Abstract
Background
The neonatal resuscitation program (NRP) recommends interrupted chest compressions (CCs) with ventilation in the severely bradycardic neonate. The conventional 3:1 compression-to-ventilation (C:V) resuscitation provides 90 CCs/min, significantly lower than the intrinsic newborn heart rate (120–160 beats/min). Continuous CC with asynchronous ventilation (CCCaV) may improve the success of return of spontaneous circulation (ROSC).
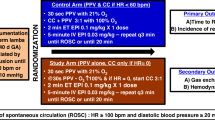
Methods
Twenty-two near-term fetal lambs were randomized to interrupted 3:1 C:V (90 CCs + 30 breaths/min) or CCCaV (120 CCs + 30 breaths/min). Asphyxiation was induced by cord occlusion. After 5 min of asystole, resuscitation began following NRP guidelines. The first dose of epinephrine was given at 6 min. Invasive arterial blood pressure and left carotid blood flow were continuously measured. Serial arterial blood gases were collected.
Results
Baseline characteristics between groups were similar. Rate of and time to ROSC was similar between groups. CCCaV was associated with a higher PaO2 (partial oxygen tension) (22 ± 5.3 vs. 15 ± 3.5 mmHg, p < 0.01), greater left carotid blood flow (7.5 ± 3.1 vs. 4.3 ± 2.6 mL/kg/min, p < 0.01) and oxygen delivery (0.40 ± 0.15 vs. 0.13 ± 0.07 mL O2/kg/min, p < 0.01) compared to 3:1 C:V.
Conclusions
In a perinatal asphyxiated cardiac arrest lamb model, CCCaV showed greater carotid blood flow and cerebral oxygen delivery compared to 3:1 C:V resuscitation.
Impact
-
In a perinatal asphyxiated cardiac arrest lamb model, CCCaV improved carotid blood flow and oxygen delivery to the brain compared to the conventional 3:1 C:V resuscitation.
-
Pre-clinical studies assessing neurodevelopmental outcomes and tissue injury comparing continuous uninterrupted chest compressions to the current recommended 3:1 C:V during newborn resuscitation are warranted prior to clinical trials.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Black, R. E. et al. Global, regional, and national causes of child mortality in 2008: a systematic analysis. Lancet 375, 1969–1987 (2010).
Bairoliya, N. & Fink, G. Causes of death and infant mortality rates among full-term births in the United States between 2010 and 2012: an observational study. PLoS Med. 15, e1002531 (2018).
Kleinman, M. E. et al. Part 5: Adult Basic Life Support and Cardiopulmonary Resuscitation Quality: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 132, S414–S435 (2015).
Atkins, D. L. et al. Part 11: Pediatric Basic Life Support and Cardiopulmonary Resuscitation Quality: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 132, S519–S525 (2015).
Kern, K. B., Hilwig, R. W., Berg, R. A., Sanders, A. B. & Ewy, G. A. Importance of continuous chest compressions during cardiopulmonary resuscitation: improved outcome during a simulated single lay-rescuer scenario. Circulation 105, 645–649 (2002).
Ewy, G. A. et al. Improved neurological outcome with continuous chest compressions compared with 30:2 compressions-to-ventilations cardiopulmonary resuscitation in a realistic swine model of out-of-hospital cardiac arrest. Circulation 116, 2525–2530 (2007).
Xanthos, T. et al. Continuous chest compressions improve survival and neurologic outcome in a swine model of prolonged ventricular fibrillation. Am. J. Emerg. Med. 30, 1389–1394 (2012).
Berg, R. A. et al. Adverse hemodynamic effects of interrupting chest compressions for rescue breathing during cardiopulmonary resuscitation for ventricular fibrillation cardiac arrest. Circulation 104, 2465–2470 (2001).
Bobrow, B. J. et al. Chest compression-only CPR by lay rescuers and survival from out-of-hospital cardiac arrest. JAMA 304, 1447–1454 (2010).
Kitamura, T. et al. Conventional and chest-compression-only cardiopulmonary resuscitation by bystanders for children who have out-of-hospital cardiac arrests: a prospective, nationwide, population-based cohort study. Lancet 375, 1347–1354 (2010).
Rea, T. D. et al. CPR with chest compression alone or with rescue breathing. N. Engl. J. Med. 363, 423–433 (2010).
Nichol, G. et al. Trial of continuous or interrupted chest compressions during CPR. N. Engl. J. Med. 373, 2203–2214 (2015).
Vali, P. et al. Hemodynamics and gas exchange during chest compressions in neonatal resuscitation. PLoS ONE 12, e0176478 (2017).
Berg, R. A., Hilwig, R. W., Kern, K. B., Babar, I. & Ewy, G. A. Simulated mouth-to-mouth ventilation and chest compressions (bystander cardiopulmonary resuscitation) improves outcome in a swine model of prehospital pediatric asphyxial cardiac arrest. Crit. Care Med. 27, 1893–1899 (1999).
Berg, R. A., Hilwig, R. W., Kern, K. B. & Ewy, G. A. “Bystander” chest compressions and assisted ventilation independently improve outcome from piglet asphyxial pulseless “cardiac arrest”. Circulation 101, 1743–1748 (2000).
Barber, C. A. & Wyckoff, M. Neonatal cardiac compressions following asystole from asphyxia: beneficial or futile? [Abstract 7932.7]. In Pediatric Academic Societies Meeting, Toronto, Canada (2007).
Solevåg, A. L., Dannevig, I., Wyckoff, M., Saugstad, O. D. & Nakstad, B. Extended series of cardiac compressions during CPR in a swine model of perinatal asphyxia. Resuscitation 81, 1571–1576 (2010).
Solevag, A. L., Dannevig, I., Wyckoff, M., Saugstad, O. D. & Nakstad, B. Return of spontaneous circulation with a compression:ventilation ratio of 15:2 versus 3:1 in newborn pigs with cardiac arrest due to asphyxia. Arch. Dis. Child Fetal Neonatal Ed. 96, F417–F421 (2011).
Hemway, R. J., Christman, C. & Perlman, J. The 3:1 is superior to a 15:2 ratio in a newborn manikin model in terms of quality of chest compressions and number of ventilations. Arch. Dis. Child Fetal Neonatal Ed. 98, F42–F45 (2013).
Schmölzer, G. M. et al. 3:1 compression to ventilation ratio versus continuous chest compression with asynchronous ventilation in a porcine model of neonatal resuscitation. Resuscitation 85, 270–275 (2014).
Solevåg, A. L. & Schmölzer, G. M. Optimal chest compression rate and compression to ventilation ratio in delivery room resuscitation: evidence from newborn piglets and neonatal manikins. Front. Pediatr. 5, 3 (2017).
Solevåg, A. L. et al. Chest compressions in newborn animal models: a review. Resuscitation 96, 151–155 (2015).
Wyckoff, M. H. & Berg, R. A. Optimizing chest compressions during delivery-room resuscitation. Semin. Fetal Neonatal Med. 13, 410–415 (2008).
Kilkenny, C., Browne, W. J., Cuthill, I. C., Emerson, M. & Altman, D. G. Improving Bioscience Research Reporting: the ARRIVE Guidelines for Reporting Animal Research. PLoS Biol. 8, e1000412 (2010).
Vali, P. et al. Evaluation of timing and route of epinephrine in a neonatal model of asphyxial arrest. J. Am. Heart Assoc. 6, 2 (2017).
Wyckoff, M. H. et al. Part 13: Neonatal Resuscitation: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 132, S543–S560 (2015).
McKinsey, S. & Perlman, J. M. Resuscitative interventions during simulated asystole deviate from the recommended timeline. Arch. Dis. Child Fetal Neonatal Ed. 101, F244–F247 (2016).
Halling, C., Sparks, J. E., Christie, L. & Wyckoff, M. H. Efficacy of intravenous and endotracheal epinephrine during neonatal cardiopulmonary resuscitation in the delivery room. J. Pediatr. 185, 232–236 (2017).
Vali, P. et al. The perinatal asphyxiated lamb model: a model for newborn resuscitation. J. Vis. Exp. 138, 57553 (2018).
Paradis, N. A. et al. Coronary perfusion pressure and the return of spontaneous circulation in human cardiopulmonary resuscitation. JAMA 263, 1106–1113 (1990).
Moraga, F., Monge, C., Riquelme, R. & Llanos, A. J. Fetal and maternal blood oxygen affinity: a comparative study in llamas and sheep. Comp. Biochem. Physiol. A 115, 111–115 (1996).
Babbs, C. F., Meyer, A. & Nadkarni, V. Neonatal CPR: room at the top-a mathematical study of optimal chest compression frequency versus body size. Resuscitation 80, 1280–1284 (2009).
Dawes, G. S., Mott, J. C. & Shelley, H. J. The importance of cardiac glycogen for the maintenance of life in foetal lambs and newborn animals during anoxia. J. Physiol. 146, 516–538 (1959).
Vali, P. et al. Continuous chest compressions during sustained inflations in a perinatal asphyxial cardiac arrest lamb model. Pediatr. Crit. Care Med. 18, e370–e377 (2017).
Acknowledgements
The work has been supported by NIH grants HD096299 (P.V.) and HD072929 (S.L.).
Author information
Authors and Affiliations
Contributions
P.V. made substantial contributions to conception and design, acquisition, analysis and interpretation of data. and drafting the manuscript. A.L., M.H., Z.A., P.C., H.J., and D.S. made substantial contributions to data acquisition and extraction. All authors critically revised and approve the final version for publication.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Vali, P., Lesneski, A., Hardie, M. et al. Continuous chest compressions with asynchronous ventilations increase carotid blood flow in the perinatal asphyxiated lamb model. Pediatr Res 90, 752–758 (2021). https://doi.org/10.1038/s41390-020-01306-4
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-020-01306-4
This article is cited by
-
Cardiopulmonary resuscitation with 3:1 Compression:Ventilation or continuous compression with asynchronized ventilation in infantile piglets
Pediatric Research (2024)
-
Neonatal resuscitation with continuous chest compressions and high frequency percussive ventilation in preterm lambs
Pediatric Research (2024)
-
Laryngeal mask ventilation with chest compression during neonatal resuscitation: randomized, non-inferiority trial in lambs
Pediatric Research (2022)
-
Neonatal chest compressions: time to act
Pediatric Research (2021)