Abstract
Background
Exposure to diabetes in utero influences future metabolic health of the offspring. MicroRNAs (miRNA) are small noncoding RNAs that may contribute mechanistically to the effects on offspring imparted by diabetes mellitus (DM) during pregnancy. We hypothesized that exposure to DM during pregnancy influences select miRNAs in fetal circulation, in human umbilical vein endothelial cells (HUVEC), and placenta.
Methods
miRNA abundance was quantified using real-time PCR from RNA isolated from umbilical cord serum exosomes, HUVEC, and placenta exposed to diabetes or normoglycemia during pregnancy. The abundance of each of these miRNAs was determined by comparison to a known standard and the relative expression assessed using the 2−ΔΔCt method. Multivariable regression models examined the associations between exposure to diabetes during pregnancy and miRNA expression.
Results
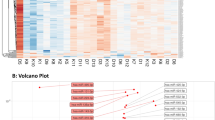
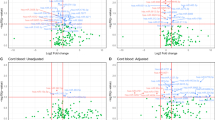
miR-126-3p was highly abundant in fetal circulation, HUVEC, and placenta. Diabetes exposure during pregnancy resulted in lower expression of miR-148a-3p and miR-29a-3p in the HUVEC. In the placenta, for miR-126-3p, there was a differential effect of DM by birth weight between DM versus control group, expression being lower at the lower birth weight, however not different at the higher birth weight.
Conclusion
Exposure to DM during pregnancy alters miRNA expression in the offspring in a tissue-specific manner.
Impact
-
miRNAs are differentially expressed in fetal tissues from offspring exposed to in utero diabetes mellitus compared to those who were not exposed.
-
miRNA expression differs among tissue types (human umbilical vein endothelial cells, placenta and circulation exosomes) and response to diabetes exposure varies according to tissue of origin.
-
miRNA expression is also affected by maternal and infant characteristics such as infant birth weight, infant sex, maternal age, and maternal BMI.
-
miRNAs might be one of the potential mechanisms by which offspring’s future metabolic status may be influenced by maternal diabetes mellitus.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Boney, C. M., Verma, A., Tucker, R. & Vohr, B. R. Metabolic syndrome in childhood: association with birth weight, maternal obesity, and gestational diabetes mellitus. Pediatrics 115, e290–e296 (2005).
Short, K. R. et al. Lower resting energy expenditure and fat oxidation in Native American and Hispanic infants born to mothers with diabetes. J. Pediatr. 166, 884–889 (2015).
Kappil, M. & Chen, J. Environmental exposures in utero and microRNA. Curr. Opin. Pediatr. 26, 243–251 (2014).
Chen, X. et al. Characterization of microRNAs in serum: a novel class of biomarkers for diagnosis of cancer and other diseases. Cell Res. 18, 997–1006 (2008).
Rottiers, V. & Naar, A. M. MicroRNAs in metabolism and metabolic disorders. Nat. Rev. Mol. Cell Biol. 13, 239–250 (2012).
Zampetaki, A. et al. Plasma microRNA profiling reveals loss of endothelial miR-126 and other microRNAs in type 2 diabetes. Circ. Res. 107, 810–817 (2010).
Wagschal, A. et al. Genome-wide identification of microRNAs regulating cholesterol and triglyceride homeostasis. Nat. Med. 21, 1290–1297 (2015).
He, A. et al. Overexpression of micro ribonucleic acid 29, highly up-regulated in diabetic rats, leads to insulin resistance in 3T3-L1 adipocytes. Mol. Endocrinol. 21, 2785–2794 (2007).
Mirra, P. et al. The destiny of glucose from a microRNA perspective. Front. Endocrinol. 9, 46 (2018).
Zhu, H. et al. The Lin28/let-7 axis regulates glucose metabolism. Cell 147, 81–94 (2011).
American Diabetes A. Gestational diabetes mellitus. Diabetes Care 26(Suppl 1), S103–S105 (2003).
Jaffe, E. A., Nachman, R. L., Becker, C. G. & Minick, C. R. Culture of human endothelial cells derived from umbilical veins. Identification by morphologic and immunologic criteria. J. Clin. Invest. 52, 2745–2756 (1973).
Tryggestad, J. B. et al. Influence of gestational diabetes mellitus on human umbilical vein endothelial cell miRNA. Clin. Sci. 130, 1955–1967 (2016).
Kroh, E. M., Parkin, R. K., Mitchell, P. S. & Tewari, M. Analysis of circulating microRNA biomarkers in plasma and serum using quantitative reverse transcription-PCR (qRT-PCR). Methods 50, 298–301 (2010).
Duan, Z. Y. et al. U6 can be used as a housekeeping gene for urinary sediment miRNA studies of IgA nephropathy. Sci. Rep. 8, 10875 (2018).
Bissels, U. et al. Absolute quantification of microRNAs by using a universal reference. RNA 15, 2375–2384 (2009).
Livak, K. J. & Schmittgen, T. D. Analysis of relative gene expression data using real-time quantitative PCR and the 2−ΔΔCt Method. Methods 25, 402–408 (2001).
R Core Team. R: A Language and Environment for Statistical Computing (R Foundation for Statistical Computing, Vienna, Austria, 2018).
van Buuren, S. & Groothuis-Oudshoorn, K. mice: multivariate imputation by chained equations in R. J. Stat. Softw. 45, 1–67 (2011).
Mehrotra, D. V., Li, X., Liu, J. & Lu, K. Analysis of longitudinal clinical trials with missing data using multiple imputation in conjunction with robust regression. Biometrics 68, 1250–1259 (2012).
Wang, S. et al. The endothelial-specific microRNA miR-126 governs vascular integrity and angiogenesis. Dev. Cell 15, 261–271 (2008).
de Candia, P. et al. A unique plasma microRNA profile defines type 2 diabetes progression. PLoS ONE 12, e0188980 (2017).
Mononen, N. et al. Whole blood microRNA levels associate with glycemic status and correlate with target mRNAs in pathways important to type 2 diabetes. Sci. Rep. 9, 8887 (2019).
Novikova, D. S. et al. AMP-activated protein kinase: structure, function, and role in pathological processes. Biochemistry 80, 127–144 (2015).
Kong, L. et al. Significance of serum microRNAs in pre-diabetes and newly diagnosed type 2 diabetes: a clinical study. Acta Diabetol. 48, 61–69 (2011).
Prabu, P. et al. Circulating MiRNAs of ‘Asian Indian phenotype’ identified in subjects with impaired glucose tolerance and patients with type 2 diabetes. PLoS ONE 10, e0128372 (2015).
Jiang, S. et al. Effects of maternal diabetes and fetal sex on human placenta mitochondrial biogenesis. Placenta 57, 26–32 (2017).
Jiang, S., Teague, A. M., Tryggestad, J. B. & Chernausek, S. D. Role of microRNA-130b in placental PGC-1alpha/TFAM mitochondrial biogenesis pathway. Biochem. Biophys. Res. Commun. 487, 607–612 (2017).
Tsamou, M. et al. Mother’s pre-pregnancy BMI and placental candidate miRNAs: findings from the ENVIRONAGE Birth Cohort. Sci. Rep. 7, 5548 (2017).
Lizarraga, D. et al. miRNAs differentially expressed by next-generation sequencing in cord blood buffy coat samples of boys and girls. Epigenomics 8, 1619–1635 (2016).
Ameling, S. et al. Associations of circulating plasma microRNAs with age, body mass index and sex in a population-based study. BMC Med. Genomics 8, 61 (2015).
Rodil-Garcia, P., Arellanes-Licea E. D. C., Montoya-Contreras, A. & Salazar-Olivo, L. A. Analysis of microRNA expression in newborns with differential birth weight using newborn screening cards. Int. J. Mol. Sci. 18, 2552 (2017).
Li, J. et al. The role, mechanism and potentially novel biomarker of microRNA-17-92 cluster in macrosomia. Sci. Rep. 5, 17212 (2015).
Weng, S. F. et al. Systematic review and meta-analyses of risk factors for childhood overweight identifiable during infancy. Arch. Dis. Child 97, 1019–1026 (2012).
Morisaki, S. et al. Effect of labor on plasma concentrations and postpartum clearance of cell-free, pregnancy-associated, placenta-specific microRNAs. Prenat. Diagn. 35, 44–50 (2015).
Hashimoto, K. & Koga, M. Indicators of glycemic control in patients with gestational diabetes mellitus and pregnant women with diabetes mellitus. World J. Diabetes 6, 1045–1056 (2015).
Acknowledgements
We thank our study participants. Funding was received from NIH 1K23DK106533-01A1, Endocrine Fellow Foundation Grant, Children Hospital Foundation Fellow Research Award.
Author information
Authors and Affiliations
Contributions
K.B.S. contributed to experimental design, sample analysis, data analysis, interpretation, and manuscript preparation. S.D.C. was involved in experimental design, data analysis, interpretation, and manuscript preparation. A.M.T. assisted with sample analysis, data analysis, and manuscript preparation. D.E.B. provided statistical analyses for the miRNA experiments and assisted in manuscript preparation. J.B.T. was involved in experimental design, sample analysis, data analysis, interpretation, and manuscript preparation. All authors gave their final approval of this paper for publication.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Informed consent
Consent was obtained from all participants before participation.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Shah, K.B., Chernausek, S.D., Teague, A.M. et al. Maternal diabetes alters microRNA expression in fetal exosomes, human umbilical vein endothelial cells and placenta. Pediatr Res 89, 1157–1163 (2021). https://doi.org/10.1038/s41390-020-1060-x
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-020-1060-x
This article is cited by
-
Exploring the role of miR-126 in diabetes and its complications: a comprehensive review
Diabetology & Metabolic Syndrome (2025)
-
Global DNA methylation and miR-126-3p expression in Mexican women with gestational diabetes mellitus: a pilot study
Molecular Biology Reports (2024)
-
Reciprocal regulation of TWIST1 and OGT determines the decitabine efficacy in MDS/AML
Cell Communication and Signaling (2023)
-
Sex differences in glycolipidic disorders after exposure to maternal hyperglycemia during early development
Journal of Endocrinological Investigation (2023)