Abstract
Background
The objective was to determine the association between perioperative risk factors and brain imaging abnormalities on neurologic outcome in neonates with hypoplastic left heart syndrome (HLHS) or d-Transposition of the great arteries (d-TGA) who underwent cardiac surgery including cardiopulmonary bypass.
Methods
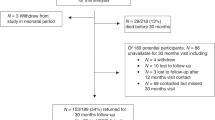
A retrospective analysis of neonates with HLHS or d-TGA undergoing cardiac surgery including cardiopulmonary bypass between 2009 and 2017 was performed. Perioperative risk factors and Andropoulos’ Brain Injury Scores from pre- and postoperative brain magnetic resonant images (MRI) were correlated to outcome assessments on patients between 5 and 23 months of age. Neurologic outcome was measured using the Pediatric Stroke Outcome Measure (PSOM) and Pediatric Version of the Glasgow Outcome Scale-Extended (GOS-E).
Results
Fifty-three neonates met our enrollment criteria (24 HLHS, 29 d-TGA). Mechanical ventilation > 12 days and DHCA > 40 min were associated with worse outcome. MRI measures of brain injuries were not associated with worse outcome by PSOM or GOS-E.
Conclusion
For HLHS and d-TGA patients, duration of mechanical ventilation and DHCA are associated with adverse neurologic outcome. Neonatal brain MRI commonly demonstrates acquired brain injuries, but the clinical impact of these abnormalities are not often seen before 2 years of age.
Impact
-
Acquired brain injury is common in high-risk neonates with CHD but poor neurological outcome was not predicted by severity of injury or lesion subtype. Longer stay in ICU is associated with postoperative brain injuries on MRI.
-
Total duration of ventilation > 12 days is predictive of adverse neurological outcome scores.
-
DHCA > 40 min is associated with adverse neurological outcome scores.
-
Neurological outcome before 2 years of age is more affected by the clinical course than by cardiac diagnosis.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Hoffman, J. I. E. & Kaplan, S. The incidence of congenital heart disease. J. Am. Coll. Cardiol. 39, 1890–1900 (2002).
Gilboa, S. M., Salemi, J. L., Nembhard, W. N., Fixler, D. E. & Correa, A. Mortality resulting from congenital heart disease among children and adults in the United States, 1999 to 2006. Circulation 122, 2254–2263 (2010).
Wernovsky, G. Current insights regarding neurological and developmental abnormalities in children and young adults with complex congenital cardiac disease. Cardiol. Young-. 16, 92–104 (2019).
Latal, B. Neurodevelopmental outcomes of the child with congenital heart disease. Clin. Perinatol. 43, 173–185 (2016).
Limperopoulos, C., Majnemer, A., Shevell, M. I., Rosenblatt, B., Rohlicek, C. & Tchervenkov, C. Neurodevelopmental status of newborns and infants with congenital heart defects before and after open heart surgery. J. Pediatr. 137, 638–645 (2000).
Dittrich, H. Neurodevelopment at 1 year of age in infants with congenital heart disease. Heart 89, 436–441 (2003).
Jain, V. et al. Cerebral oxygen metabolism in neonates with congenital heart disease quantified by MRI and optics. J. Cereb. Blood Flow. Metab. 34, 380–388 (2014).
Andropoulos, D. B. et al. Brain immaturity is associated with brain injury before and after neonatal cardiac surgery with high-flow bypass and cerebral oxygenation monitoring. J. Thorac. Cardiovasc. Surg. 139, 543–556 (2010).
Clouchoux, C. et al. Delayed cortical development in fetuses with complex congenital heart disease. Cereb. Cortex 23, 2932–2943 (2013).
Donofrio, M. T., DuPlessis, A. J. & Limperopoulos, C. Impact of congenital heart disease on fetal brain development and injury. Curr. Opin. Pediatr. 23, 502–511 (2011).
Donofrio, M. T. et al. Autoregulation of cerebral blood flow in fetuses with congenital heart disease: the brain sparing effect. Pediatr. Cardiol. 24, 436–443 (2003).
Kaltman, J. R., Di, H., Tian, Z. & Rychik, J. Impact of congenital heart disease on cerebrovascular blood flow dynamics in the fetus. Ultrasound Obstet. Gynecol. 25, 32–36 (2005).
Limperopoulos, C. et al. Brain volume and metabolism in fetuses with congenital heart disease: evaluation with quantitative magnetic resonance imaging and spectroscopy. Circulation 121, 26–33 (2010).
McQuillen, Patrick S., Goff, Donna A. & Licht, Daniel J. Effects of congenital heart disease on brain development. Prog. Pediatr. Cardiol. 29, 79–85 (2010).
Back, S. A. et al. Protective effects of caffeine on chronic hypoxia-induced perinatal white matter injury. Ann. Neurol. 60, 696–705 (2006).
Marino, B. S. et al. Neurodevelopmental outcomes in children with congenital heart disease: evaluation and management a scientific statement from the american heart association. Circulation 126, 1143–1172 (2012).
Miller, S. P. et al. Abnormal brain development in newborns with congenital heart disease. N. Engl. J. Med. 357, 1928–1938 (2007).
Gaynor, J. W. et al. Is cardiac diagnosis a predictor of neurodevelopmental outcome after cardiac surgery in infancy? J. Thorac. Cardiovasc. Surg. 140, 1230–1237 (2010).
Wypij, D. & Newburger, J. W. et al. The effect of duration of deep hypothermic circulatory arrest in infant heart surgery on late neurodevelopment: the Boston Circulatory Arrest Trial. J. Thorac. Cardiovasc Surg. 126, 1397–1403 (2003).
Andropoulos, D. B. et al. The association between brain injury, perioperative anesthetic exposure, and 12-month neurodevelopmental outcomes after neonatal cardiac surgery: a retrospective cohort study. Paediatr. Anaesth. 24, 266–274 (2015).
Sananes, R. et al. Neurodevelopmental outcomes after open heart operations before 3 months of age. Ann. Thorac. Surg. 93, 1577–1583 (2012).
McQuillen, P. S. et al. Temporal and anatomic risk profile of brain injury with neonatal repair of congenital heart defects. Stroke 38, 736–741 (2007).
Cooper, A. N. et al. The pediatric stroke outcome measure. Neurology 90, e365–e372 (2018).
Beers, S. R. et al. Validity of a Pediatric Version of the Glasgow Outcome Scale—extended. J. Neurotrauma 29, 1126–1139 (2012).
Tavani, F., Zimmerman, R. A., Clancy, R. R., Licht, D. J. & Mahle, W. T. Incidental intracranial hemorrhage after uncomplicated birth: MRI before and after neonatal heart surgery. Neuroradiology 45, 253–258 (2003).
Dimitropoulos, A. et al. Brain injury and development in newborns with critical congenital heart disease. Neurology 81, 241–248 (2013).
McQuillen, P. S. et al. Balloon atrial septostomy is associated with preoperative stroke in neonates with transposition of the great arteries. Circulation 113, 280–285 (2006).
Beca, J. et al. Pre-operative brain injury in newborn infants with transposition of the great arteries occurs at rates similar to other complex congenital heart disease and is not related to balloon atrial septostomy. J. Am. Coll. Cardiol. 53, 1807–1811 (2009).
Petit, C. J. et al. Preoperative brain injury in transposition of the great arteries is associated with oxygenation and time to surgery, not balloon atrial septostomy. Circulation 119, 709–716 (2009).
Bertholdt, S. et al. Cerebral lesions on magnetic resonance imaging correlate with preoperative neurological status in neonates undergoing cardiopulmonary bypass surgery. Eur. J. Cardio-Thorac. Surg. 45, 625–632 (2014).
Kelly, C. J. et al. Neuroimaging findings in newborns with congenital heart disease prior to surgery: an observational study. Arch. Dis. Child 104, 1042–1048 (2019).
Forbess, J. M., Visconti, K. J., Hancock-friesen, C., Howe, R. C., Bellinger, D. C. & Jonas, R. A. Neurodevelopmental outcome after congenital heart surgery: results from an institutional registry. Circulation 106, 95–102 (2002).
Fuller, S. et al. Deep hypothermic circulatory arrest does not impair neurodevelopmental outcome in school-age children after infant cardiac surgery. Ann. Thorac. Surg. 90, 1985–94-5 (2010).
Beca, J. et al. New white matter brain injury after infant heart surgery circulatory arrest. Circulation 127, 971–979 (2013).
Claessens, N. H. P. et al. Perioperative neonatal brain injury is associated with worse school-age neurodevelopment in children with critical congenital heart disease. Dev. Med. Child Neurol. 60, 1052–1058 (2018).
Peyvandi, S. et al. Neonatal brain injury and timing of neurodevelopmental assessment in patients with congenital heart disease. J. Am. Coll. Cardiol. 71, 1986–1996 (2018).
Mcgrath, E., Wypij, D., Rappaport, L. A., Newburger, J. W. & Bellinger, D. C. Prediction of IQ and achievement at age 8 years from neurodevelopmental status at age 1 year in children with D-transposition of the great arteries. Pediatrics 114, 572–576 (2004).
Acknowledgements
V.A.K. was supported by the Kaltenbach doctoral candidate-grant, funded by the German Heart Foundation. This sponsor has no influence on the study design, the collection, analysis, and interpretation of data, the writing of the report or the decision to submit the paper for publication.
Author information
Authors and Affiliations
Contributions
V.A.K.: Study design, initial drafting, project administration, data collection, visualization, critical review, final revision. J.L.C.: Study design, initial drafting, project administration, data collection, data analysis, critical review, final revision, approval of the article. D.Z.: Study design, statistics, data analysis, visualization, critical review, final revision, approval of the article. J.G.R.: Data collection, visualization, critical review. L.T.: Initial drafting, data collection, critical review, approval of the article. M.T.D.: Study design, initial drafting, critical review, approval of the article. R.A.-F.: Initial drafting, critical review, approval of the article. C.L.: Study design, initial drafting, critical review, approval of the article. C.Y.: Supervision, study design, initial drafting, project administration, visualization, data analysis, critical review, final revision, approval of the article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplemental information
Rights and permissions
About this article
Cite this article
Kuhn, V.A., Carpenter, J.L., Zurakowski, D. et al. Determinants of neurological outcome in neonates with congenital heart disease following heart surgery. Pediatr Res 89, 1283–1290 (2021). https://doi.org/10.1038/s41390-020-1085-1
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-020-1085-1
This article is cited by
-
Altered brain structure in preschool-aged children with tetralogy of Fallot
Pediatric Research (2023)
-
Altered white matter connectivity in children with congenital heart disease with single ventricle physiology
Scientific Reports (2023)
-
Predictors of Neurological Outcome Following Infant Cardiac Surgery Without Deep Hypothermic Circulatory Arrest
Pediatric Cardiology (2022)