Abstract
Background
Oxylipins are formed from oxidation of omega-6 (n6) and omega-3 (n3) fatty acids (FAs). Evidence for inflammatory effects comes mostly from adults.
Methods
Oxylipins from n6 FA (27 n6-oxylipins) and n3 FA (12 n3-oxylipins) were measured through ultra-high-performance liquid chromatography–mass spectrometry (LC-MS/MS) in plasma from 111 children at risk of type 1 diabetes (age 1–17 years) studied longitudinally. Oxylipin precursor FAs (arachidonic acid, linoleic acid, alpha-linolenic acid, docosahexaenoic acid, eicosapentaenoic acid) were measured in red blood cell (RBC) membrane and plasma. Precursor FAs dietary intake was measured through food frequency questionnaire and environmental tobacco smoke (ETS) through questionnaires. Linear mixed models were used to test oxylipins with predictors.
Results
Age associated with 15 n6- and 6 n3-oxylipins; race/ethnicity associated with 3 n6- and 1 n3-oxylipins; sex associated with 2 n6-oxylipins. ETS associated with lipoxin-A4. Oxylipins associated with precursor FAs in plasma more often than RBC. RBC levels and dietary intake of precursor FAs more consistently associated with n3-oxylipins than with n6-oxylipins.
Conclusions
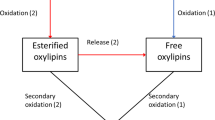
In healthy children, oxylipin levels change with age. Oxylipins associated with precursor FAs more often in plasma than RBC or diet, suggesting that inflammatory regulation leading to FA release into plasma may also be a determinant of oxylipin generation.
Impact
-
This is the first study to examine predictors of oxylipins in healthy children at risk of type 1 diabetes.
-
In healthy children at risk of type 1 diabetes, many oxylipins change with age, and most oxylipins do not differ by sex or race/ethnicity.
-
Environmental tobacco smoke exposure was associated with the presence of lipoxin A4.
-
Omega-6- and omega-3-related oxylipin levels were consistently associated with their respective precursor fatty acid levels measured in the plasma.
-
Proportionally more omega-3 compared to omega-6 oxylipins were associated with dietary intake and red blood cell membrane levels of the respective precursor fatty acid.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Patterson, E., Wall, R., Fitzgerald, G. F., Ross, R. P. & Stanton, C. Health implications of high dietary omega-6 polyunsaturated fatty acids. J. Nutr. Metab. 2012, 539426 (2012).
Totsch, S. K. et al. The impact of the Standard American Diet in rats: effects on behavior, physiology and recovery from inflammatory injury. Scand. J. Pain. 17, 316–324 (2017).
Berkecz, R., Lisa, M. & Holcapek, M. Analysis of oxylipins in human plasma: comparison of ultrahigh-performance liquid chromatography and ultrahigh-performance supercritical fluid chromatography coupled to mass spectrometry. J. Chromatogr. A 1511, 107–121 (2017).
Gabbs, M., Leng, S., Devassy, J. G., Monirujjaman, M. & Aukema, H. M. Advances in our understanding of oxylipins derived from dietary PUFAs. Adv. Nutr. 6, 513–540 (2015).
Radmark, O., Werz, O., Steinhilber, D. & Samuelsson, B. 5-Lipoxygenase, a key enzyme for leukotriene biosynthesis in health and disease. Biochim. Biophys. Acta 1851, 331–339 (2015).
Gilroy, D. W. et al. CYP450-derived oxylipins mediate inflammatory resolution. Proc. Natl Acad. Sci. USA 113, E3240–E3249 (2016).
Liou, Y. A., King, D. J., Zibrik, D. & Innis, S. M. Decreasing linoleic acid with constant alpha-linolenic acid in dietary fats increases (n-3) eicosapentaenoic acid in plasma phospholipids in healthy men. J. Nutr. 137, 945–952 (2007).
Pauls, S. D. et al. Anti-inflammatory effects of alpha-linolenic acid in M1-like macrophages are associated with enhanced production of oxylipins from alpha-linolenic and linoleic acid. J. Nutr. Biochem. 57, 121–129 (2018).
Picklo, M. J. Sr. & Newman, J. W. Antioxidant supplementation and obesity have independent effects on hepatic oxylipin profiles in insulin-resistant, obesity-prone rats. Free Radic. Biol. Med. 89, 182–191 (2015).
Lundstrom, S. L. et al. Lipid mediator serum profiles in asthmatics significantly shift following dietary supplementation with omega-3 fatty acids. Mol. Nutr. Food Res. 57, 1378–1389 (2013).
Duvall, M. G., Bruggemann, T. R. & Levy, B. D. Bronchoprotective mechanisms for specialized pro-resolving mediators in the resolution of lung inflammation. Mol. Asp. Med. 58, 44–56 (2017).
Croasdell, A. et al. Resolvins attenuate inflammation and promote resolution in cigarette smoke-exposed human macrophages. Am. J. Physiol. Lung Cell. Mol. Physiol. 309, L888–L901 (2015).
Shearer, G. C., Harris, W. S., Pedersen, T. L. & Newman, J. W. Detection of omega-3 oxylipins in human plasma and response to treatment with omega-3 acid ethyl esters. J. Lipid Res. 51, 2074–2081 (2010).
Markworth, J. F. et al. Divergent shifts in lipid mediator profile following supplementation with n-3 docosapentaenoic acid and eicosapentaenoic acid. FASEB j. 30, 3714–3725 (2016).
Nording, M. L. et al. Individual variation in lipidomic profiles of healthy subjects in response to omega-3 fatty acids. PLoS ONE 8, e76575 (2013).
Caligiuri, S. P., Aukema, H. M., Ravandi, A. & Pierce, G. N. Elevated levels of pro-inflammatory oxylipins in older subjects are normalized by flaxseed consumption. Exp. Gerontol. 59, 51–57 (2014).
Zulyniak, M. A. et al. Fish oil regulates blood fatty acid composition and oxylipin levels in healthy humans: a comparison of young and older men. Mol. Nutr. Food Res 60, 631–641 (2016).
Strzelak, A., Ratajczak, A., Adamiec, A. & Feleszko, W. Tobacco smoke induces and alters immune responses in the lung triggering inflammation, allergy, asthma and other lung diseases: a mechanistic review. Int. J. Environ. Res. Public Health 15, 1033 (2018).
Rewers, M. et al. Newborn screening for HLA markers associated with IDDM: diabetes autoimmunity study in the young (DAISY). Diabetologia 39, 807–812 (1996).
Norris, J. M. et al. Omega-3 polyunsaturated fatty acid intake and islet autoimmunity in children at increased risk for type 1 diabetes. JAMA 298, 1420–1428 (2007).
American Diabetes Association. 2. Classification and diagnosis of diabetes. Diabetes Care 39(Suppl 1), S13–S22 (2016).
Pedersen, T. L. & Newman, J. W. in Clinical Metabolomics: Methods and Protocols (ed. Giera, M.) 175–212 (Springer, New York, NY, 2018).
Seifert, J. A., Ross, C. A. & Norris, J. M. Validation of a five-question survey to assess a child’s exposure to environmental tobacco smoke. Ann. Epidemiol. 12, 273–277 (2002).
Brady, H. et al. Plasma micronutrients are associated with dietary intake and environmental tobacco smoke exposure in a paediatric population. Public Health Nutr. 10, 712–718 (2007).
Lamb, M. M., Ross, C. A., Brady, H. L. & Norris, J. M. Comparison of children’s diets as reported by the child via the Youth/Adolescent Questionnaire and the parent via the Willett food-frequency questionnaire. Public Health Nutr. 10, 663–670 (2007).
Kind, T. et al. LipidBlast in silico tandem mass spectrometry database for lipid identification. Nat. Methods 10, 755–758 (2013).
Dangour, A. D. et al. Fish consumption and cognitive function among older people in the UK: baseline data from the OPAL study. J. Nutr. Health Aging 13, 198–202 (2009).
Lauretani, F. et al. Plasma polyunsaturated fatty acids and the decline of renal function. Clin. Chem. 54, 475–481 (2008).
Heemskerk, M. M. et al. Prolonged niacin treatment leads to increased adipose tissue PUFA synthesis and anti-inflammatory lipid and oxylipin plasma profile. J. Lipid Res. 55, 2532–2540 (2014).
Lundstrom, S. L. et al. Asthmatics exhibit altered oxylipin profiles compared to healthy individuals after subway air exposure. PLoS ONE 6, e23864 (2011).
Martens, D. S. et al. Neonatal cord blood oxylipins and exposure to particulate matter in the early-life environment: an ENVIRONAGE birth cohort study. Environ. Health Perspect. 125, 691–698 (2017).
Tahan, F., Eke, G. H., Bicici, E., Saraymen, B. & Akar, H. H. Increased postexercise lipoxin A4 levels in exhaled breath condensate in asthmatic children with exercise-induced bronchoconstriction. J. Investig. Allergol. Clin. Immunol. 26, 19–24 (2016).
Sacharzewska, E. et al. The role of 12/15-lipoxygenase in production of selected eicosanoids in allergic airway inflammation. Adv. Med. Sci. 61, 141–146 (2016).
Whyand, T., Hurst, J. R., Beckles, M. & Caplin, M. E. Pollution and respiratory disease: can diet or supplements help? A review. Respir. Res. 19, 79 (2018).
Miyake, Y. et al. Fish and fat intake and prevalence of allergic rhinitis in Japanese females: the Osaka Maternal and Child Health Study. J. Am. Coll. Nutr. 26, 279–287 (2007).
Caligiuri, S. P. et al. Dietary linoleic acid and alpha-linolenic acid differentially affect renal oxylipins and phospholipid fatty acids in diet-induced obese rats. J. Nutr. 143, 1421–1431 (2013).
Berthelot, C. C. et al. Changes in PTGS1 and ALOX12 gene expression in peripheral blood mononuclear cells are associated with changes in arachidonic acid, oxylipins, and oxylipin/fatty acid ratios in response to omega-3 fatty acid supplementation. PLoS ONE 10, e0144996 (2015).
Keenan, A. H. et al. Basal omega-3 fatty acid status affects fatty acid and oxylipin responses to high-dose n3-HUFA in healthy volunteers. J. Lipid Res. 53, 1662–1669 (2012).
Schuchardt, J. P. et al. Increase of EPA-derived hydroxy, epoxy and dihydroxy fatty acid levels in human plasma after a single dose of long-chain omega-3 PUFA. Prostaglandins Other Lipid Mediat. 109–111, 23–31 (2014).
Sun, Y. et al. Plasma fatty acids, oxylipins, and risk of myocardial infarction: the Singapore Chinese Health Study. J. Lipid Res. 57, 1300–1307 (2016).
Heemskerk, M. M. et al. Increased PUFA content and 5-lipoxygenase pathway expression are associated with subcutaneous adipose tissue inflammation in obese women with type 2 diabetes. Nutrients 7, 7676–7690 (2015).
Lands, B., Bibus, D. & Stark, K. D. Dynamic interactions of n-3 and n-6 fatty acid nutrients. Prostaglandins Leukot. Essent. Fatty Acids 136, 15–21 (2018).
Acknowledgements
This work was supported by the National Institutes of Health R01-DK104351 and R01-DK32493.
Author information
Authors and Affiliations
Contributions
T.B. designed the study, performed data analysis, interpreted the data, and drafted the manuscript. J.M.N. designed the study, interpreted the data, and edited the manuscript. B.C.D. and O.F. collected data and reviewed and edited the manuscript. L.A.V., R.K.J., P.M.C., J.S., K.W., M.C.-S. F.D., and M.R. reviewed and edited the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Patient consent
Patient consent was required for this study. All study recruitment and protocols designed to protect participants enrolled in the parent study, DAISY, were approved by the Colorado Multiple Institutional Review Board. All participants provided written informed consent.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Buckner, T., Vanderlinden, L.A., Johnson, R.K. et al. Predictors of oxylipins in a healthy pediatric population. Pediatr Res 89, 1530–1540 (2021). https://doi.org/10.1038/s41390-020-1084-2
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41390-020-1084-2