Abstract
Background
Volatile organic compounds (VOCs) are hydrocarbons that originate within different healthy and diseased tissues. VOCs can be secreted into the circulation and then excreted in the urine and faeces. In the lungs, VOCs are locally produced and can be detected in exhaled breath. VOCs can be identified using non-invasive techniques, which make their use in preterm infants safe and desirable.
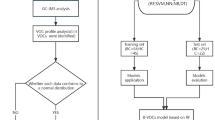
Methods
A systematic search of the literature in PubMed, Embase and Web of Science was conducted looking for VOCs techniques and diagnostic performance in preterm infants. A total of 50 articles identified with only seven papers were included in the final analysis in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).
Results
VOCs could diagnose necrotising enterocolitis up to 4 days before a clinical diagnosis; for late onset sepsis, up to 3 days before; and for bronchopulmonary dysplasia, up to 2 weeks before. In addition to these diagnostic uses, VOCs analysis could also distinguish breastfed from formula-fed preterm neonates in the first month of life.
Conclusion
VOCs analysis is a non-invasive tool that makes the use in preterm infants of preference. VOCs analytic techniques require more research and consensus between researchers to overcome their limitations.
Impact
-
Volatile organic compounds are hydrocarbons that can separate between healthy and diseased states in preterm infants.
-
Biomarker panels developed from volatile organic compounds are potential diagnostic tools.
-
The non-invasive nature of acquiring volatile organic compounds markers make it desirable in the paediatric patients.
-
Research into exact chemical components of the volatile organic compounds can inform about the pathophysiology of disease in preterm infants.
-
More robust longitudinal studies with repeated experiments are required before volatile organic compounds can be applied in clinical practice.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Shirasu, M. & Touhara, K. The scent of disease: volatile organic compounds of the human body related to disease and disorder. J. Biochem. 150, 257–266 (2011).
Padua, A. C., Palma, S., Gruber, J., Gamboa, H. & Roque, A. C. Design and evolution of an opto-electronic device for VOCs detection. Biomed. Eng. Syst. Technol. Int. Jt. Conf. BIOSTEC Revis. Sel. Pap. 1, 48–55 (2018).
Arasaradnam, R. P. et al. Non-invasive exhaled volatile organic biomarker analysis to detect inflammatory bowel disease (IBD). Dig. Liver Dis. 48, 148–153 (2016).
Sun, X., Shao, K. & Wang, T. Detection of volatile organic compounds (VOCs) from exhaled breath as noninvasive methods for cancer diagnosis. Anal. Bioanal. Chem. 408, 2759–2780 (2016).
Zetola, N. M. et al. Diagnosis of pulmonary tuberculosis and assessment of treatment response through analyses of volatile compound patterns in exhaled breath samples. J. Infect. 74, 367–376 (2017).
Buijck, M. et al. Sniffing out paediatric gastrointestinal diseases: the potential of volatile organic compounds as biomarkers for disease. J. Pediatr. Gastroenterol. Nutr. 63, 585–591 (2016).
Bannier, M., van de Kant, K. D. G., Jobsis, Q. & Dompeling, E. Feasibility and diagnostic accuracy of an electronic nose in children with asthma and cystic fibrosis. J. Breath Res. 13, 036009 (2018).
Tauchi, H. et al. Gut microbiota development of preterm infants hospitalised in intensive care units. Benef. Microbes 9, 1–12 (2019).
Fleischmann-Struzek, C. et al. The global burden of paediatric and neonatal sepsis: a systematic review. Lancet Respir. Med. 6, 223–230 (2018).
Walsh, E. M., Li, S. X., Black, L. K. & Kuzniewicz, M. Incremental cost of prematurity by week of gestational age. AJP Rep. 9, 76–83 (2019).
Fitzgibbons, S. C. et al. Mortality of necrotizing enterocolitis expressed by birth weight categories. J. Pediatr. Surg. 44, 1072–1075 (2009).
Chiesa, C., Panero, A., Osborn, J. F., Simonetti, A. F. & Pacifico, L. Diagnosis of neonatal sepsis: a clinical and laboratory challenge. Clin. Chem. 50, 279–287 (2004).
Beltempo, M. et al. C-reactive protein for late-onset sepsis diagnosis in very low birth weight infants. BMC Pediatr. 18, 1–8 (2018).
Neu, J. & Walker, W. A. Necrotizing enterocolitis. N. Engl. J. Med. 364, 255–264 (2011).
Jobe, A. H. & Bancalari, E. Bronchopulmonary dysplasia. Am. J. Respir. Crit. Care Med. 163, 1723–1729 (2001).
Berkhout, D. J. C. et al. Detection of sepsis in preterm infants by fecal volatile organic compounds analysis: a proof of principle study. J. Pediatr. Gastroenterol. Nutr. 65, e47–e52 (2017).
Berkhout, D. J. C. et al. Late-onset sepsis in preterm infants can be detected preclinically by fecal volatile organic compound analysis: a prospective, multicenter cohort study. Clin. Infect. Dis. 68, 70–77 (2019).
de Meij, T. G. J. et al. Early detection of necrotizing enterocolitis by fecal volatile organic compounds analysis. J. Pediatrics. 167, 562–567 (2015).
Garner, C. E. et al. Analysis of faecal volatile organic compounds in preterm infants who develop necrotising enterocolitis: a pilot study. J. Pediatr. Gastroenterol. Nutr. 49, 559–565 (2009).
Probert, C. et al. Faecal volatile organic compounds in preterm babies at risk of necrotising enterocolitis: the DOVE study. Arch. Dis. Child. Fetal Neonatal Ed. Dec 23 (2019). [Epub ahead of print].
Berkhout, D. J. C. et al. Development of severe bronchopulmonary dysplasia is associated with alterations in fecal volatile organic compounds. Pediatr. Res. 83, 412–419 (2018).
Kononikhin, A. S. et al. Exhaled breath condensate analysis from intubated newborns by nano-HPLC coupled to high resolution MS. J. Chromatogr. B-Anal. Technol. Biomed. Life Sci. 1047, 97–105 (2017).
Embleton, N. D. et al. Mechanisms affecting the gut of preterm infants in enteral feeding trials. Front. Nutr. 4, 1–13 (2017).
Park, J. H., Chang, Y. S., Sung, S. & Park, W. S. Mortality rate-dependent variations in the timing and causes of death in extremely preterm infants born at 23–24 weeks’ gestation. Pediatr. Crit. Care Med. 20, 630–637 (2019).
Vinall, J. & Grunau, R. E. Impact of repeated procedural pain-related stress in infants born very preterm. Pediatr. Res. 75, 584–587 (2014).
Deeg, K. H. Sonographic and Doppler sonographic diagnosis of necrotizing enterocolitis in preterm infants and newborns. Ultraschall. Med. 40, 292–318 (2019).
Sankarganesh, D. et al. Urinary volatile metabolomics as a viable alternative diagnostic tool for polycystic ovary syndrome: an exploratory hypothesis. Med. Hypotheses 124, 121–124 (2019).
van de Goor, R., Hardy, J. C. A., van Hooren, M. R. A., Kremer, B. & Kross, K. W. Detecting recurrent head and neck cancer using electronic nose technology: a feasibility study. Head Neck 41, 2983–2990 (2019).
Behera, B., Joshi, R., Anil Vishnu, G. K., Bhalerao, S. & Pandya, H. J. Electronic nose: a non-invasive technology for breath analysis of diabetes and lung cancer patients. J. Breath Res. 13, 024001 (2019).
Harrison, C. M. & Andersen, C. C. Exhaled breath measures of inflammation: are they useful in neonatal chronic lung disease. Arch. Dis. Child. Fetal Neonatal Ed. 90, 6–10 (2005).
Sahota, A. S. et al. A simple breath test for tuberculosis using ion mobility: a pilot study. Tuberculosis (Edinburgh) 99, 143–146 (2016).
Steinbach, J. et al. Bedside measurement of volatile organic compounds in the atmosphere of neonatal incubators using ion mobility spectrometry. Front. Pediatrics 7, 1–7 (2019).
Liu, D. et al. Urine volatile organic compounds as biomarkers for minimal change type nephrotic syndrome. Biochem. Biophys. Res. Commun. 496, 58–63 (2018).
Wang, M., Xie, R., Jia, X. & Liu, R. Urinary volatile organic compounds as potential biomarkers in idiopathic membranous nephropathy. Med. Princ. Pract. 26, 375–380 (2017).
Arasaradnam, R. P. et al. Non-invasive distinction of non-alcoholic fatty liver disease using urinary volatile organic compound analysis: early results. J. Gastrointestin Liver Dis. 24, 197–201 (2015).
Arasaradnam, R. P. et al. Noninvasive diagnosis of pancreatic cancer through detection of volatile organic compounds in urine. Gastroenterology 154, 485–487 (2018).
Widlak, M. M. et al. Risk stratification of symptomatic patients suspected of colorectal cancer using faecal and urinary markers. Colorectal Dis. 20, 335–342 (2018).
Arasaradnam, R. P. et al. Detection of colorectal cancer (CRC) by urinary volatile organic compound analysis. PLoS ONE 9, 1–9 (2014).
El-Metwally, D. et al. Urinary metabolites of volatile organic compounds of infants in the neonatal intensive care unit. Pediatr. Res. 83, 1158–1164 (2018).
El Manouni El Hassani, S. et al. Fecal volatile organic compounds in preterm infants are influenced by enteral feeding composition. Sensors (Basel) 18, 1–13 (2018).
Author information
Authors and Affiliations
Contributions
H.W. collected and analysed the data and participated in the final manuscript. A.S.B., R.I. and M.M. contributed to all aspects of the final manuscript for analysis and intellectual input. R.P. A. designed the study and supervised the project.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wright, H., Bannaga, A.S., Iriarte, R. et al. Utility of volatile organic compounds as a diagnostic tool in preterm infants. Pediatr Res 89, 263–268 (2021). https://doi.org/10.1038/s41390-020-0828-3
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-020-0828-3
This article is cited by
-
Cyclohexanone and metabolites exposure in critically Ill neonates and children
Pediatric Research (2025)
-
Longitudinal fecal microbiota and volatile metabolomics preceding necrotizing enterocolitis in preterm infants: a case–control study
Scientific Reports (2025)