Abstract
Background
Neonatal encephalopathy (NE) is a major cause of long-term neurodevelopmental disability in neonates. We evaluated the ability of serially measured biomarkers of brain injury to predict adverse neurological outcomes in this population.
Methods
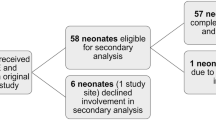
Circulating brain injury biomarkers including BDNF, IL-6, IL-8, IL-10, VEGF, Tau, GFAP, and NRGN were measured at 0, 12, 24, 48, 72, and 96 h of cooling from 103 infants with NE undergoing TH. The biomarkers’ individual and combinative ability to predict death or severe brain injury and adverse neurodevelopmental outcomes beyond 1 year of age was assessed.
Results
Early measurements of inflammatory cytokines IL-6, 8, and 10 within 24 HOL (AUC = 0.826) and late measurements of Tau from 72 to 96 HOL (AUC = 0.883, OR 4.37) were accurate in predicting severe brain injury seen on MRI. Late measurements of Tau were predictive of adverse neurodevelopmental outcomes (AUC = 0.81, OR 2.59).
Conclusions
Tau was consistently a predictive marker for brain injury in neonates with NE. However, in the first 24 HOL, IL-6, 8, and 10 in combination were most predictive of death or severe brain injury. The results of this study support the use of a serial biomarker panel to assess brain injury over the time course of disease in NE.
Impact
-
While recent studies have evaluated candidate brain injury biomarkers, no biomarker is in current clinical use.
-
This study supports the use of a serial biomarker panel for ongoing assessment of brain injury neonates with NE.
-
In combination, IL6, IL8, and IL10 in the first 24 h of cooling were more predictive of brain injury by MRI than each cytokine alone.
-
Individually, Tau was overall most consistently predictive of adverse neurological outcomes, particularly when measured at or after rewarming.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Shankaran, S., Woldt, E., Koepke, T., Bedard, M. P. & Nandyal, R. Acute neonatal morbidity and long-term central nervous system sequelae of perinatal asphyxia in term infants. Early Hum. Dev. 25, 135–148 (1991).
Gluckman, P. D. et al. Selective head cooling with mild systemic hypothermia after neonatal encephalopathy: multicentre randomised trial. Lancet Lond. Engl. 365, 663–670 (2005).
Kurinczuk, J. J., White-Koning, M. & Badawi, N. Epidemiology of neonatal encephalopathy and hypoxic-ischaemic encephalopathy. Early Hum. Dev. 86, 329–338 (2010).
Shankaran, S. et al. Whole-body hypothermia for neonates with hypoxic-ischemic encephalopathy. N. Engl. J. Med. 353, 1574–1584 (2005).
Wu, Y. W. et al. High-dose erythropoietin and hypothermia for hypoxic-ischemic encephalopathy: a Phase II Trial. Pediatrics 137, e20160191 (2016).
Orrock, J. E. et al. Association of brain injury and neonatal cytokine response during therapeutic hypothermia in newborns with hypoxic-ischemic encephalopathy. Pediatr. Res. 79, 742–747 (2016).
Chalak, L. F. et al. Biomarkers for severity of neonatal hypoxic-ischemic encephalopathy and outcomes in newborns receiving hypothermia therapy. J. Pediatr. 164, 468–474.e1 (2014).
Takahashi, K. et al. Serum tau protein level serves as a predictive factor for neurological prognosis in neonatal asphyxia. Brain Dev. 36, 670–675 (2014).
Ennen, C. S. et al. Glial fibrillary acidic protein as a biomarker for neonatal hypoxic-ischemic encephalopathy treated with whole-body cooling. Am. J. Obstet. Gynecol. 205, 251.e1–7 (2011).
Kubota, Y., Putkey, J. A. & Waxham, M. N. Neurogranin controls the spatiotemporal pattern of postsynaptic Ca2+/CaM signaling. Biophys. J. 93, 3848–3859 (2007).
Massaro, A. N. et al. Plasma biomarkers of brain injury in neonatal hypoxic-ischemic encephalopathy. J. Pediatr. 194, 67–75.e1 (2018).
Ramaswamy, V. et al. Systematic review of biomarkers of brain injury in term neonatal encephalopathy. Pediatr. Neurol. 40, 215–226 (2009).
Massaro, A. N. et al. Biomarkers of brain injury in neonatal encephalopathy treated with hypothermia. J. Pediatr. 161, 434–440 (2012).
Massaro, A. N. et al. Biomarkers S100B and neuron-specific enolase predict outcome in hypothermia-treated encephalopathic newborns. Pediatr. Crit. Care Med. 15, 615–622 (2014).
Sarnat, H. B. & Sarnat, M. S. Neonatal encephalopathy following fetal distress. A clinical and electroencephalographic study. Arch. Neurol. 33, 696–705 (1976).
Dietrick, B. et al. Plasma and CSF candidate biomarkers of neonatal encephalopathy severity and neurodevelopmental outcomes. J. Pediatr. https://doi.org/10.1016/j.jpeds.2020.06.078 (2020).
Yang, J., Korley, F. K., Dai, M. & Everett, A. D. Serum neurogranin measurement as a biomarker of acute traumatic brain injury. Clin. Biochem. 48, 843–848 (2015).
Bembea, M. M. et al. Glial fibrillary acidic protein as a brain injury biomarker in children undergoing extracorporeal membrane oxygenation. Pediatr. Crit. Care Med. 12, 572–579 (2011).
Barkovich, A. J. et al. Prediction of neuromotor outcome in perinatal asphyxia: evaluation of MR scoring systems. Am. J. Neuroradiol. 19, 143–149 (1998).
Michalec, D. in Encyclopedia of Child Behavior and Development (eds Goldstein, S. & Naglieri, J. A.) 215–215 (2011).
Anderson, P. J. et al. Underestimation of developmental delay by the new Bayley-III Scale. Arch. Pediatr. Adolesc. Med. 164, 352–356 (2010).
Vohr, B. R. et al. Are outcomes of extremely preterm infants improving? Impact of Bayley assessment on outcomes. J. Pediatr. 161, 222–8.e3 (2012).
Chalak, L. F. et al. Neurodevelopmental outcomes after hypothermia therapy in the era of Bayley-III. J. Perinatol. Off. J. Calif. Perinat. Assoc. 34, 629–633 (2014).
Moore, T., Johnson, S., Haider, S., Hennessy, E. & Marlow, N. Relationship between test scores using the second and third editions of the Bayley Scales in extremely preterm children. J. Pediatr. 160, 553–558 (2012).
Jenkins, D. D. et al. Serum cytokines in a clinical trial of hypothermia for neonatal hypoxic-ischemic encephalopathy. J. Cereb. Blood Flow. Metab. 32, 1888–1896 (2012).
Wu, H. et al. SBDPs and Tau proteins for diagnosis and hypothermia therapy in neonatal hypoxic ischemic encephalopathy. Exp. Ther. Med. 13, 225–229 (2017).
Acknowledgements
This study was supported by the Clinical and Translational Science Institute at Children’s National (UL1TR000075, 1KL2RR031987-01) and the National Institutes of Health Intellectual and Developmental Disabilities Research Consortium (U54 HD090257).
Author information
Authors and Affiliations
Contributions
Substantial contributions to conception and design (T.C., A.D.E, P.G., J.B., A.N.M.), acquisition of data (M.M.M., A.C.O., G.V., T.C., N.B., P.G., A.N.M.), or analysis (J.G., J.B.) and interpretation of data (G.V., T.C., P.G., J.B., A.D.E., A.N.M.); drafting the article (M.M.M.) or revising it critically for important intellectual content (all authors); and final approval of the version to be published (all authors).
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent statement
Written informed consent for enrollment into this study was obtained from the parents of participants.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
McGowan, M.M., O’Kane, A.C., Vezina, G. et al. Serial plasma biomarkers of brain injury in infants with neonatal encephalopathy treated with therapeutic hypothermia. Pediatr Res 90, 1228–1234 (2021). https://doi.org/10.1038/s41390-021-01405-w
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-021-01405-w
This article is cited by
-
Stay cool and keep moving forwards
Pediatric Research (2025)