Abstract
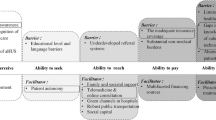
Most individuals with autism spectrum disorder (ASD)—a complex, life-long developmental disorder—do not have access to the care required to address their diverse health needs. Here, we review: (1) common barriers to healthcare access (shortage/cost of services; physician awareness; stigma); (2) barriers encountered primarily during childhood (limited screening/diagnosis; unclear referral pathways), transition to adulthood (insufficient healthcare transition services; suboptimal physician awareness of healthcare needs) and adulthood (shortage of services/limited insurance; communication difficulties with physicians; limited awareness of healthcare needs of aging adults); and (3) advances in research/program development for better healthcare access. A robust understanding of barriers to accessing healthcare across the lifespan of autistic individuals is critical to ensuring the best use of healthcare resources to improve social, physical, and mental health outcomes. Stakeholders must strengthen healthcare service provision by coming together to: better understand healthcare needs of underserved populations; strengthen medical training on care of autistic individuals; increase public awareness of ASD; promote research into/uptake of tools for ASD screening, diagnosis, and treatment; understand specific healthcare needs of autistic individuals in lower resource countries; and conduct longitudinal studies to understand the lifetime health, social, and economic impacts of ASD and enable the evaluation of novel approaches to increasing healthcare access.
Impact
-
Despite the growing body of evidence, our understanding of barriers to healthcare encountered by individuals with ASD remains limited, particularly beyond childhood and in lower resource countries.
-
We describe current and emerging barriers to healthcare access encountered by individuals with ASD across the lifespan.
-
We recommend that stakeholders develop evidence-informed policies, programs, and technologies that address barriers to healthcare access for individuals with ASD and consider broad, equitable implementation to maximize impact.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders 5th edn (American Psychiatric Association, 2013).
Elsabbagh, M. et al. Global prevalence of autism and other pervasive developmental disorders. Autism Res. 5, 160–179 (2012).
Buescher, A. V. S., Cidav, Z., Knapp, M. & Mandell, D. S. Costs of autism spectrum disorders in the United Kingdom and the United States. JAMA Pediatr. 168, 721–728 (2014).
Knapp, M., Romeo, R. & Beecham, J. Economic cost of autism in the UK. Autism 13, 317–336 (2009).
Markowitz, L. A. et al. Development and psychometric evaluation of a psychosocial quality-of-life questionnaire for individuals with autism and related developmental disorders. Autism 20, 832–844 (2016).
Brookman-Frazee, L., Stadnick, N., Chlebowski, C., Baker-Ericzén, M. & Ganger, W. Characterizing psychiatric comorbidity in children with autism spectrum disorder receiving publicly funded mental health services. Autism 22, 938–952 (2018).
Davignon, M. N., Qian, Y., Massolo, M. & Croen, L. A. Psychiatric and medical conditions in transition-aged individuals with ASD. Pediatrics 141, S335–S345 (2018).
Vohra, R., Madhavan, S. & Sambamoorthi, U. Comorbidity prevalence, healthcare utilization, and expenditures of Medicaid enrolled adults with autism spectrum disorders. Autism 21, 995–1009 (2017).
Antezana, L., Scarpa, A., Valdespino, A., Albright, J. & Richey, J. A. Rural trends in diagnosis and services for autism spectrum disorder. Front. Psychol. 8, 590 (2017).
Thomas, K. C., Ellis, A. R., McLaurin, C., Daniels, J. & Morrissey, J. P. Access to care for autism-related services. J. Autism Dev. Disord. 37, 1902–1912 (2007).
American Psychological Association. Education and Socioeconomic Status (American Psychological Association, 2019).
American Board of Pediatrics. Pediatric Physicians Workforce Data Book, 2018–2019 (American Board of Pediatrics, 2019).
American Academy of Child and Adolescent Psychiatry. Workforce Maps by State: Practicing Child and Adolescent Psychiatrists (American Academy of Child and Adolescent Psychiatry, 2019).
Elder, J. H., Brasher, S. & Alexander, B. Identifying the Barriers to early diagnosis and treatment in underserved individuals with autism spectrum disorders (ASD) and their families: a qualitative study. Issues Ment. Health Nurs. 37, 412–420 (2016).
Raymaker, D. M. et al. Barriers to healthcare: Instrument development and comparison between autistic adults and adults with and without other disabilities. Autism 21, 972–984 (2017).
Dudley, K. M., Klinger, M. R., Meyer, A., Powell, P. & Klinger, L. G. Understanding service usage and needs for adults with ASD: the importance of living situation. J. Autism Dev. Disord. 49, 556–568 (2019).
Mazurek, M. O., Curran, A., Burnette, C. & Sohl, K. ECHO autism STAT: accelerating early access to autism diagnosis. J. Autism Dev. Disord. 49, 127–137 (2019).
Juárez, A. P. et al. Early identification of ASD through telemedicine: potential value for underserved populations. J. Autism Dev. Disord. 48, 2601–2610 (2018).
Kuhlthau, K. A. et al. Health care transition services for youth with autism spectrum disorders: perspectives of caregivers. Pediatrics 137(Suppl. 2), S158–S166 (2016).
Nicolaidis, C. et al. “Respect the way I need to communicate with you”: healthcare experiences of adults on the autism spectrum. Autism 19, 824–831 (2015).
Austriaco, K., Aban, I., Willig, J. & Kong, M. Contemporary trainee knowledge of autism: how prepared are our future providers? Front. Pediatr. 7, 165 (2019).
Unigwe, S. et al. GPs’ confidence in caring for their patients on the autism spectrum: an online self-report study. Br. J. Gen. Pract. 67, e445–e452 (2017).
Muskat, B. et al. Autism comes to the hospital: the experiences of patients with autism spectrum disorder, their parents and health-care providers at two Canadian paediatric hospitals. Autism 19, 482–490 (2015).
Saqr, Y., Braun, E., Porter, K., Barnette, D. & Hanks, C. Addressing medical needs of adolescents and adults with autism spectrum disorders in a primary care setting. Autism 22, 51–61 (2018).
Bradshaw, P., Pellicano, E., van Driel, M. & Urbanowicz, A. How can we support the healthcare needs of autistic adults without intellectual disability? Curr. Dev. Disord. Rep. 6, 45–56 (2019).
Mason, D. et al. A systematic review of what barriers and facilitators prevent and enable physical healthcare services access for autistic adults. J. Autism Dev. Disord. 49, 3387–3400 (2019).
Doherty, A. J. et al. Barriers and facilitators to primary health care for people with intellectual disabilities and/or autism: an integrative review. BJGP Open 4, bjgpopen20X101030 (2020).
Sohl, K., Mazurek, M. O. & Brown, R. ECHO Autism: using technology and mentorship to bridge gaps, increase access to care, and bring best practice autism care to primary care. Clin. Pediatr. 56, 509–511 (2017).
Nicolaidis, C. et al. The development and evaluation of an online healthcare toolkit for autistic adults and their primary care providers. J. Gen. Intern. Med. 31, 1180–1189 (2016).
Pickard, K. E. & Ingersoll, B. R. Quality versus quantity: the role of socioeconomic status on parent-reported service knowledge, service use, unmet service needs, and barriers to service use. Autism 20, 106–115 (2016).
Barry, C. L. et al. Effects of state insurance mandates on health care use and spending for autism spectrum disorder. Health Aff. 36, 1754–1761 (2017).
Mandell, D. S. et al. Effects of autism spectrum disorder insurance mandates on the treated prevalence of autism spectrum disorder. JAMA Pediatr. 170, 887–893 (2016).
Herlihy, L., Knoch, K., Vibert, B. & Fein, D. Parents’ first concerns about toddlers with autism spectrum disorder: effect of sibling status. Autism 19, 20–28 (2015).
Salomone, E. et al. Development of the WHO caregiver skills training program for developmental disorders or delays. Front. Psychiatry 10, 769 (2019).
Zhou, B. et al. Effects of Parent-Implemented Early Start Denver model intervention on Chinese toddlers with autism spectrum disorder: a non-randomized controlled trial. Autism Res. 11, 654–666 (2018).
Fox, F., Aabe, N., Turner, K., Redwood, S. & Rai, D. “It was like walking without knowing where I was going”: a qualitative study of autism in a UK Somali migrant community. J. Autism Dev. Disord. 47, 305–315 (2017).
Kairys, S. W. & Petrova, A. Role of participation of pediatricians in the “Activated Autism Practice” program in practicing children with autism spectrum disorders at the primary care setting. Glob. Pediatr. Health 3, 2333794X16663544 (2016).
Khanlou, N. et al. Access barriers to services by immigrant mothers of children with autism in Canada. Int. J. Ment. Health Addict. 15, 239–259 (2017).
Autism Speaks. Autism speaks non-English resources. https://www.autismspeaks.org/non-english-resources (2021).
University Southern California. Autism fact sheets. http://www.uscucedd.org/publications-resources/autism-pubs/autism-fact-sheets (2011).
Kinnear, S. H., Link, B. G., Ballan, M. S. & Fischbach, R. L. Understanding the experience of stigma for parents of children with autism spectrum disorder and the role stigma plays in families’ lives. J. Autism Dev. Disord. 46, 942–953 (2016).
Vogan, V., Lake, J. K., Tint, A., Weiss, J. A. & Lunsky, Y. Tracking health care service use and the experiences of adults with autism spectrum disorder without intellectual disability: a longitudinal study of service rates, barriers and satisfaction. Disabil. Health J. 10, 264–270 (2017).
Pasha, S. B., Qadir, T. F., Fatima, H. & Hussain, S. A. Sesame Street’s recognition of autism. Lancet Psychiatry 4, 520–521 (2017).
Anthony, B. J. et al. Increasing autism acceptance: the impact of the Sesame Street “See Amazing in All Children” initiative. Autism 24, 95–108 (2020).
Ip, A., Zwaigenbaum, L. & Brian, J. A. Post-diagnostic management and follow-up care for autism spectrum disorder. Paediatr. Child Health 24, 461–468 (2019).
World Health Organization. Autism spectrum disorders. https://www.who.int/news-room/fact-sheets/detail/autism-spectrum-disorders (2019).
Hyman, S. L., Levy, S. E., Myers, S. M., Council on Children with Disabilities, Section on Developmental and Behavioral Pediatrics. Identification, evaluation, and management of children with autism spectrum disorder. Pediatrics 145, e20193447 (2020).
National Institute for Health and Care Excellence. Autism. https://www.nice.org.uk/guidance/qs51/resources/autism-pdf-2098722137029 (2014).
Barthélémy, C., Fuentes, J., Howlin, P. & Jan van der Gaag, R. People with Autism Spectrum Disorder. Identification, Understanding, Intervention 3rd edn (Autism Europe, 2019).
Weitlauf, A. S., Gotham, K. O., Vehorn, A. C. & Warren, Z. E. Brief report: DSM-5 “levels of support”: a comment on discrepant conceptualizations of severity in ASD. J. Autism Dev. Disord. 44, 471–476 (2014).
Lord, C. et al. Autism spectrum disorder. Nat. Rev. Dis. Prim. 6, 5 (2020).
Happé, F. G. et al. Demographic and cognitive profile of individuals seeking a diagnosis of autism spectrum disorder in adulthood. J. Autism Dev. Disord. 46, 3469–3480 (2016).
World Health Organization. Comprehensive and Coordinated Efforts for the Management of Autism Spectrum Disorders, Sixty-Seventh World Health Assembly (World Health Organization, 2014).
Rutherford, M. et al. Gender ratio in a clinical population sample, age of diagnosis and duration of assessment in children and adults with autism spectrum disorder. Autism 20, 628–634 (2016).
Giarelli, E. et al. Sex differences in the evaluation and diagnosis of autism spectrum disorders among children. Disabil. Health J. 3, 107–116 (2010).
Guinchat, V. et al. Very early signs of autism reported by parents include many concerns not specific to autism criteria. Res. Autism Spectr. Disord. 6, 589–601 (2012).
Pierce, K. et al. Evaluation of the diagnostic stability of the early autism spectrum disorder phenotype in the general population starting at 12 months. JAMA Pediatr. 173, 578–587 (2019).
Maenner, M. J. et al. Prevalence of autism spectrum disorder among children aged 8 years - autism and developmental disabilities monitoring network, 11 sites, United States, 2016. MMWR Surveill. Summ. 69, 1–12 (2020).
Salomone, E., Charman, T., McConachie, H. & Warreyn, P. Child’s verbal ability and gender are associated with age at diagnosis in a sample of young children with ASD in Europe. Child Care Health Dev. 42, 141–145 (2016).
Public Health Agency of Canada. Autism spectrum disorder among children and youth in Canada. https://www.canada.ca/en/public-health/services/publications/diseases-conditions/autism-spectrum-disorder-children-youth-canada-2018.html (2018).
Clark, M. L. E., Vinen, Z., Barbaro, J. & Dissanayake, C. School age outcomes of children diagnosed early and later with autism spectrum disorder. J. Autism Dev. Disord. 48, 92–102 (2018).
Dawson, G. et al. Randomized, controlled trial of an intervention for toddlers with autism: the Early Start Denver Model. Pediatrics 125, e17–e23 (2010).
Zuckerman, K., Lindly, O. J. & Chavez, A. E. Timeliness of autism spectrum disorder diagnosis and use of services among U.S. elementary school-aged children. Psychiatr. Serv. 68, 33–40 (2017).
American Academy of Pediatrics. Initial medical evaluation of a child diagnosed with an autism spectrum disorder. https://www.aap.org/en-us/Documents/cocd_fact_sheet_initialmedicine.pdf (2013).
Canadian Paediatric Society. Standards of diagnostic assessment for autism spectrum disorder. https://www.cps.ca/en/documents/position/asd-diagnostic-assessment#ref24 (2019).
Schaefer, G. B. & Mendelsohn, N. J., Professional Practice and Guidelines Committee. Clinical genetics evaluation in identifying the etiology of autism spectrum disorders: 2013 guideline revisions. Genet. Med. 15, 399–407 (2013).
Barton, K. S. et al. Pathways from autism spectrum disorder diagnosis to genetic testing. Genet. Med. 20, 737–744 (2018).
Shattuck, P. T. et al. Services for adults with an autism spectrum disorder. Can. J. Psychiatry 57, 284–291 (2012).
Shea, L. L. et al. Brief report: service use and associated expenditures among adolescents with autism spectrum disorder transitioning to adulthood. J. Autism Dev. Disord. 48, 3223–3227 (2018).
Weiss, J. A. et al. Health concerns and health service utilization in a population cohort of young adults with autism spectrum disorder. J. Autism Dev. Disord. 48, 36–44 (2018).
Bennett, A. E., Miller, J. S., Stollon, N., Prasad, R. & Blum, N. J. Autism spectrum disorder and transition-aged youth. Curr. Psychiatry Rep. 20, 103 (2018).
Crane, L., Adams, F., Harper, G., Welch, J. & Pellicano, E. “Something needs to change”: mental health experiences of young autistic adults in England. Autism 23, 477–493 (2019).
Cheak-Zamora, N. C., Yang, X., Farmer, J. E. & Clark, M. Disparities in transition planning for youth with autism spectrum disorder. Pediatrics 131, 447–454 (2013).
Rast, J. E., Shattuck, P. T., Roux, A. M., Anderson, K. A. & Kuo, A. The medical home and health care transition for youth with autism. Pediatrics 141, S328–S334 (2018).
Nathenson, R. A. & Zablotsky, B. The transition to the adult health care system among youths with autism spectrum disorder. Psychiatr. Serv. 68, 735–738 (2017).
Autism Community, Newfoundland Labrador. Report: needs assessment survey. https://www.autism.nf.net/wp-content/uploads/2017/03/Needs-Assesment-2015.pdf (2015).
Cheak-Zamora, N. C. & Teti, M. “You think it’s hard now … It gets much harder for our children”: youth with autism and their caregiver’s perspectives of health care transition services. Autism 19, 992–1001 (2015).
Kuhlthau, K. A., Warfield, M. E., Hurson, J., Delahaye, J. & Crossman, M. K. Pediatric provider’s perspectives on the transition to adult health care for youth with autism spectrum disorder: current strategies and promising new directions. Autism 19, 262–271 (2015).
Mazurek, M. O. et al. ECHO Autism Transition: enhancing healthcare for adolescents and young adults with autism spectrum disorder. Autism 24, 633–644 (2020).
Dietz, P. M., Rose, C. E., McArthur, D. & Maenner M. National and state estimates of adults with autism spectrum disorder. J. Autism Dev. Disord. 50, 4258–4266 (2020).
Croen, L. A. et al. The health status of adults on the autism spectrum. Autism 19, 814–823 (2015).
Hand, B. N., Angell, A. M., Harris, L. & Carpenter, L. A. Prevalence of physical and mental health conditions in Medicare-enrolled, autistic older adults. Autism 24, 755–764 (2020).
Hirvikoski, T. et al. Premature mortality in autism spectrum disorder. Br. J. Psychiatry 208, 232–238 (2016).
Benevides, T. W. et al. Interventions to address health outcomes among autistic adults: a systematic review. Autism 1362361320913664 (2020).
Warfield, M. E., Crossman, M. K., Delahaye, J., Der Weerd, E. & Kuhlthau, K. A. Physician perspectives on providing primary medical care to adults with autism spectrum disorders (ASD). J. Autism Dev. Disord. 45, 2209–2217 (2015).
Autism Canada. Aging and autism: a think tank round table. https://autismcanada.org/research/scientific-symposium/ (2017).
Camm-Crosbie, L., Bradley, L., Shaw, R., Baron-Cohen, S. & Cassidy, S. ‘People like me don’t get support’: autistic adults’ experiences of support and treatment for mental health difficulties, self-injury and suicidality. Autism 23, 1431–1441 (2019).
Maddox, B. B. & Gaus, V. L. Community mental health services for autistic adults: good news and bad news. Autism Adulthood 1, 15–19 (2019).
Bruder, M. B., Kerins, G., Mazzarella, C., Sims, J. & Stein, N. Brief report: the medical care of adults with autism spectrum disorders: identifying the needs. J. Autism Dev. Disord. 42, 2498–2504 (2012).
Zerbo, O., Massolo, M. L., Qian, Y. & Croen, L. A. A study of physician knowledge and experience with autism in adults in a large integrated healthcare system. J. Autism Dev. Disord. 45, 4002–4014 (2015).
Nicolaidis, C. et al. Comparison of healthcare experiences in autistic and non-autistic adults: a cross-sectional online survey facilitated by an academic-community partnership. J. Gen. Intern. Med. 28, 761–769 (2013).
Zerbo, O. et al. Health care service utilization and cost among adults with autism spectrum disorders in a U.S. Integrated Health Care System. Autism Adulthood 1, 27–36 (2019).
Roestorf, A. et al. “Older Adults with ASD: The Consequences of Aging”. Insights from a series of special interest group meetings held at the International Society for Autism Research 2016–2017. Res. Autism Spectr. Disord. 63, 3–12 (2019).
Altay, M. A. Family physicians’ awareness of autism spectrum disorder: results from a survey study. Open Access Maced. J. Med. Sci. 7, 967–972 (2019).
de Vries, P. J. Thinking globally to meet local needs: autism spectrum disorders in Africa and other low-resource environments. Curr. Opin. Neurol. 29, 130–136 (2016).
Rahbar, M. H., Ibrahim, K. & Assassi, P. Knowledge and attitude of general practitioners regarding autism in Karachi, Pakistan. J. Autism Dev. Disord. 41, 465–474 (2011).
Mahapatra, P. et al. Parental care-seeking pathway and challenges for autistic spectrum disorders children: a mixed method study from Bhubaneswar, Odisha. Indian J. Psychiatry 61, 37–44 (2019).
Tekola, B. et al. Adapting and pre-testing the World Health Organization’s Caregiver Skills Training programme for autism and other developmental disorders in a very low-resource setting: findings from Ethiopia. Autism 24, 51–63 (2020).
Divan, G. et al. The feasibility and effectiveness of PASS Plus, a lay health worker delivered comprehensive intervention for autism spectrum disorders: Pilot RCT in a rural low and middle income country setting. Autism Res. 12, 328–339 (2019).
Bai, D. et al. Association of genetic and environmental factors with autism in a 5-Country Cohort. JAMA Psychiatry 76, 1035–1043 (2019).
Srivastava, S. et al. Meta-analysis and multidisciplinary consensus statement: exome sequencing is a first-tier clinical diagnostic test for individuals with neurodevelopmental disorders. Genet. Med. 21, 2413–2421 (2019).
Feliciano, P. et al. Exome sequencing of 457 autism families recruited online provides evidence for autism risk genes. NPJ Genom. Med. 4, 19 (2019).
Tarailo-Graovac, M. et al. Exome sequencing and the management of neurometabolic disorders. N. Engl. J. Med. 374, 2246–2255 (2016).
Wolff, M. et al. Genetic and phenotypic heterogeneity suggest therapeutic implications in SCN2A-related disorders. Brain 140, 1316–1336 (2017).
Frazier, T. W. et al. Molecular and phenotypic abnormalities in individuals with germline heterozygous PTEN mutations and autism. Mol. Psychiatry 20, 1132–1138 (2015).
Frazier, T. W. Autism spectrum disorder associated with germline heterozygous PTEN mutations. Cold Spring Harb. Perspect. Med. 9, a037002 (2019).
Beversdorf, D. Q. Missouri Autism Summit Consortium. Phenotyping, etiological factors, and biomarkers: toward precision medicine in autism spectrum disorders. J. Dev. Behav. Pediatr. 37, 659–673 (2016).
The University of British Columbia. iTARGET Autism Initiative (individualized Treatments for Autism Recovery using Genetic-Environmental Targets). http://www.itargetautism.ca/ (2017).
Shea, L., Newschaffer, C. J., Xie, M., Myers, S. M. & Mandell, D. S. Genetic testing and genetic counseling among Medicaid-enrolled children with autism spectrum disorder in 2001 and 2007. Hum. Genet. 133, 111–116 (2014).
Karpur, A., Lello, A., Frazier, T., Dixon, P. J. & Shih, A. J. Health disparities among children with autism spectrum disorders: analysis of the National Survey of Children’s Health 2016. J. Autism Dev. Disord. 49, 1652–1664 (2019).
WHO. WHO mental health quality rights initiative. https://www.who.int/mental_health/policy/quality_rights/QRs_flyer_eng_2017.pdf?ua=1 (2017).
Ozonoff, S. et al. Recurrence risk for autism spectrum disorders: a Baby Siblings Research Consortium study. Pediatrics 128, e488–e495 (2011).
Frazier, T. W. et al. Brief report: a survey of autism research priorities across a diverse community of stakeholders. J. Autism Dev. Disord. 48, 3965–3971 (2018).
Hudry, K., Pellicano, E., Uljarević, M. & Whitehouse, A. J. O. Setting the research agenda to secure the wellbeing of autistic people. Lancet Neurol. 19, 374–376 (2020).
Acknowledgements
This work was partially sponsored by F. Hoffman-La Roche Ltd. Shift Health consults with organizations across the health and life sciences sector, including F. Hoffman-La Roche Ltd. Authors from Shift Health (R.E.W., A.E.M., N.M.-S., A.S., H.L.) were employed under contract with Hoffman-La Roche Ltd for the purpose of this work. Authors not employed by Shift Health (S.L., J.F., T.W.F.) did not receive support or remuneration related to this work. S.L. is supported by an IGAP salary award from the BC Children’s Hospital Research Institute, and is an invited contributor on behalf of Autism Canada. The sponsor (F. Hoffman-La Roche Ltd) did not have a role in the: design and conduct of the literature review; synthesis and analysis of evidence; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
N.M.-S., H.L., A.E.M., and A.S. conceptualized and designed the study, collected the data (e.g., papers reviewed), drafted the initial manuscript, and reviewed and revised the manuscript. R.E.W., S.L., J.F., and T.W.F. conceptualized and designed the study, reviewed. and revised the manuscript. All authors approved the final manuscript as submitted for publication.
Corresponding author
Ethics declarations
Competing interests
T.W.F. has received funding or research support from, acted as a consultant to, received travel support from, and/or received a speaker’s honorarium from Quadrant Biosciences, Impel NeuroPharma, F. Hoffmann-La Roche AG Pharmaceuticals, the Cole Family Research Fund, Simons Foundation, Ingalls Foundation, Forest Laboratories, Ecoeos, IntegraGen, Kugona LLC, Shire Development, Bristol-Myers Squibb, Roche Pharma, National Institutes of Health, and the Brain and Behavior Research Foundation and has an investor stake in Autism EYES LLC. J.F. has received research support from Policlinica Gipuzkoa Foundation (PGF), Servier, and AIMS-2 Trials/Project ID 777394. He has received partial support for professional meetings attendance from PGF, ESCAP & AACAP.
Patient consent
Not required for this study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Malik-Soni, N., Shaker, A., Luck, H. et al. Tackling healthcare access barriers for individuals with autism from diagnosis to adulthood. Pediatr Res 91, 1028–1035 (2022). https://doi.org/10.1038/s41390-021-01465-y
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-021-01465-y
This article is cited by
-
Longitudinal multi-omics analysis of umbilical cord blood and childhood serum in Autism
Molecular Psychiatry (2026)
-
Self-harm and suicidality experiences of autistic and non-autistic adults in midlife and old age
Molecular Autism (2025)
-
Access to services for autistic people across Europe
Molecular Autism (2025)
-
Medical management and differential diagnosis of restrictive eating disorders in men: a case study report with co-produced recommendations
Journal of Eating Disorders (2025)
-
Pharmacological treatment in autism: a proposal for guidelines on common co-occurring psychiatric symptoms
BMC Medicine (2025)