Abstract
Background
Continuous heart rate (HR) and oxygenation (SpO2) metrics can be useful for predicting adverse events in very low birth weight (VLBW) infants. To optimize the utility of these tools, inter-site variability must be taken into account.
Methods
For VLBW infants at three neonatal intensive care units (NICUs), we analyzed the mean, standard deviation, skewness, kurtosis, and cross-correlation of electrocardiogram HR, pulse oximeter pulse rate, and SpO2. The number and durations of bradycardia and desaturation events were also measured. Twenty-two metrics were calculated hourly, and mean daily values were compared between sites.
Results
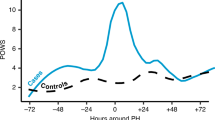
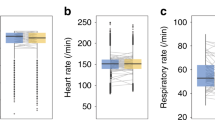
We analyzed data from 1168 VLBW infants from birth through day 42 (35,238 infant-days). HR and SpO2 metrics were similar at the three NICUs, with mean HR rising by ~10 beats/min over the first 2 weeks and mean SpO2 remaining stable ~94% over time. The number of bradycardia events was higher at one site, and the duration of desaturations was longer at another site.
Conclusions
Mean HR and SpO2 were generally similar among VLBW infants at three NICUs from birth through 6 weeks of age, but bradycardia and desaturation events differed in the first 2 weeks after birth. This highlights the importance of developing predictive analytics tools at multiple sites.
Impact
-
HR and SpO2 analytics can be useful for predicting adverse events in VLBW infants in the NICU, but inter-site differences must be taken into account in developing predictive algorithms.
-
Although mean HR and SpO2 patterns were similar in VLBW infants at three NICUs, inter-site differences in the number of bradycardia events and duration of desaturation events were found.
-
Inter-site differences in bradycardia and desaturation events among VLBW infants should be considered in the development of predictive algorithms.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Data and Code
Summary data and code are available on UVA Dataverse at https://doi.org/10.18130/V3/7UAPHU.
Change history
14 July 2021
A Correction to this paper has been published: https://doi.org/10.1038/s41390-021-01621-4
References
Kumar, N., Akangire, G., Sullivan, B., Fairchild, K. & Sampath, V. Continuous vital sign analysis for predicting and preventing neonatal diseases in the twenty-first century: big data to the forefront. Pediatr. Res. https://doi.org/10.1038/s41390-019-0527-0 (2019).
Joshi, R. et al. Predicting neonatal sepsis using features of heart rate variability, respiratory characteristics, and ECG-derived estimates of infant motion. IEEE J. Biomed. Heal. Inform. 24, 681–692 (2020).
Dewhurst, C. J., Cooke, R. W. I. & Turner, M. A. Clinician observation of physiological trend monitoring to identify late-onset sepsis in preterm infants. Acta Paediatr. Int. J. Paediatr. 97, 1187–1191 (2008).
Mithal, L. B. et al. Vital signs analysis algorithm detects inflammatory response in premature infants with late onset sepsis and necrotizing enterocolitis. Early Hum. Dev. 117, 83–89 (2018).
Sullivan, B. A. & Fairchild, K. D. Predictive monitoring for sepsis and necrotizing enterocolitis to prevent shock. Semin. Fetal Neonatal Med. 20, 255–261 (2015).
Griffin, M. P., Moorman, J. R., Todd, J., Workman-Daniels, K. & Goldmann, D. Toward the early diagnosis of neonatal sepsis and sepsis-like illness using novel heart rate analysis. Pediatrics 107, 97–104 (2001).
Griffin, M. P. et al. Abnormal heart rate characteristics preceding neonatal sepsis and sepsis-like illness. Pediatr. Res. 53, 920–926 (2003).
Griffin, M. P. et al. Heart rate characteristics: novel physiomarkers to predict neonatal infection and death. Pediatrics 116, 1070–1074 (2005).
Weitkamp, J. H. et al. Meningitis, urinary tract, and bloodstream infections in very low birth weight infants enrolled in a heart rate characteristics monitoring trial. Pediatr. Res. 87, 1226–1230 (2020).
Moorman, J. R. et al. Mortality reduction by heart rate characteristic monitoring in very low birth weight neonates: a randomized trial. J. Pediatr. 159, 900–907 (2011).
Lee, H. et al. A new algorithm for detecting central apnea in neonates. Physiol. Meas. 33, 1–17 (2012).
Clark, M. T. et al. Breath-by-breath analysis of cardiorespiratory interaction for quantifying developmental maturity in premature infants. J. Appl. Physiol. 112, 859–867 (2012).
Fairchild, K. D. & Lake, D. E. Cross-correlation of heart rate and oxygen saturation in very low birthweight infants: association with apnea and adverse events. Am. J. Perinatol. 35, 463–469 (2018).
Fairchild, K. D. et al. Vital signs and their cross-correlation in sepsis and NEC:a study of 1,065 very-low-birth-weight infants in two NICUs. Pediatr. Res. 81, 315–321 (2017).
Martin, R. J., DiFiore, J. M., Macfarlane, P. M. & Wilson, C. G. Physiologic basis for intermittent hypoxic episodes in preterm infants. Adv. Exp. Med. Biol. 758, 351–358 (2012).
Bancalari, E. & Claure, N. Respiratory instability and hypoxemia episodes in preterm infants. Am. J. Perinatol. 35, 534–536 (2018).
McDonald, F. B., Dempsey, E. M. & O’Halloran, K. D. The impact of preterm adversity on cardiorespiratory function. Exp. Physiol. 105, 17–43 (2020).
Nagraj, V. P., Sinkin, R. A., Lake, D. E., Randall Moorman, J. & Fairchild, K. D. Recovery from bradycardia and desaturation events at 32 weeks corrected age and NICU length of stay: an indicator of physiologic resilience? Pediatr. Res. https://doi.org/10.1038/s41390-019-0488-3 (2019).
Fairchild, K. D., Nagraj, V. P., Sullivan, B. A., Moorman, J. R. & Lake, D. E. Oxygen desaturations in the early neonatal period predict development of bronchopulmonary dysplasia. Pediatr. Res. https://doi.org/10.1038/s41390-018-0223-5 (2018).
Sullivan, B. A. et al. Early pulse oximetry data improves prediction of death and adverse outcomes in a two-center cohort of very low birth weight infants. Am. J. Perinatol. https://doi.org/10.1055/s-0038-1654712 (2018).
Vesoulis, Z. A. et al. Early hypoxemia burden is strongly associated with severe intracranial hemorrhage in preterm infants. J. Perinatol. 39, 48–53 (2019).
Searle, S. R., Speed, F. M. & Milliken, G. A. Population marginal means in the linear model: an alternative to least squares means. Am. Stat. 34, 216–221 (1980).
Fleming, S. et al. Normal ranges of heart rate and respiratory rate in children from birth to 18 years of age: a systematic review of observational studies. Lancet 377, 1011–1018 (2011).
Alonzo, C. J. et al. Heart rate ranges in premature neonates using high resolution physiologic data. J. Perinatol. 38, 1242–1245 (2018).
Van Marter, L. J. et al. Do clinical markers of barotrauma and oxygen toxicity explain interhospital variation in rates of chronic lung disease? The Neonatology Committee for the Developmental Network. Pediatrics 105, 1194–1201 (2000).
Fairchild, K. et al. Clinical associations of immature breathing in preterm infants: part 1-central apnea. Pediatr. Res. 80, 21–27 (2016).
March Of Dimes. Infant mortality rates St. Louis city. PeriStats. https://www.marchofdimes.org/Peristats/ViewSubtopic.aspx?reg=29510&top=6&stop=91&lev=1&slev=5&obj=9.
March Of Dimes. Infant mortality rates Virginia. PeriStats. https://www.marchofdimes.org/Peristats/ViewSubtopic.aspx?reg=51&top=6&stop=91&lev=1&slev=4&obj=9.
March Of Dimes. Infant mortality rates Manhattan. PeriStats. https://www.marchofdimes.org/Peristats/ViewSubtopic.aspx?reg=36061&dv=rdo&top=6&stop=91&lev=1&slev=6&eny=&sty=&chy=&obj=8.
Dennery, P. A. et al. Pre-Vent: the prematurity-related ventilatory control study. Pediatr. Res. 85, 769–776 (2019).
Ransohoff, D. F. & Feinstein, A. R. Problems of spectrum and bias in evaluating the efficacy of diagnostic tests. N. Engl. J. Med. 299, 926–930 (1978).
Reyna, M. A. et al. Early prediction of sepsis from clinical data. Crit. Care Med. 48, 210–217 (2020).
Acknowledgements
This work was supported by HHS|NIH|Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) R01 HD072071 and K23 HD097254-01. HHS|NIH|National Institute of Neurological Disorders and Stroke (NINDS) K23 NS111086.
Author information
Authors and Affiliations
Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data, and drafting the article or revising it critically for important intellectual content. All authors gave final approval of the version to be published.
Corresponding author
Ethics declarations
Competing interests
J.R.M. and D.E.L. have equity shares in Medical Predictive Science Corporation, Charlottesville, VA. J.R.M. is an officer and owns equity in Advanced Medical Predictive Devices, Diagnostics, and Displays. S.J.R. has received consulting fees from Airway Therapeutics. The other authors declare no competing interests.
Patient consent
Institutional Review Boards at each site approved the study with waiver of consent.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: In the Discussion section paragraph four, first sentence was changed and a Data and Code section was added.
Supplementary information
Rights and permissions
About this article
Cite this article
Zimmet, A.M., Sullivan, B.A., Fairchild, K.D. et al. Vital sign metrics of VLBW infants in three NICUs: implications for predictive algorithms. Pediatr Res 90, 125–130 (2021). https://doi.org/10.1038/s41390-021-01428-3
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-021-01428-3
This article is cited by
-
Car seat tolerance screen failure in the neonatal intensive care unit: clinical, oxygen saturation and heart rate analysis
Pediatric Research (2025)
-
Early prediction of severe retinopathy of prematurity requiring laser treatment using physiological data
Pediatric Research (2023)
-
Cardiorespiratory signature of neonatal sepsis: development and validation of prediction models in 3 NICUs
Pediatric Research (2023)
-
Discovery of signatures of fatal neonatal illness in vital signs using highly comparative time-series analysis
npj Digital Medicine (2022)
-
The Impact of Dexmedetomidine Initiation on Cardiovascular Status and Oxygenation in Critically ill Neonates
Pediatric Cardiology (2022)