Abstract
BACKGROUND
Few studies have characterized follow-up after pediatric acute kidney injury (AKI). Our aim was to describe outpatient AKI follow-up after pediatric intensive care unit (PICU) admission.
METHODS
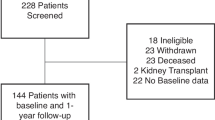
Two-center retrospective cohort study (0–18 years; PICU survivors (2003–2005); noncardiac surgery; and no baseline kidney disease). Provincial administrative databases were used to determine outcomes. Exposure: AKI (KDIGO (Kidney Disease: Improving Global Outcomes) definitions). Outcomes: post-discharge nephrology, family physician, pediatrician, and non-nephrology specialist visits. Regression was used to evaluate factors associated with the presence of nephrology follow-up (Cox) and the number of nephrology and family physician or pediatrician visits (Poisson), among AKI survivors.
RESULTS
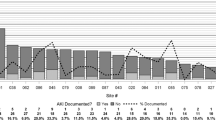
Of n = 2041, 355 (17%) had any AKI; 64/355 (18%) had nephrology; 198 (56%) had family physician or pediatrician; and 338 (95%) had family physician, pediatrician, or non-nephrology specialist follow-up by 1 year post discharge. Only 44/142 (31%) stage 2–3 AKI patients had nephrology follow-up by 1 year. Inpatient nephrology consult (adjusted hazard ratio (aHR) 7.76 [95% confidence interval (CI) 4.89–12.30]), kidney admission diagnosis (aHR 4.26 [2.21–8.18]), and AKI non-recovery by discharge (aHR 2.65 [1.55–4.55]) were associated with 1-year nephrology follow-up among any AKI survivors.
CONCLUSIONS
Nephrology follow-up after AKI was uncommon, but nearly all AKI survivors had follow-up with non-nephrologist physicians. This suggests that AKI follow-up knowledge translation strategies for non-nephrology providers should be a priority.
Impact
-
Pediatric AKI survivors have high long-term rates of chronic kidney disease (CKD) and hypertension, justifying regular kidney health surveillance after AKI.
-
However, there is limited pediatric data on follow-up after AKI, including the factors associated with nephrology referral and extent of non-nephrology follow-up.
-
We found that only one-fifth of all AKI survivors and one-third of severe AKI (stage 2–3) survivors have nephrology follow-up within 1 year post discharge.
-
However, 95% are seen by a family physician, pediatrician, or non-nephrology specialist within 1 year post discharge.
-
This suggests that knowledge translation strategies for AKI follow-up should be targeted at non-nephrology healthcare providers.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Wang, L. et al. Electronic health record-based predictive models for acute kidney injury screening in pediatric inpatients. Pediatr. Res. 82, 465–473 (2017).
Kaddourah, A. et al. Epidemiology of acute kidney injury in critically ill children and young adults. N. Engl. J. Med. 376, 11–20 (2017).
Kari, J. A. et al. Outcome of pediatric acute kidney injury: a multicenter prospective cohort study. Pediatr. Nephrol. 33, 335–340 (2018).
Sutherland, S. M. et al. AKI in hospitalized children: epidemiology and clinical associations in a national cohort. Clin. J. Am. Soc. Nephrol. 8, 1661–1669 (2013).
Susantitaphong, P. et al. World incidence of AKI: a meta-analysis. Clin. J. Am. Soc. Nephrol. 8, 1482–1493 (2013).
Sutherland, S. M. et al. AKI in hospitalized children: comparing the pRIFLE, AKIN, and KDIGO definitions. Clin. J. Am. Soc. Nephrol. 10, 554–561 (2015).
Alkandari, O. et al. Acute kidney injury is an independent risk factor for pediatric intensive care unit mortality, longer length of stay and prolonged mechanical ventilation in critically ill children: a two-center retrospective cohort study. Crit. Care 15, R146 (2011).
Hessey, E. et al. Long-term mortality after acute kidney injury in the pediatric ICU. Hosp. Pediatr. 8, 260–268 (2018).
Greenberg, J. H., Coca, S. & Parikh, C. R. Long-term risk of chronic kidney disease and mortality in children after acute kidney injury: a systematic review. BMC Nephrol. 15, 184 (2014).
Hui-Stickle, S., Brewer, E. D. & Goldstein, S. L. Pediatric ARF epidemiology at a tertiary care center from 1999 to 2001. Am. J. Kidney Dis. 45, 96–101 (2005).
Askenazi, D. J. et al. 3-5 year longitudinal follow-up of pediatric patients after acute renal failure. Kidney Int. 69, 184–189 (2006).
Greenberg, J. H. et al. Kidney outcomes 5 years after pediatric cardiac surgery: the TRIBE-AKI study. JAMA Pediatr. 170, 1071–1078 (2016).
Mammen, C. et al. Long-term risk of CKD in children surviving episodes of acute kidney injury in the intensive care unit: a prospective cohort study. Am. J. Kidney Dis. 59, 523–530 (2012).
Menon, S., Kirkendall, E. S., Nguyen, H. & Goldstein, S. L. Acute kidney injury associated with high nephrotoxic medication exposure leads to chronic kidney disease after 6 months. J. Pediatr. 165, 522–527.e2 (2014).
Hollander, S. A. et al. Recovery from acute kidney injury and CKD following heart transplantation in children, adolescents, and young adults: a retrospective cohort study. Am. J. Kidney Dis. 68, 212–218 (2016).
Madsen, N. L. et al. Cardiac surgery in patients with congenital heart disease is associated with acute kidney injury and the risk of chronic kidney disease. Kidney Int. 92, 751–756 (2017).
Garg, A. X. et al. Long-term renal prognosis of diarrhea-associated hemolytic uremic syndrome: a systematic review, meta-analysis, and meta-regression. JAMA 290, 1360–1370 (2003).
Cooper, D. S. et al. Follow-up renal assessment of injury long-term after acute kidney injury (FRAIL-AKI). Clin. J. Am. Soc. Nephrol. 11, 21–29 (2016).
Hirano, D. et al. Independent risk factors and 2-year outcomes of acute kidney injury after surgery for congenital heart disease. Am. J. Nephrol. 46, 204–209 (2017).
Hoffmeister, P. A. et al. Hypertension in long-term survivors of pediatric hematopoietic cell transplantation. Biol. Blood Marrow Transplant. 16, 515–524 (2010).
Hessey, E. et al. Acute kidney injury in critically ill children and subsequent chronic kidney disease. Can. J. Kidney Health Dis. 6, 2054358119880188 (2019).
Kashani, K. et al. Quality improvement goals for acute kidney injury. Clin. J. Am. Soc. Nephrol. 14, 941–953 (2019).
Goldstein, S. L. et al. AKI transition of care: a potential opportunity to detect and prevent CKD. Clin. J. Am. Soc. Nephrol. 8, 476–483 (2013).
Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group. KDIGO Clinical Practice Guideline for Acute Kidney Injury. Section 2: AKI definition. Kidney Int. Suppl. 2, 19–36 (2012).
Hessey, E. et al. Healthcare utilization after acute kidney injury in the pediatric intensive care unit. Clin. J. Am. Soc. Nephrol. 13, 685–692 (2018).
Harel, Z. et al. Nephrologist follow-up improves all-cause mortality of severe acute kidney injury survivors. Kidney Int. 83, 901–908 (2013).
Khan, I. H., Catto, G. R., Edward, N. & Macleod, A. M. Acute renal failure: factors influencing nephrology referral and outcome. QJM 90, 781–785 (1997).
Silver, S. A. et al. Ambulatory care after acute kidney injury: an opportunity to improve patient outcomes. Can. J. Kidney Health Dis. 2, 71 (2015) .
Hessey, E. et al. Renal function follow-up and renal recovery after acute kidney injury in critically ill children. Pediatr. Crit. Care Med. 18, 733–740 (2017).
D’Arienzo, D. et al. A validation study of administrative health care data to detect acute kidney injury in the pediatric intensive care unit. Can. J. Kidney Health Dis. 6, 205435811982752 (2019).
Hessey, E. et al. Evaluation of height-dependent and height-independent methods of estimating baseline serum creatinine in critically ill children. Pediatr. Nephrol. 32, 1953–1962 (2017).
Simon, T. D. et al. Pediatric medical complexity algorithm: a new method to stratify children by medical complexity. Pediatrics 133, e1647–e1654 (2014).
United States Renal Data System. USRDS Annual Data Report: Epidemiology of Kidney Disease in the United States (National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, 2018).
Karsanji, D. J. et al. Disparity between nephrologists’ opinions and contemporary practices for community follow-up after AKI hospitalization. Clin. J. Am. Soc. Nephrol. 12, 1753–1761 (2017).
Sigurjonsdottir, V. K., Chaturvedi, S., Mammen, C. & Sutherland, S. M. Pediatric acute kidney injury and the subsequent risk for chronic kidney disease: is there cause for alarm? Pediatr. Nephrol. 33, 2047–2055 (2018).
Benisty, K. et al. Kidney and blood pressure abnormalities 6 years after acute kidney injury in critically ill children: a prospective cohort study. Pediatr. Res. 88, 271–278 (2020).
Acknowledgements
This work was funded by an operating grant from the Fonds de Recherche du Quebec-Sante. M.Z. was supported by a research salary award from the Fonds de Recherche du Quebec-Sante during the performance of the majority of this work.
Author information
Authors and Affiliations
Contributions
C.R., R.C. and M.Z. conceptualized and designed the study, coordinated and supervised data collection and/or analysis, drafted the initial manuscript, and reviewed and revised the manuscript. J.L., P.J. and V.P. conceptualized and designed the study, coordinated and supervised data collection and analysis, and reviewed and revised the manuscript. E.H. and S.N. conceptualized and designed the study, performed data collection, reviewed data analyses, assisted with data interpretation, and reviewed and revised the manuscript. M.D. reviewed and revised the proposed study design, was primarily responsible for data analysis, and reviewed and revised the manuscript. All authors have approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Data sharing
Deidentified individual participant data will not be made available.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent
Informed consent was waived due to the retrospective nature of the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Robinson, C., Hessey, E., Nunes, S. et al. Acute kidney injury in the pediatric intensive care unit: outpatient follow-up. Pediatr Res 91, 209–217 (2022). https://doi.org/10.1038/s41390-021-01414-9
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-021-01414-9
This article is cited by
-
From acute kidney injury to chronic kidney disease in children: maladaptive repair and the need for long-term surveillance - a literature review
BMC Nephrology (2025)
-
Sepsis criteria and kidney function: eliminating sex, age and economic status biases
Nature Reviews Nephrology (2025)
-
Exploring Racial and Ethnic Disparities in Outcomes Following Pediatric Cardiac Surgery: A NEPHRON Study Analysis
Pediatric Cardiology (2025)
-
Acute kidney injury in pediatric critical care
Intensive Care Medicine – Paediatric and Neonatal (2025)
-
Expanded discussion of kidney health monitoring for critically ill term and late preterm infants after acute kidney injury: a report from the Neonatal Kidney Health Consensus Workshop
Pediatric Nephrology (2025)