Abstract
Background
Screening studies have shown that 0.7–4.5% of generally healthy children have isolated diastolic high BP. We therefore studied the characteristics of children with diastolic BP in the elevated and hypertensive ranges according to current guidelines in US children from the National Health and Nutrition Examination Survey (NHANES, 1999–2016).
Methods
We studied 17,362 children (8–18 years) with BP measured by sphygmomanometry. High BP was categorized as isolated systolic (iSH), isolated diastolic (iDH), or Mixed.
Results
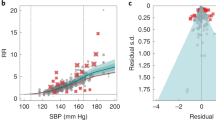
Overall, 86.0% (95% CI = 85.0–87.0) of the population had normal BP, 8.7% (8.0–9.3) elevated BP, 4.9% (4.4–5.5) Stage 1, and 0.4% (0.4–0.6) Stage 2. Moreover, 11.1% (10.3–12.0) had iSH, 1.9% (1.5–2.2) iDH, and 1.0% (0.8–1.2) Mixed. Children with iDH were more likely to be female, younger, white, and leaner than those with iSH, with lower rates of overweight/obesity. iDH was generally between normals and iSH. Resting heart rate was significantly higher in iDH even after adjustment for known covariates.
Conclusions
Children with iDH may have a distinct clinical picture. A leaner habitus and higher resting heart rate may reflect differences in underlying pathophysiology. Longitudinal follow-up studies are needed to better define the pathogenesis, progression, and long-term prognosis in iDH.
Impact
-
Using gold-standard auscultation and 2017 guidelines, isolated diastolic high BP (iDH) is found in 1.9% (95% CI 1.5–2.2) of American children; these children are younger, leaner, more female, and have fewer cardiometabolic risks.
-
Resting heart rate is significantly higher in iDH compared to both normals and iSH even after adjustments for known covariates. Autonomic hyperactivity in iDH may speak to both etiology and therapeutic approaches.
-
iDH appears to be a distinct clinical phenotype characterized by differences in anthropometric measures, sex, age, and resting heart rate. Follow-up studies are clearly needed to clarify its pathogenesis, progression, and prognosis.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Rosner, B., Cook, N., Portman, R., Daniels, S. & Falkner, B. Determination of blood pressure percentiles in normal-weight children: some methodological issues. Am. J. Epidemiol. 167, 653–666 (2008).
Flynn, J. T. et al. Subcommittee on Screening and Management of High Blood Pressure in Children. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics 140, e20171904 (2017).
Sorof, J. M., Poffenbarger, T., Franco, K., Bernard, L. & Portman, R. J. Isolated systolic hypertension, obesity, and hyperkinetic hemodynamic states in children. J. Pediatr. 140, 660–666 (2002).
Karatzi, K. et al. Prevalence of hypertension and hypertension phenotypes by age and gender among schoolchildren in Greece: The Healthy Growth Study. Atherosclerosis 259, 128–133 (2017).
Yang, Y. et al. Prevalence of high blood pressure subtypes and its associations with BMI in Chinese children: a national cross-sectional survey. BMC Public Health 17, 598 (2017).
Pileggi, C., Carbone, V., Nobile, C. G. A. & Pavia, M. Blood pressure and related cardiovascular disease risk factors in 6-18 year-old students in Italy. J. Paediatr. Child Health 41, 347–352 (2005).
Manios, Y. et al. Prevalence of childhood hypertension and hypertension phenotypes by weight status and waist circumference: the Healthy Growth Study. Eur. J. Nutr. 57, 1147–1155 (2018).
Berney, M., Burnier, M. & Wuerzner, G. [Isolated diastolic hypertension: do we still have to care about it?]. Rev. Med Suisse 14, 1607–1610 (2018).
NHANES Questionnaires, Datasets, and Related Documentation. https://wwwn.cdc.gov/nchs/nhanes/Default.aspx (2020).
NHANES Examination Data. https://wwwn.cdc.gov/nchs/nhanes/search/datapage.aspx?Component=Examination&CycleBeginYear= (2020).
Sharma, A. K., Metzger, D. L. & Rodd, C. J. Prevalence and severity of high blood pressure among children based on the 2017 American Academy of Pediatrics Guidelines. JAMA Pediatr. 172, 557–565 (2018).
Kuczmarski, R. J. et al. 2000 CDC growth charts for the United States: methods and development. Vital Health Stat. 11, 1–190 (2002).
de Onis, M. et al. Development of a WHO growth reference for school-aged children and adolescents. Bull. World Health Organ. 85, 660–667 (2007).
Sharma, A. K., Metzger, D. L., Daymont, C., Hadjiyannakis, S. & Rodd, C. J. LMS tables for waist-circumference and waist-height ratio Z-scores in children aged 5-19 y in NHANES III: association with cardio-metabolic risks. Pediatr. Res. 78, 723–729 (2015).
Addo, O. Y., Himes, J. H. & Zemel, B. S. Reference ranges for midupper arm circumference, upper arm muscle area, and upper arm fat area in US children and adolescents aged 1-20 y. Am. J. Clin. Nutr. 105, 111–120 (2017).
Addo, O. Y. & Himes, J. H. Reference curves for triceps and subscapular skinfold thicknesses in US children and adolescents. Am. J. Clin. Nutr. 91, 635–642 (2010).
Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents, National Heart, Lung, and Blood Institute. Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report. Pediatrics 128, S213–S256 (2011).
American Diabetes Association. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2020. Diabetes Care 43, S14–S31 (2020).
Schwartz, G. J. et al. New equations to estimate GFR in children with CKD. J. Am. Soc. Nephrol. 20, 629–637 (2009).
Pottel, H. et al. An estimated glomerular filtration rate equation for the full age spectrum. Nephrol. Dial. Transpl. 31, 798–806 (2016).
R: The R Project for Statistical Computing. https://www.r-project.org/ (2020).
Lumley, T. Complex Surveys: A Guide to Analysis Using R (Wiley and Sons, Hoboken, New Jersey, 2010).
Fleming, S. et al. Normal ranges of heart rate and respiratory rate in children from birth to 18 years of age: a systematic review of observational studies. Lancet 377, 1011–1018 (2011).
Kubota, M. Hyperuricemia in children and adolescents: present knowledge and future directions. J. Nutr. Metab. 2019, 3480718 (2019).
Miranda, J. J., Stanojevic, S., Bernabe-Ortiz, A., Gilman, R. H. & Smeeth, L. Performance of oscillometric blood pressure devices in children in resource-poor settings. Eur. J. Cardiovasc. Prev. Rehabil. 15, 362–364 (2008).
Rosner, B., Cook, N. R., Daniels, S. & Falkner, B. Childhood blood pressure trends and risk factors for high blood pressure: the NHANES experience 1988-2008. Hypertension 62, 247–254 (2013).
Flynn, J. T. Adiposity, the sympathetic nervous system, and childhood primary hypertension. Hypertension 62, 689–690 (2013).
Burke, G. L., Freedman, D. S., Webber, L. S. & Berenson, G. S. Persistence of high diastolic blood pressure in thin children. The Bogalusa Heart Study. Hypertension 8, 24–29 (1986).
Bell, C. S., Samuel, J. P. & Samuels, J. A. Prevalence of hypertension in children. Hypertension 73, 148–152 (2019).
Kollias, A., Pantsiotou, K., Karpettas, N., Roussias, L. & Stergiou, G. S. Tracking of blood pressure from childhood to adolescence in a Greek cohort. Eur. J. Public Health 22, 389–393 (2012).
Bao, W., Threefoot, S. A., Srinivasan, S. R. & Berenson, G. S. Essential hypertension predicted by tracking of elevated blood pressure from childhood to adulthood: the Bogalusa Heart Study. Am. J. Hypertens. 8, 657–665 (1995).
Nicklas, T. A., von Duvillard, S. P. & Berenson, G. S. Tracking of serum lipids and lipoproteins from childhood to dyslipidemia in adults: the Bogalusa Heart Study. Int. J. Sports Med. 23, S39–S43 (2002).
Sundström, J., Neovius, M., Tynelius, P. & Rasmussen, F. Association of blood pressure in late adolescence with subsequent mortality: cohort study of Swedish male conscripts. BMJ 342, d643 (2011).
Chen, X. & Wang, Y. Tracking of blood pressure from childhood to adulthood: a systematic review and meta-regression analysis. Circulation 117, 3171–3180 (2008).
Whelton, P. K. et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 71, e127–e248 (2018).
Lewington, S., Clarke, R., Qizilbash, N., Peto, R. & Collins, R. Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 360, 1903–1913 (2002).
Leiba, A. et al. Prehypertension among 2.19 million adolescents and future risk for end-stage renal disease. J. Hypertens. 35, 1290–1296 (2017).
Author information
Authors and Affiliations
Contributions
All authors met the authorship requirements of Pediatric Research. A.S., C.R., and H.B.A. conceptualized and designed the study, carried out the initial analyses, drafted the initial manuscript, and reviewed and revised the manuscript. D.L.M. and T.B.-H. conceptualized and designed the study and reviewed and revised the manuscript. All authors approved the final manuscript as submitted.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Patient consent
Patient consent was obtained at the time of the NHANES survey.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Alsaeed, H., Metzger, D.L., Blydt-Hansen, T.D. et al. Isolated diastolic high blood pressure: a distinct clinical phenotype in US children. Pediatr Res 90, 903–909 (2021). https://doi.org/10.1038/s41390-021-01369-x
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-021-01369-x
This article is cited by
-
Isolated diastolic hypertension and incident cardio-renal-metabolic multimorbidity in the Tehran Lipid and Glucose Study: comparison of ACC/AHA and ESC/NICE guideline definitions
Hypertension Research (2025)
-
Utility of home doppler blood pressure measurement to minimise unnecessary investigations in children with suspected hypertension
Journal of Human Hypertension (2025)
-
Precision approaches to paediatric hypertension: linking pathophysiology to therapy
Pediatric Nephrology (2025)
-
Ambulatory isolated diastolic hypertension and risk of left ventricular hypertrophy in children with primary and secondary hypertension
Pediatric Nephrology (2024)
-
Variation in paediatric 24-h ambulatory blood pressure monitoring interpretation by Canadian and UK physicians
Journal of Human Hypertension (2022)