Abstract
Background
The aim of the study was to describe and contrast the brain development and outcome among very preterm infants that were and were not exposed to surgery requiring general anesthesia prior to term equivalent age (TEA).
Methods
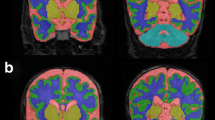
Preterm infants born ≤30 weeks’ gestation who did (n = 25) and did not (n = 59) have surgery requiring general anesthesia during the preterm period were studied. At TEA, infants had MRI scans performed with measures of brain tissue volumes, cortical surface area, Gyrification Index, and white matter microstructure. Neurodevelopmental follow-up with the Bayley Scales of Infant and Toddler Development, Third Edition was undertaken at 2 years of corrected age. Multivariate models, adjusted for clinical and social risk factors, were used to compare the groups.
Results
After controlling for clinical and social variables, preterm infants exposed to surgical anesthesia demonstrated decreased relative white matter volumes at TEA and lower cognitive and motor composite scores at 2-year follow-up. Those with longer surgical exposure demonstrated the greatest decrease in white matter volumes and lower cognitive and motor outcomes at age 2 years.
Conclusions
Very preterm infants who required surgery during the preterm period had lower white mater volumes at TEA and worse neurodevelopmental outcome at age 2 years.
Impact
-
In very preterm infants, there is an association between surgery requiring general anesthesia during the preterm period and reduced white mater volume on MRI at TEA and lower cognitive and motor composite scores at age 2 years.
-
It is known that the very preterm infant’s brain undergoes rapid growth during the period corresponding to the third trimester.
-
The current study suggests an association between surgery requiring general anesthesia during this period and worse outcomes.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Wilder, R. T. et al. Early exposure to anesthesia and learning disabilities in a population-based birth cohort. Anesthesiology 110, 796–804 (2009).
Flick, R. P. et al. Cognitive and behavioral outcomes after early exposure to anesthesia and surgery. Pediatrics 128, e1053–e1061 (2011).
Moran, M. M. et al. Associations of neonatal noncardiac surgery with brain structure and neurodevelopment: a prospective case-control study. J. Pediatr. 212, 93.e2–101.e2 (2019).
Sanders, R. D., Hassell, J., Davidson, A. J., Robertson, N. J. & Ma, D. Impact of anaesthetics and surgery on neurodevelopment: an update. Br. J. Anaesth. 110, i53–i72 (2013).
Brambrink, A. M. et al. Isoflurane-induced apoptosis of oligodendrocytes in the neonatal primate brain. Ann. Neurol. 72, 525–535 (2012).
Sun, L. S. et al. Association between a single general anesthesia exposure before age 36 months and neurocognitive outcomes in later childhood. JAMA 315, 2312–2320 (2016).
Davidson, A. J. et al. Neurodevelopmental outcome at 2 years of age after general anaesthesia and awake-regional anaesthesia in infancy (GAS): an international multicentre, randomised controlled trial. Lancet 387, 239–250 (2016).
Rizzi, S., Ori, C. & Jevtovic-Todorovic, V. Timing versus duration: determinants of anesthesia-induced developmental apoptosis in the young mammalian brain. Ann. NY Acad. Sci. 1199, 43–51 (2010).
Andescavage, N. N. et al. Complex trajectories of brain development in the healthy human fetus. Cereb. Cortex 27, 5274–5283 (2017).
Filan, P. M., Hunt, R. W., Anderson, P. J., Doyle, L. W. & Inder, T. E. Neurologic outcomes in very preterm infants undergoing surgery. J. Pediatr. 160, 409–414 (2012).
Morriss, F. H. Jr et al. Surgery and neurodevelopmental outcome of very low-birth-weight infants. JAMA Pediatr. 168, 746–754 (2014).
Stolwijk, L. J. et al. Neonatal surgery for noncardiac congenital anomalies: neonates at risk of brain injury. J. Pediatr. 182, 335.e1–341.e1 (2017).
Mathur, A. M., Neil, J. J., McKinstry, R. C. & Inder, T. E. Transport, monitoring, and successful brain MR imaging in unsedated neonates. Pediatr. Radiol. 38, 260–264 (2008).
Kidokoro, H., Neil, J. J. & Inder, T. E. New MR imaging assessment tool to define brain abnormalities in very preterm infants at term. AJNR Am. J. Neuroradiol. 34, 2208–2214 (2013).
Klein, A. et al. Evaluation of volume-based and surface-based brain image registration methods. Neuroimage 51, 214–220 (2010).
Van Essen, D. C. et al. An integrated software suite for surface-based analyses of cerebral cortex. J. Am. Med Inf. Assoc. 8, 443–459 (2001).
Hill, J. et al. A surface-based analysis of hemispheric asymmetries and folding of cerebral cortex in term-born human infants. J. Neurosci. 30, 2268–2276 (2010).
Smith, S. M. et al. Tract-based spatial statistics: voxelwise analysis of multi-subject diffusion data. Neuroimage 3, 1487–1505 (2006).
Lean, R. E., Paul, R. A., Smyser, C. D. & Rogers, C. E. Maternal intelligence quotient (IQ) predicts IQ and language in very preterm children at age 5 years. J. Child Psychol. Psychiatry 59, 150–159 (2018).
Lean, R. E., Paul, R. A., Smyser, T. A., Smyser, C. D. & Rogers, C. E. Social adversity and cognitive, language, and motor development of very preterm children from 2 to 5 years of age. J. Pediatr. 203, 177.e1–184.e1 (2018).
Lean, R. E. et al. Maternal and family factors differentiate profiles of psychiatric impairments in very preterm children at age 5-years. J. Child Psychol. Psychiatry 6, 157–166 (2020).
Matthews, L. G. et al. Brain growth in the NICU: critical periods of tissue-specific expansion. Pediatr. Res. 83, 976–981 (2018).
Makaryus, R. et al. Brain maturation in neonatal rodents is impeded by sevoflurane anesthesia. Anesthesiology 123, 557–568 (2015).
Broad, K. D. et al. Isoflurane exposure induces cell death, microglial activation and modifies the expression of genes supporting neurodevelopment and cognitive function in the male newborn piglet brain. PLoS ONE 11, e0166784 (2016).
Jevtovic-Todorovic, V. et al. Early exposure to common anesthetic agents causes widespread neurodegeneration in the developing rat brain and persistent learning deficits. J. Neurosci. 23, 876–882 (2003).
Fredriksson, A., Pontén, E., Gordh, T. & Eriksson, P. Neonatal exposure to a combination of N-methyl-D-aspartate and gamma-aminobutyric acid type A receptor anesthetic agents potentiates apoptotic neurodegeneration and persistent behavioral deficits. Anesthesiology 107, 427–436 (2007).
Stratmann, G. et al. Isoflurane differentially affects neurogenesis and long-term neurocognitive function in 60-day-old and 7-day-old rats. Anesthesiology 110, 834–848 (2009).
Deng, M. et al. Brain regional vulnerability to anaesthesia-induced neuroapoptosis shifts with age at exposure and extends into adulthood for some regions. Br. J. Anaesth. 113, 443–451 (2014).
Ing, C. et al. Latent class analysis of neurodevelopmental deficit after exposure to anesthesia in early childhood. J. Neurosurg. Anesthesiol. 29, 264–273 (2017).
Dammann, O. & Leviton, A. Maternal intrauterine infection, cytokines, and brain damage in the preterm newborn. Pediatr. Res 42, 1–8 (1997).
Lodygensky, G. A. et al. In vivo MRI analysis of an inflammatory injury in the developing brain. Brain Behav. Immun. 24, 759–767 (2010).
Volpe, J. J. Brain injury in premature infants: a complex amalgam of destructive and developmental disturbances. Lancet Neurol. 8, 110–124 (2009).
Gano, D. et al. Impaired cognitive performance in premature newborns with two or more surgeries prior to term-equivalent age. Pediatr. Res. 78, 323–329 (2015).
Xu, G. et al. Late development of the GABAergic system in the human cerebral cortex and white matter. J. Neuropathol. Exp. Neurol. 70, 841–858 (2011).
Moeskops, P. et al. Development of cortical morphology evaluated with longitudinal MR brain images of preterm infants. PLoS ONE 10, e0131552 (2015).
Sinha, S. K. and Neogi, S. Bedside neonatal intensive care unit surgery - myth or reality! J. Neonatal Surg. 2, 20 (2013).
Zwicker, J. G. et al. Smaller cerebellar growth and poorer neurodevelopmental outcomes in very preterm infants exposed to neonatal morphine. J. Pediatr. 172, 81.e2–87.e2 (2016).
McPherson, C. et al. Brain injury and development in preterm infants exposed to fentanyl. Ann. Pharmacother. 49, 1291–1297 (2015).
Acknowledgements
We thank Dr. Regina Triplett for her assistance in qualitative interpretation of the MR images. This work was supported by the Eunice Kennedy Shriver National Institute Of Child Health & Human Development with Awards U54 HD087011 (Intellectual and Developmental Disabilities Research Center at Washington University (to J.S.S.)) and R01 HD 057098 (original WUNDER cohort grant): K02 NS089852 and UL1 TR000448.
Author information
Authors and Affiliations
Contributions
Substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; drafting the article or revising it critically for important intellectual content; and final approval of the version to be published: all authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent
The study was approved by the Washington University Human Research Protection Office. Parental informed consent was obtained for each subject prior to enrollment.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Walsh, B.H., Paul, R.A., Inder, T.E. et al. Surgery requiring general anesthesia in preterm infants is associated with altered brain volumes at term equivalent age and neurodevelopmental impairment. Pediatr Res 89, 1200–1207 (2021). https://doi.org/10.1038/s41390-020-1030-3
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-020-1030-3
This article is cited by
-
Rutin ameliorates sevoflurane-induced neurotoxicity by inhibiting microglial synaptic phagocytosis through the complement pathway
Scientific Reports (2025)
-
Evaluation of timed dexamethasone eye drops to prevent proliferative retinopathy of prematurity: a study protocol for a randomized intervention, multi-centre, double-blinded trial (DROPROP)
BMC Pediatrics (2025)
-
Complement C1q-mediated microglial synaptic elimination by enhancing desialylation underlies sevoflurane-induced developmental neurotoxicity
Cell & Bioscience (2024)
-
Morbidity and neurodevelopmental outcomes at 2 years in preterm infants undergoing percutaneous transcatheter closure vs. surgical ligation of the PDA
Journal of Perinatology (2024)
-
Early surgery in very preterm infants is associated with brain abnormalities on term MRI: a propensity score analysis
Journal of Perinatology (2023)