Abstract
Background
The impact of the permissive hypotension approach in clinically well infants on regional cerebral oxygen saturation (rScO2) and autoregulatory capacity (CAR) remains unknown.
Methods
Prospective cohort study of blinded rScO2 measurements within a randomized controlled trial of management of hypotension (HIP trial) in extremely preterm infants. rScO2, mean arterial blood pressure, duration of cerebral hypoxia, and transfer function (TF) gain inversely proportional to CAR, were compared between hypotensive infants randomized to receive dopamine or placebo and between hypotensive and non-hypotensive infants, and related to early intraventricular hemorrhage or death.
Results
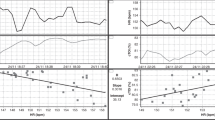
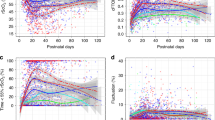
In 89 potentially eligible HIP trial patients with rScO2 measurements, the duration of cerebral hypoxia was significantly higher in 36 hypotensive compared to 53 non-hypotensive infants. In 29/36 hypotensive infants (mean GA 25 weeks, 69% males) receiving the study drug, no significant difference in rScO2 was observed after dopamine (n = 13) compared to placebo (n = 16). Duration of cerebral hypoxia was associated with early intraventricular hemorrhage or death.
Calculated TF gain (n = 49/89) was significantly higher reflecting decreased CAR in 16 hypotensive compared to 33 non-hypotensive infants.
Conclusions
Dopamine had no effect on rScO2 compared to placebo in hypotensive infants. Hypotension and cerebral hypoxia are associated with early intraventricular hemorrhage or death.
Impact
-
Treatment of hypotension with dopamine in extremely preterm infants increases mean arterial blood pressure, but does not improve cerebral oxygenation.
-
Hypotensive extremely preterm infants have increased duration of cerebral hypoxia and reduced cerebral autoregulatory capacity compared to non-hypotensive infants.
-
Duration of cerebral hypoxia and hypotension are associated with early intraventricular hemorrhage or death in extremely preterm infants.
-
Since systematic treatment of hypotension may not be associated with better outcomes, the diagnosis of cerebral hypoxia in hypotensive extremely preterm infants might guide treatment.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Adams-Chapman, I. et al. Neurodevelopmental impairment among extremely preterm infants in the neonatal research network. Pediatrics 141, e20173091 (2018).
Blencowe, H. et al. National, regional, and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: a systematic analysis and implications. Lancet 379, 2162–2172 (2012).
Levene, M. Development of audit measures and guidelines for good practice in the management of neonatal respiratory distress syndrome. Report of a Joint Working Group of the British Association of Perinatal Medicine and the Research Unit of the Royal College of Physicians. Arch. Dis. Child 67, 1221–1227 (1992).
Munro, M. J., Walker, A. M. & Barfield, C. P. Hypotensive extremely low birth weight infants have reduced cerebral blood flow. Pediatrics 114, 1591–1596 (2004).
Borch, K., Lou, H. C. & Greisen, G. Cerebral white matter blood flow and arterial blood pressure in preterm infants. Acta Paediatr. 99, 1489–1492 (2010).
Miall-Allen, V. M., de Vries, L. S. & Whitelaw, A. G. Mean arterial blood pressure and neonatal cerebral lesions. Arch. Dis. Child 62, 1068–1069 (1987).
Tsuji, M. et al. Cerebral intravascular oxygenation correlates with mean arterial pressure in critically ill premature infants. Pediatrics 106, 625–632 (2000).
Wong, F. Y. et al. Impaired autoregulation in preterm infants identified by using spatially resolved spectroscopy. Pediatrics 121, e604–e611 (2008).
Batton, B. et al. Blood pressure, anti-hypotensive therapy, and neurodevelopment in extremely preterm infants. J. Pediatr. 154, 351–357 (2009). e351.
Sassano-Higgins, S., Friedlich, P. & Seri, I. A meta-analysis of dopamine use in hypotensive preterm infants: blood pressure and cerebral hemodynamics. J. Perinatol. 31, 647–655 (2011).
Eriksen, V. R., Hahn, G. H. & Greisen, G. Dopamine therapy is associated with impaired cerebral autoregulation in preterm infants. Acta Paediatr. 103, 1221–1226 (2014).
Durrmeyer, X. et al. Abstention or intervention for isolated hypotension in the first 3 days of life in extremely preterm infants: association with short-term outcomes in the EPIPAGE 2 cohort study. Arch. Dis. Child. Fetal Neonatal Ed. 102, 490–496 (2017).
Dempsey, E. M., Al Hazzani, F. & Barrington, K. J. Permissive hypotension in the extremely low birthweight infant with signs of good perfusion. Arch. Dis. Child Fetal Neonatal Ed. 94, F241–F244 (2009).
Dempsey, E. M. et al. Management of hypotension in preterm infants (The HIP Trial): a randomised controlled trial of hypotension management in extremely low gestational age newborns. Neonatology 105, 275–281 (2014).
Papile, L. A., Burstein, J., Burstein, R. & Koffler, H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J. Pediatr. 92, 529–534 (1978).
Wong, F. Y., Nakamura, M., Alexiou, T., Brodecky, V. & Walker, A. M. Tissue oxygenation index measured using spatially resolved spectroscopy correlates with changes in cerebral blood flow in newborn lambs. Intensive Care Med. 35, 1464–1470 (2009).
Caicedo, A. et al. Decomposition of near-infrared spectroscopy signals using oblique subspace projections: applications in brain hemodynamic monitoring. Front. Physiol. 7, 515 (2016).
Caicedo, A. et al. Detection of cerebral autoregulation by near-infrared spectroscopy in neonates: performance analysis of measurement methods. J. Biomed. Opt. 17, 117003 (2012).
Hahn, G. H., Heiring, C., Pryds, O. & Greisen, G. Applicability of near-infrared spectroscopy to measure cerebral autoregulation noninvasively in neonates: a validation study in piglets. Pediatr. Res. 70, 166–170 (2011).
Schreiber, T. & Schmitz, A. Surrogate time series. Phys. D 142, 346–382 (2000).
Kleiser, S., Nasseri, N., Andresen, B., Greisen, G. & Wolf, M. Comparison of tissue oximeters on a liquid phantom with adjustable optical properties. Biomed. Opt. Express 7, 2973–2992 (2016).
van Bel, F., Lemmers, P. & Naulaers, G. Monitoring neonatal regional cerebral oxygen saturation in clinical practice: value and pitfalls. Neonatology 94, 237–244 (2008).
Harrell, F. Regression Modeling Strategies (Springer, 2001).
The International Neonatal Network. The CRIB (clinical risk index for babies) score: a tool for assessing initial neonatal risk and comparing performance of neonatal intensive care units. Lancet 342, 193–198 (1993).
Zhang, J., Penny, D. J., Kim, N. S., Yu, V. Y. H. & Smolich, J. J. Mechanisms of blood pressure increase induced by dopamine in hypotensive preterm neonates. Arch. Dis. Child. Fetal Neonatal Ed. 81, F99–F104 (1999).
Rennie, J. M. Cerebral blood flow velocity variability after cardiovascular support in premature babies. Arch. Dis. Child 64, 897–901 (1989).
Seri, I., Rudas, G., Bors, Z., Kanyicska, B. & Tulassay, T. Effects of low-dose dopamine infusion on cardiovascular and renal functions, cerebral blood flow, and plasma catecholamine levels in sick preterm neonates. Pediatr. Res. 34, 742–749 (1993).
Bouissou, A. et al. Hypotension in preterm infants with significant patent ductus arteriosus: effects of dopamine. J. Pediatr. 153, 790–794 (2008).
Pellicer, A. et al. Cardiovascular support for low birth weight infants and cerebral hemodynamics: a randomized, blinded, clinical trial. Pediatrics 115, 1501–1512 (2005).
Hyttel-Sorensen, S. et al. Cerebral near infrared spectroscopy oximetry in extremely preterm infants: phase II randomised clinical trial. BMJ 350, g7635 (2015).
Hansen, M. L. et al. Cerebral near-infrared spectroscopy monitoring versus treatment as usual for extremely preterm infants: a protocol for the SafeBoosC randomised clinical phase III trial. Trials 20, 811 (2019).
Alderliesten, T. et al. Hypotension in preterm neonates: low blood pressure alone does not affect neurodevelopmental outcome. J. Pediatr. 164, 986–991 (2014).
Chock, V. Y., Ramamoorthy, C. & Van Meurs, K. P. Cerebral autoregulation in neonates with a hemodynamically significant patent ductus arteriosus. J. Pediatr. 160, 936–942 (2012).
Cunningham, S., Symon, A. G., Elton, R. A., Zhu, C. & McIntosh, N. Intra-arterial blood pressure reference ranges, death and morbidity in very low birthweight infants during the first seven days of life. Early Hum. Dev. 56, 151–165 (1999).
Alderliesten, T. et al. Reference values of regional cerebral oxygen saturation during the first 3 days of life in preterm neonates. Pediatr. Res. 79, 55–64 (2016).
Alderliesten, T. et al. Low cerebral oxygenation in preterm infants is associated with adverse neurodevelopmental outcome. J. Pediatr. 207, 109–116 (2019). e102.
Plomgaard, A. M. et al. No neurodevelopmental benefit of cerebral oximetry in the first randomised trial (SafeBoosC II) in preterm infants during the first days of life. Acta Paediatr. 108, 275–281 (2019).
Menke, J., Michel, E., Hillebrand, S., von Twickel, J. & Jorch, G. Cross-spectral analysis of cerebral autoregulation dynamics in high risk preterm infants during the perinatal period. Pediatr. Res. 42, 690–699 (1997).
Greisen, G. To autoregulate or not to autoregulate-that is no longer the question. Semin. Pediatr. Neurol. 16, 207–215 (2009).
Vesoulis, Z. A. & Mathur, A. M. Cerebral autoregulation, brain injury, and the transitioning premature infant. Front. Pediatr. 5, 64 (2017).
Dix, L. M. L. et al. Carbon dioxide fluctuations are associated with changes in cerebral oxygenation and electrical activity in infants born preterm. J. Pediatr. 187, 66–72 e61 (2017).
Wyatt, J. S. et al. Response of cerebral blood volume to changes in arterial carbon dioxide tension in preterm and term infants. Pediatr. Res. 29, 553–557 (1991).
Vanderhaegen, J. et al. The effect of changes in tPCO2 on the fractional tissue oxygen extraction-as measured by near-infrared spectroscopy-in neonates during the first days of life. Eur. J. Paediatr. Neurol. 13, 128–134 (2009).
Kaiser, J. R., Gauss, C. H. & Williams, D. K. The effects of hypercapnia on cerebral autoregulation in ventilated very low birth weight infants. Pediatr. Res. 58, 931–935 (2005).
Lemmers, P. M. et al. Cerebral oxygenation and brain activity after perinatal asphyxia: does hypothermia change their prognostic value? Pediatr. Res. 74, 180–185 (2013).
Peng, S. et al. Does near-infrared spectroscopy identify asphyxiated newborns at risk of developing brain injury during hypothermia treatment? Am. J. Perinatol. 32, 555–564 (2015).
Ancora, G., Maranella, E., Locatelli, C., Pierantoni, L. & Faldella, G. Changes in cerebral hemodynamics and amplitude integrated EEG in an asphyxiated newborn during and after cool cap treatment. Brain Dev. 31, 442–444 (2009).
Cohen, E. et al. Cerebrovascular autoregulation in preterm fetal growth restricted neonates. Arch. Dis. Child Fetal Neonatal Ed. 104, F467–F472 (2019).
Acknowledgements
We thank Steffen Fieuws, statistician (Interuniversity Institute for Biostatistics and Statistical Bioinformatics, KU Leuven, Leuven, Belgium) for the statistical advice and analysis of the data. We thank Margreet Koolen, Isabelle Hermans, and Julie Messiaen, research nurses at University Hospitals Leuven and the Clinical Research Facility Cork for the support during the trial. This trial was funded by the European Union’s Seventh Framework Program (FP7/2007-2013) The HIP Trial: #260777.
Author information
Authors and Affiliations
Contributions
L.T. conceptualized and designed the study, collected data, carried out the initial analysis, drafted the initial manuscript, and reviewed and revised the manuscript for important intellectual content. G.N. and E.D. conceptualized and designed the study, collected data, coordinated and supervised data collection, and critically reviewed and revised the manuscript for important intellectual content. D.H. and A.C. conceptualized and designed the study, performed the data analysis, and reviewed and revised the manuscript for important intellectual content. K.B., G.B., P.-Y.C., D.C., A.E.-K., A.G., J.M., N.M., J.M., C.P.F.O’D., J.M.O’T., Z.S., D.V.L., and H.W. conceptualized and designed the study, collected data, and reviewed and revised the manuscript for important intellectual content. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
N.M. reports consultancy for Novartis and Shire, and is member of the Advisory Committee of GSK. The remaining authors declare no competing interests.
Consent statement
Parental informed consent was required for inclusion of infants in this study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Thewissen, L., Naulaers, G., Hendrikx, D. et al. Cerebral oxygen saturation and autoregulation during hypotension in extremely preterm infants. Pediatr Res 90, 373–380 (2021). https://doi.org/10.1038/s41390-021-01483-w
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-021-01483-w
This article is cited by
-
Cerebrovascular autoregulation and preterm brain injury: a systematic review and meta-analysis
Pediatric Research (2025)
-
Near-infrared spectroscopy monitoring of neonatal cerebrovascular reactivity: where are we now?
Pediatric Research (2024)
-
Clinical determinants of cerebrovascular reactivity in very preterm infants during the transitional period
Pediatric Research (2022)
-
How to safeguard the brain of extremely preterm infants?
Pediatric Research (2021)