Abstract
Background
The aim of this study was to investigate the association between race and severe neonatal opioid withdrawal syndrome (NOWS) in infants exposed to intrauterine opioids.
Methods
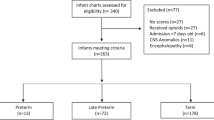
This is a prospective observational study on intrauterine opioid-exposed term infants. Exposure to opioids was based on maternal disclosure, urine, or umbilical cord drug screening. Severe NOWS was defined based on modified Finnegan scoring and the need for pharmacological intervention.
Results
One hundred and fifty mother–infant pairs, 60 Black and 90 White with history of opioid exposure during pregnancy, were included. More White than Black infants developed NOWS that required pharmacological treatment, 70 vs. 40%: RR = 1.75 (1.25–2.45). In adjusted analysis, there was no significant association between race and the development of severe NOWS in mothers who attended opioid maintenance treatment program (OMTP). However, in mothers who did not attend OMTP, White race remained a significant factor associated with the development of severe NAS, RR = 1.69 (1.06, 2.69).
Conclusions
Severe NOWS that required pharmacological intervention was significantly higher in White than in Black infants born to mothers who did not attend OMTP. Larger studies are needed to evaluate the association between social as well as genetic factors and the development of NOWS.
Impact
-
There is a significant association between race and development of severe NOWS.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Patrick, S. W., Davis, M. M., Lehman, C. U. & Cooper, W. O. Increasing incidence and geographic distribution of neonatal abstinence syndrome: United States 2009-2012. J. Perinatol. 35, 650–655 (2015).
Ramphul, K., Gonzalez Mejias, S. & Joynauth, J. An update on the burden of neonatal abstinence syndrome in the United States. Hospital Pediatr. 10, 1–4 (2020).
Hudak, M. L., Tan, R. C., The Committee on Drugs & The Committee on Fetus and Newborn. Neonatal drug withdrawal. Pediatrics 129, e540–e560 (2012).
Tolia, V. N. et al. Antenatal methadone vs buprenorphine exposure and length of hospital stay in infants admitted to the intensive care unit with neonatal abstinence syndrome. J. Perinatol. 38, 75–79 (2018).
Smid, M. C., Metz, T. D. & Gordon, A. J. Stimulant use in pregnancy- an under-recognized epidemic among pregnant women. Clin. Obstet. Gynecol. 62, 168–184 (2019).
Malek, A., Obrist, C., Wenzinger, S. & von Mandach, U. The impact of cocaine and heroin on placental transfer of methadone. Reprod. Biol. Endocrinol. 7, 1–9 (2009).
Volpe, J. J. Commentary-Marijuana use during pregnancy and premature birth: a problem likely to worsen. J. Neonatal Perinat. Med. 13, 1–3 (2020).
Jones, H. E. et al. Cigarette smoking in opioid-dependent pregnant women: neonatal and maternal outcome. Drug Alcohol Depend. 131, 271–277 (2013).
Wachman, E. M. et al. The relationship between maternal opioid agonists and psychiatric medications on length of hospitalization for neonatal abstinence syndrome. J. Addict. Med. 5, 293–299 (2011).
Benningfield, M. M. et al. Co-occurring psychiatric symptoms are associated with increased psychological, social, and medical impairment in opioid dependent pregnant women. Am. J. Addict. 19, 416–421 (2010).
Wachman, E. M. & Farrer, L. A. The genetics and epigenetics of neonatal abstinence syndrome. Semin. Fetal Neonatal Med. 24, 105–110 (2019).
Balyan, R. et al. CYP2D6 pharmacogenetic and oxycodone pharmacokinetics association study in pediatric surgical patients. Pharmacogenomics 18, 337–348 (2017).
Gibson, K. S., Stark, S., Kumar, D. & Bailit, J. L. The relationship between gestational age and the severity of neonatal abstinence syndrome. Addiction 112, 711–716 (2016).
Holbrook, A. & Kaltenbach, K. Gender and NAS: does sex matter? Drug Alcohol Depend. 112, 156–159 (2010).
Patrick, S. W. et al. Prescription opioid epidemic and infant outcomes. Pediatrics 135, 842–850 (2015).
Bogen, D. L., Hanusa, B. H., Baker, R., Medoff-Cooper, B. & Cohlan, B. Randomized clinical trial of standard-versus high-calorie formula for methadone-exposed infants: a feasibility study. Hospital Pediatr. 8, 7–14 (2018).
Bagley, S. M., Wachman, E. M., Holland, E. & Brogly, S. B. Review of the assessment and management of neonatal abstinence syndrome. Addict. Sci. Clin. Pract. 9, 1–10 (2014).
Grossman, M. R. et al. An initiative to improve the quality of care of infants with neonatal abstinence syndrome. Pediatrics 139, e1–e7 (2017).
Howard, M. B. et al. Impact of parental presence at infants’ bedside on neonatal abstinence syndrome. Hospital Pediatr. 7, 63–69 (2017).
Zimmermann-Baer, U., Notzli, U., Rentsch, K. & Bucher, H. U. Finnegan neonatal abstinence scoring system: normal values for first 3 days and weeks 5-6 in non-addicted infants. Addiction 105, 524–528 (2010).
Kushnir, A., Bleznak, J. L., Saslow, J. G. & Stahl, G. Nurses’ Finnegan scoring of newborns with neonatal abstinence syndrome not affected by time or day of week. Am. J. Perinatol. 37, 224–230 (2020).
McCarthy, J. J. et al. The use of serum methadone/methadone ratios to monitor changing perinatal pharmacokinetics. J. Addict. Med. 12, 241–246 (2018).
Jansson, L. M., Velez, M. & Harrow, C. The opioid-exposed newborn: assessment and pharmacologic management. J. Opioid Manag. 5, 47–55 (2009).
McCarthy, J. J., Leamon, M. H., Parr, M. S. & Anania, B. High-dose methadone maintenance in pregnancy: maternal and neonatal outcomes. Am. J. Obstet. Gynecol. 193, 606–610 (2005).
Patrick, S. W. et al. Association pf pregnancy and insurance status withtreatment access for opioid use disorder. JAMA Netw. Open 3, 1–12 (2020).
Welch, S. P. Interaction of the cannabinoid and opioid systems in the modulation of nociception. Int. Rev. Psychiatry 21, 143–151 (2009).
Cooper, Z. D. et al. Impact of co-administration of oxycodone and smoked cannabis on analgesia and abuse liability. Neuropsychpharmacology 43, 2046–2055 (2018).
Lofwall, M. R., Babalonis, S., Nuzzo, P. A., Elay, S. C. & Walsh, S. L. Opioid withdrawal suppression efficacy of oral dronabinol in opioid depenent humans. Drug Alcohol Depend. 1, 164–50 (2016).
Chasnoff, I. J., Landress, H. J. & Barrett, M. E. The prevalence of illicit-drug or alcohol use during pregnancy and discrepencies in mandatory reporting in Pinellas County, Florida. N. Engl. J. Med. 322, 1202–1206 (1990).
Plessinger, M. A. & Woods, J. R. Maternal, placental, and fetal pathophysiology of cocaine exposure during pregnancy. Clin. Obstet. Gynecol. 36, 267–277 (1993).
Parikh, A., Gopalakrishnan, A. A., Booth, A. & El-Metwally, D. Racial association and pharmacotherapy in neonatal opioid withdrawal syndrome. J. Perinatol. 39, 1370–1376 (2019).
Oei, J. L. et al. Dopamine D2 receptor gene polymorphisms in newborn infants of drug-using women. Arch. Dis. Child. Fetal Neonatal Ed. 97, F193–F198 (2012).
Venkatasubramanian, R. et al. ABCC3 and OCT1 genotypes influence pharmacokinetics of morphine in children. Pharmacogenomics 15, 1297–1309 (2014).
Wachman, E. M. et al. Association of maternal and infant variants in PNOC and COMT genes with neonatal abstinence syndrome severity. Am. J. Addict. 26, 42–49 (2017).
Cole, F. S., Wegner, D. J. & Davis, J. M. The genomics of neonatal abstinence syndrome. Front. Pediatr. 5, 1–4 (2017).
Sadhasivam, S. et al. Morphine clearance in children: does race or genetics matter? J. Opioid Manag. 8, 217–226 (2012).
Emoto, C. et al. Characterization of contributing factors to variability in morphine clearance through (physiologically based pharmacokinetic (PBPK) modeling implemented with OCT1 transporter. CPT Pharmacometrics Syst. Pharmacol. 6, 110–119 (2017).
Lewis, T., Dinh, J. & Leeder, J. S. Genetic determinants of fetal opiate exposure and risk of neonatal abstinence syndrome: Knowledge deficit and prospect for future. Clin. Pharmacol. Ther. 98, 309–320 (2015).
Hauser, K. F. & Knapp, P. E. Opiate drugs with abuse liability hijack the endogenous opioid system to disrupt neuronal and glial maturation in the central nervous system. Front. Pediatr. 5, 1–23 (2018).
Grossman, M. R., Berkwitt, A. K. & Osborn, R. R. Racial association and pharmacotherapy in neonatal opioid withdeawal syndrome: thinking beyond genetics. J. Perinatol. 40, 689–690 (2020).
Acknowledgements
We thank Gail Camp RN, Research Coordinator for obtaining consent form and gathering the data. We also thank the team of Social workers who help our mothers with OUD with their social needs.
Author information
Authors and Affiliations
Contributions
M.P. conceptualized and designed the study, coordinated and supervised data collection, initial analysis, drafted the initial manuscript, and reviewed and revised the final version of manuscript. M.T.E. and R.D. carried out the initial and final analysis and reviewed the final manuscript. D.R. designed the data collection, collected data, carried out the initial analysis, and critically reviewed the final manuscript. K.P.G. and L.D. collected data and critically reviewed the final manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent
Patient consent was required and was obtained per our IRB guidelines.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pourcyrous, M., Elabiad, M.T., Rana, D. et al. Racial differences in opioid withdrawal syndrome among neonates with intrauterine opioid exposure. Pediatr Res 90, 459–463 (2021). https://doi.org/10.1038/s41390-020-01279-4
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41390-020-01279-4
This article is cited by
-
Implicit Racial Bias in Evaluation of Neonatal Opioid Withdrawal Syndrome
Journal of Racial and Ethnic Health Disparities (2025)
-
Comparing maternal substance use and perinatal outcomes before and during the COVID-19 pandemic
Journal of Perinatology (2023)
-
Words matter
Pediatric Research (2022)