 512–522 (2009).
Austin, P. C. Optimal caliper widths for propensity-score matching when estimating differences in means and differences in proportions in observational studies. Pharmacol. Stat. 10, 150–161 (2011).
Austin, P. C. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat. Med. 28, 3083–3107 (2009).
SAS System for Windows 9.4 (SAS Institute, Cary, NC, 2014).
Hanley, G. E., Brain, U. & Oberlander, T. F. Prenatal exposure to serotonin reuptake inhibitor antidepressants and childhood behavior. Pediatr. Res. 78, 174–180 (2015).
Brandlistuen, R. E. et al. Behavioural effects of fetal antidepressant exposure in a Norwegian cohort of discordant siblings. Int. J. Epidemiol. 44, 1397–1407 (2015).
Galbally, M., Lewis, A. J. & Buist, A. Child developmental outcomes in preschool children following antidepressant exposure in pregnancy. Aust. NZ J. Psychiatry 49, 642–650 (2015).
Hanley, G. E., Brain, U. & Oberlander, T. F. Infant developmental outcomes following prenatal exposure to antidepressants, and maternal depressed mood and positive affect. Early Hum. Dev. 89, 519–524 (2013).
Viktorin, A. et al. Association of antidepressant medication use during pregnancy with intellectual disability in offspring. JAMA Psychiatry 74, 1031–1038 (2017).
Rommel, A. S., Bergink, V., Liu, X., Munk-Olsen, T. & Molenaar, N. M. Long-term effects of intrauterine exposure to antidepressants on physical, neurodevelopmental, and psychiatric outcomes: a systematic review. J. Clin. Psychiatry 81, 19r12965 (2020).
Ansorge, M. S., Zhou, M., Lira, A., Hen, R. & Gingrich, J. A. Early-life blockade of the 5-HT transporter alters emotional behavior in adult mice. Science 306, 879–881 (2004).
Brummelte, S., Mc Glanaghy, E., Bonnin, A. & Oberlander, T. F. Developmental changes in serotonin signaling: Implications for early brain function, behavior and adaptation. Neuroscience 342, 212–231 (2017).
Hanley, G. E., Park, M. & Oberlander, T. F. Socieconomic status and psychotropic medicine use during pregnancy: a population-based study in British Columbia, Canada. Arch. Womens Ment. Health 23, 689–697 (2020).
Acknowledgements
This research was funded by the Canadian Institutes of Health Research (CIHR) Grant 117135. M.P. was supported by a CIHR Doctoral Research Award. G.E.H. is supported by a Canadian Institutes for Health Research New Investigator Award. T.F.O. is the R. Howard Webster Professor in Brain Imaging and Child Development. The authors also thank Ursula Brain for her careful review of the manuscript.
Author information
Authors and Affiliations
Contributions
M.P. and T.F.O. conceptualized and designed the study and produced the first draft of the manuscript. M.P. conducted all analyses. G.E.H. and T.F.O. were involved in data acquisition. All authors participated in critical review and interpretation of results and revisions and approval of the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Patient consent statement
Patient consent was not required as data were de-identified, anonymized, and from secondary sources.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Park, M., Hanley, G.E., Guhn, M. et al. Prenatal antidepressant exposure and child development at kindergarten age: a population-based study. Pediatr Res 89, 1515–1522 (2021). https://doi.org/10.1038/s41390-020-01269-6
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-020-01269-6
This article is cited by
-
Impact of prenatal antidepressant exposure on trajectories of childhood emotions and behaviors: evidence from a birth cohort
Pediatric Research (2026)
-
Prenatal antidepressant exposure and neurodevelopmental problems in children: to get the right answer, we must ask the right question
Pediatric Research (2021)