Abstract
Background
To assess the overall prevalence of clinical signs, symptoms, and radiological findings in children and/or adolescents with COVID-19.
Methods
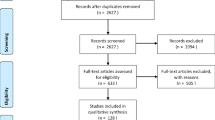
We systematically researched in PubMed, Scopus and Web of Science databases observational studies describing COVID-19 in children and/or adolescents until April 11, 2020. Data regarding clinical and radiological features were extracted from eligible studies and meta-analysis was performed using random-effects modeling.
Results
We examined 19 eligible studies for a total of 2855 children and/or adolescents with COVID-19. Approximately 47% of subjects had fever (95% confidence interval [CI] 22−72%; I2 = 98.6%), 37% cough (95%CI 15−63%; I2 = 98.6%), 4% diarrhea (95%CI 0−12%; I2 = 92.2%), 2% nasal congestion (95%CI 0−7%; I2 = 87.7%), 1% dyspnea (95%CI 0−7%; I2 = 91.5%) and 0% abdominal pain (95%CI 0−1%; I2 = 76.3%). Subjects presented mild symptoms in 79% (95%CI 65−91%; I2 = 93.5%) of cases, whereas only 4% (95%CI 1−9%; I2 = 76.4%) were critical. Among those with pneumonia on computed tomography, 26.4% (95%CI 13−41%; I2 = 80.8%) presented a unilateral involvement, 16% (95%CI 5−29%, I2 = 81.2%) had bilateral involvement and 9% (95%CI 0−24%; I2 = 88.7%) had interstitial pneumonia.
Conclusions
Children and/or adolescents tend to have a mild COVID-19 course with a good prognosis.
Impact
-
Compared to adults, children and/or adolescents tend to have a mild COVID-19 course with a good prognosis.
-
This study provides new and consistence information on the clinical and radiological characteristics of COVID-19 in pediatrics.
-
This study may help to fight COVID-19 in pediatric population.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
World Health Organization. Coronavirus disease 2019. https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (2020).
Cruz, A. & Zeichner, S. COVID-19 in children: initial characterization of the pediatric disease. Pediatrics https://doi.org/10.1542/peds.2020-0834 (2020).
Rothan, H. A. & Byrareddy, S. N. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J. Autoimmun. https://doi.org/10.1016/j.jaut.2020.102433 (2020).
Stroup, D. F. et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 283, 2008–2012 (2000).
Higgins, J. P. T. & Green, S. (eds). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (The Cochrane Collaboration, 2011).
Newcombe, R. G. Two-sided confidence intervals for the single proportion: comparison of seven methods. Stat. Med. 17, 857–872 (1998).
Nyaga, V. N., Arbyn, M. & Aerts, M. Metaprop: a STATA command to perform meta-analysis of binomial data. Arch. Public Health 72, 39 (2014).
Higgins, J. P. & Thompson, S. G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 21, 1539–1558 (2002).
Egger, M., Smith, G. D. & Phillips, A. N. Meta-analysis: principles and procedures. BMJ 315, 1533–1537 (1997).
Zheng, F., et al. Clinical characteristics of children with coronavirus disease 2019 in Hubei, China. Curr. Med. Sci. https://doi.org/10.1007/s11596-020-2172-6 (2020).
Sun, D. et al. Clinical features of severe pediatric patients with coronavirus disease 2019 in Wuhan: a single center’s observational study. World J. Pediatr. https://doi.org/10.1007/s12519-020-00354-4 (2020).
Lu, X. et al. SARS-CoV-2 infection in children. N. Engl. J. Med. https://doi.org/10.1056/NEJMc2005073 (2020).
Liu, H. et al. Clinical and CT imaging features of the COVID-19 pneumonia: focus on pregnant women and children. J. Infect. https://doi.org/10.1016/j.jinf.2020.03.007 (2020).
Liu, W. et al. Detection of Covid-19 in children in early January 2020 in Wuhan, China. N. Engl. J. Med. 382, 1370–1371 (2020).
Xia, W. et al. Clinical and CT features in pediatric patients with COVID-19 infection: different points from adults. Pediatr. Pulmonol. https://doi.org/10.1002/ppul.24718 (2020).
Cai, J. et al. A case series of children with 2019 novel coronavirus infection: clinical and epidemiological features. Clin. Infect. Dis. https://doi.org/10.1093/cid/ciaa198 (2020).
Dong, Y. et al. Epidemiological characteristics of 2143 pediatric patients with 2019 coronavirus disease in China. Pediatrics https://doi.org/10.1542/peds.2020-0702 (2020).
Liu, M., Song, Z. & Xiao, K. High-resolution computed tomography manifestations of 5 pediatric patients with 2019 novel coronavirus. J. Comput. Assist. Tomogr. https://doi.org/10.1097/RCT.0000000000001023 (2020).
Wei, M. et al. Novel coronavirus infection in hospitalized infants under 1 year of age in China. JAMA https://doi.org/10.1001/jama.2020.2131 (2020).
Su, L. et al. The different clinical characteristics of corona virus disease cases between children and their families in China—the character of children with COVID-19. Emerg. Microbes Infect. 9, 707–713 (2020).
Zhou, Y. et al. Clinical features and chest CT findings of coronavirus disease 2019 in infants and young children. Zhongguo Dang Dai Er Ke Za Zhi 22, 215–220 (2020).
Qiu, H. et al. Clinical and epidemiological features of 36 children with coronavirus disease 2019 (COVID-19) in Zhejiang, China: an observational cohort study. Lancet Infect. Dis. https://doi.org/10.1016/S1473-3099(20)30198-5 (2020).
Shen, Q. et al. Novel coronavirus infection in children outside of Wuhan, China. Pediatr. Pulmonol. https://doi.org/10.1002/ppul.24762 (2020).
Zhu, L. et al. Clinical characteristics of a case series of children with coronavirus disease 2019. Pediatr. Pulmonol. https://doi.org/10.1002/ppul.24767 (2020).
C. D. C. COVID-19 Response Team. Coronavirus disease 2019 in children—United States, February 12−April 2, 2020. MMWR Morb. Mortal. Wkly. Rep. 69, 422–426 (2020).
Tagarro, A. et al. Screening and severity of coronavirus disease 2019 (COVID-19) in children in Madrid, Spain. JAMA Pediatr. https://doi.org/10.1001/jamapediatrics.2020.1346 (2020).
Feng, K. et al. Analysis of CT features of 15 Children with 2019 novel coronavirus infection. Zhonghua Er Ke Za Zhi 58, E007 (2020).
Wang, D. et al. Clinical analysis of 31 cases of 2019 novel coronavirus infection in children from six provinces (autonomous region) of northern China. Zhonghua Er Ke Za Zhi 58, E011 (2020).
Duval, S. & Tweedie, R. A nonparametric “trim and fill” method of accounting for publication bias in meta-analysis. J. Am. Stat. Assoc. 95, 89–98 (2000).
Ludvigsson, J. F. Systematic review of COVID‐19 in children shows milder cases and a better prognosis than adults. Acta Paediatr. https://doi.org/10.1111/apa.15270 (2020).
Castagnoli, R. et al. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in children and adolescents: a systematic review. JAMA Pediatr. https://doi.org/10.1001/jamapediatrics.2020.1467 (2020).
Wu, Z. & McGoogan J. M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA https://doi.org/10.1001/jama.2020.2648 (2020).
KCDC. Updates on COVID-19 in Korea. https://www.cdc.go.kr/board/board.es?mid=a30402000000&bid=0030 (2020).
Wrapp, D. et al. Cryo-EM structure of the 2019-nCoV spike in the prefusion conformation. Science 367, 1260–1263 (2020).
Simon, A. K., Hollander, G. A. & McMichael, A. Evolution of the immune system in humans from infancy to old age. Proc. Biol. Sci. 282, 20143085 (2015).
Henry, B. M., Lippi, G. & Plebani, M. Laboratory abnormalities in children with novel coronavirus disease 2019. Clin. Chem. Lab. Med. https://doi.org/10.1515/cclm-2020-0272 (2020).
https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/children/mis-c.html (2020).
Author information
Authors and Affiliations
Contributions
A.M. and A.D. conceptualized and designed the study, carried out the initial analyses, drafted the initial manuscript, and reviewed and revised the manuscript. E.R., C.Z., G.B. and M.D.S. designed the data collection instruments, collected data, and reviewed and revised the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Mantovani, A., Rinaldi, E., Zusi, C. et al. Coronavirus disease 2019 (COVID-19) in children and/or adolescents: a meta-analysis. Pediatr Res 89, 733–737 (2021). https://doi.org/10.1038/s41390-020-1015-2
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-020-1015-2
This article is cited by
-
Health-related quality of life, glycaemic control, lifestyle characteristics and SARS-CoV-2 prevalence in children with type 1 diabetes during the COVID-19 pandemic: results of a longitudinal, prospective single-centre Swiss study
BMC Pediatrics (2026)
-
Threat of coronavirus and depressive symptoms in adolescents: do 24-hour movement behaviors mediate this relationship?
BMC Public Health (2025)
-
Epidemic profile of COVID-19 child deaths in Sri Lanka: a retrospective nationwide analysis
BMC Pediatrics (2025)
-
An exploration of COVID-19 impact on physical capacity, self-reported outcomes, and mental health in late adolescents
Current Psychology (2025)
-
Evidence linking COVID-19 and the health/well-being of children and adolescents: an umbrella review
BMC Medicine (2024)