Abstract
Background
Teaching caregivers to respond to normal infant night awakenings in ways other than feeding is a common obesity prevention effort. Models can simulate caregiver feeding behavior while controlling for variables that are difficult to manipulate or measure in real life.
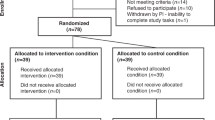
Methods
We developed a virtual infant model representing an infant with an embedded metabolism and his/her daily sleep, awakenings, and feeds from their caregiver each day as the infant aged from 6 to 12 months (recommended age to introduce solids). We then simulated different night feeding interventions and their impact on infant body mass index (BMI).
Results
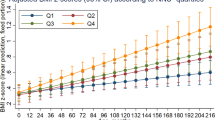
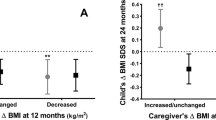
Reducing the likelihood of feeding during normal night wakings from 79% to 50% to 10% lowered infant BMI from the 84th to the 75th to the 62nd percentile by 12 months, respectively, among caregivers who did not adaptively feed (e.g., adjust portion sizes of solid foods with infant growth). Among caregivers who adaptively feed, all scenarios resulted in relatively stable BMI percentiles, and progressively reducing feeding probability by 10% each month showed the least fluctuations.
Conclusions
Reducing night feeding has the potential to impact infant BMI, (e.g., 10% lower probability can reduce BMI by 20 percentile points) especially among caregivers who do not adaptively feed.
Impact
-
Teaching caregivers to respond to infant night waking with other soothing behaviors besides feeding has the potential to reduce infant BMI.
-
When reducing the likelihood of feeding during night wakings from 79% to 50% to 10%, infants dropped from the 84th BMI percentile to the 75th to the 62nd by 12 months, respectively, among caregivers who do not adaptively feed.
-
Night-feeding interventions have a greater impact when caregivers do not adaptively feed their infant based on their growth compared to caregivers who do adaptively feed.
-
Night-feeding interventions should be one of the several tools in a multi-component intervention for childhood obesity prevention.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Taheri, S. The link between short sleep duration and obesity: we should recommend more sleep to prevent obesity. Arch. Dis. Child. 91, 881–884 (2006).
Taveras, E. M. et al. Short sleep duration in infancy and risk of childhood overweight. Arch. Pediatr. Adolesc. Med. 162, 305–311 (2008).
Hart, C. N. & Jelalian, E. Shortened sleep duration is associated with pediatric overweight. Behav. Sleep Med. 6, 251–267 (2008).
Reilly, J. J. et al. Early life risk factors for obesity in childhood: cohort study. BMJ 330, 1357 (2005).
McDonald, L. et al. Sleep and nighttime energy consumption in early childhood: a population‐based cohort study. Pediatr. Obes. 10, 454–460 (2015).
Miller, M. A. et al. Sleep duration and incidence of obesity in infants, children, and adolescents: a systematic review and meta-analysis of prospective studies. Sleep 41, zsy018 (2018).
Magee, L. & Hale, L. Longitudinal associations between sleep duration and subsequent weight gain: a systematic review. Sleep Med. Rev. 16, 231–241 (2012).
Snell, E. K., Adam, E. K. & Duncan, G. J. Sleep and the body mass index and overweight status of children and adolescents. Child Dev. 78, 309–323 (2007).
Nielsen, L., Danielsen, K. & Sørensen, T. Short sleep duration as a possible cause of obesity: critical analysis of the epidemiological evidence. Obes. Rev. 12, 78–92 (2011).
Wake, M. et al. Does an intervention that improves infant sleep also improve overweight at age 6? Follow-up of a randomised trial. Arch. Dis. Child. 96, 526–532 (2011).
Taylor, B. J. et al. Targeting sleep, food, and activity in infants for obesity prevention: an RCT. Pediatrics 139, e20162037 (2017).
Savage, J. S. et al. Effect of the INSIGHT responsive parenting intervention on rapid infant weight gain and overweight status at age 1 year: a randomized clinical trial. JAMA Pediatr. 170, 742–749 (2016).
Paul, I. M. et al. Preventing obesity during infancy: a pilot study. Obesity 19, 353–361 (2011).
Field, T. Infant sleep problems and interventions: a review. Infant Behav. Dev. 47, 40–53 (2017).
Ferguson, M. C. et al. Can following formula-feeding recommendations still result in infants who are overweight or have obesity? Pediatr. Res. 88, 661–667 (2020).
Ferguson, M. C. et al. The impact of following solid food feeding guides on BMI among infants: a simulation study. Am. J. Prev. Med. 57, 355–364 (2019).
van Rossum, G. & Drake, F. L. Python Reference Manual (PythonLabs, 2001).
Hall, K. D. Modeling metabolic adaptations and energy regulation in humans. Annu. Rev. Nutr. 32, 35–54 (2012).
Rahmandad, H. Human growth and body weight dynamics: an integrative systems model. PLoS ONE 9, e114609 (2014).
Butte, N. F. Energy requirements of infants. Public Health Nutr. 8, 953–967 (2005).
Sadeh, A., Mindell, J. A., Luedtke, K. & Wiegand, B. Sleep and sleep ecology in the first 3 years: a web‐based study. J. Sleep Res. 18, 60–73 (2009).
Prell, C. & Koletzko, B. Breastfeeding and complementary feeding: recommendations on infant nutrition. Dtsch. Ärzteblatt Int. 113, 435 (2016).
Grummer-Strawn, L. M., Scanlon, K. S. & Fein, S. B. Infant feeding and feeding transitions during the first year of life. Pediatrics 122, S36–S42 (2008).
Casiday, R. E., Wright, C. M., Panter-Brick, C. & Parkinson, K. Do early infant feeding patterns relate to breast-feeding continuation and weight gain? Data from a longitudinal cohort study. Eur. J. Clin. Nutr. 58, 1290–1296 (2004).
Syrad, H., Johnson, L., Wardle, J. & Llewellyn, C. H. Appetitive traits and food intake patterns in early life. Am. J. Clin. Nutr. 103, 231–235 (2016).
Iglowstein, I., Jenni, O. G., Molinari, L. & Largo, R. H. Sleep duration from infancy to adolescence: reference values and generational trends. Pediatrics 111, 302–307 (2003).
Ball, H. L. Breastfeeding, bed‐sharing, and infant sleep. Birth 30, 181–188 (2003).
Brown, A. & Harries, V. Infant sleep and night feeding patterns during later infancy: association with breastfeeding frequency, daytime complementary food intake, and infant weight. Breastfeed. Med. 10, 246–252 (2015).
Dewey, K. G. Nutrition, growth, and complementary feeding of the brestfed infant. Pediatr. Clin. North Am. 48, 87–104 (2001).
Butte, N. F. et al. Energy requirements derived from total energy expenditure and energy deposition during the first 2 y of life. Am. J. Clin. Nutr. 72, 1558–1569 (2000).
World Health Organization. WHO Growth charts - data table for girls length-for-age and weight-for-age charts. National Center for Health Statistics, Centers for Disease Control and Prevention, https://www.cdc.gov/growthcharts/who/girls_length_weight.htm (2010).
World Health Organization. WHO Growth charts - data table for boys length-for-age and weight-for-age charts. National Center for Health Statistics, Centers for Disease Control and Prevention, https://www.cdc.gov/growthcharts/who/boys_length_weight.htm (2010).
Douglas, P. S. & Hill, P. S. Behavioral sleep interventions in the first six months of life do not improve outcomes for mothers or infants: a systematic review. J. Dev. Behav. Pediatr. 34, 497–507 (2013).
Toomey, E. et al. A collaborative approach to developing sustainable behaviour change interventions for childhood obesity prevention: development of the Choosing Healthy Eating for Infant Health (CHErIsH) intervention and implementation strategy. Br. J. Health Psychol. 25, 275–304 (2020).
Adair, R. et al. Reducing night waking in infancy: a primary care intervention. Pediatrics 89, 585–588 (1992).
St James-Roberts, I., Roberts, M., Hovish, K. & Owen, C. Video evidence that parenting methods predict which infants develop long night-time sleep periods by three months of age. Prim. Health Care Res. Dev. 18, 212–226 (2017).
Scher, A. Attachment and sleep: a study of night waking in 12‐month‐old infants. Dev. Psychobiol. 38, 274–285 (2001).
Blunden, S. L., Thompson, K. R. & Dawson, D. Behavioural sleep treatments and night time crying in infants: challenging the status quo. Sleep Med. Rev. 15, 327–334 (2011).
Gradisar, M. et al. Behavioral interventions for infant sleep problems: a randomized controlled trial. Pediatrics 137, e20151486 (2016).
Mullins, E. N. et al. Acute sleep restriction increases dietary intake in preschool‐age children. J. Sleep Res. 26, 48–54 (2017).
Leproult, R. & Van Cauter, E. Role of sleep and sleep loss in hormonal release and metabolism. Endocr. Dev. 17, 11–21 (2010).
Hart, C. N. et al. Changes in children’s sleep duration on food intake, weight, and leptin. Pediatrics 132, e1473–e1480 (2013).
Acknowledgements
This project was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) via grant U01HD086861 and 5R01HD086013-02, as well as the NICHD and Office of Behavioral and Social Sciences Research (OBSSR) under award number U54HD070725, and the National Institute of General Medical Sciences (NIGMS) as part of the Models of Infectious Disease Agent Study (MIDAS) network under grant 1 R01 GM127512-01A1. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health, U.S. Department of Health and Human Services, NICHD, NIGMS or OBSSR. None of the study sponsors had any role in the study design, collection, analysis, and interpretation of data, writing the report, nor the decision to submit the report for publication. This study was approved by the Johns Hopkins Bloomberg School of Public Health IRB (IRB #00006667).
Author information
Authors and Affiliations
Contributions
Substantial contributions to conception and design; acquisition of data, or analysis and interpretation of data; drafting the article or revising it critically for important intellectual content; and final approval of the version to be published: all authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Patient consent
Patient consent was not required for this study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
O’Shea, K.J., Ferguson, M.C., Esposito, L. et al. The impact of reducing the frequency of night feeding on infant BMI. Pediatr Res 91, 254–260 (2022). https://doi.org/10.1038/s41390-021-01397-7
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41390-021-01397-7
This article is cited by
-
Breast milk feeding practices and frequencies among complementary-fed children: a cross-sectional study in Northern Thailand
International Breastfeeding Journal (2025)