Abstract
Objective
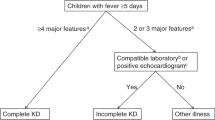
Kawasaki disease (KD) is a childhood vasculitis with conflicting reported North American trends in incidence and patient characteristics. Objectives: (1) determine KD incidence between 1995 and 2017; (2) compare patient characteristics by era and age group; (3) determine complication and cardiovascular follow-up rates.
Methods
We used population-based health administrative data to identify children (0–18 yr) hospitalized with KD in Ontario, Canada between 1995 and 2017. We excluded children with prior KD diagnosis or incomplete records. We determined the annualized incidence and follow-up trends.
Results
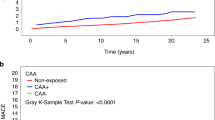
KD was diagnosed in 4,346 children between 1995 and 2017. Annual KD incidence was 22.0 (<5 yr), 6.1 (5–9 yr), and 0.6 (10–18 yr) per 100,000 children. KD incidence increased significantly for all age groups, including from 18.4 to 25.0 cases per 100,000 children <5 yr. Ninety-day mortality occurred in ≤5 children (≤0.1%). Coronary artery aneurysm (CAA) occurred in 106 children (2.4%, 95% confidence interval 2.0–2.9) during admission and 151 (3.5%, 95% confidence interval 3.0–4.1) during 11-year median follow-up. Children 10–18 yr had longer hospitalizations (4.3 vs. 3.5 days, p = 0.003) and more CAA (7.4% vs. 3.4%, p = 0.007). By 1-year post-diagnosis, 3970 (91.3%) and 2576 (59.3%) children had echocardiography and cardiology follow-up, respectively.
Conclusions
KD incidence is increasing in Ontario, with greater healthcare utilization from hospitalizations and subsequent follow-up.
Impact
-
4346 children were hospitalized for Kawasaki disease over 22 years in Ontario, and Kawasaki disease incidence increased significantly for all age groups, males and females.
-
Older children (10–18 years) had longer hospital length of stay, more PICU admissions and more frequent coronary artery aneurysms.
-
Nearly all children with Kawasaki disease had follow-up echocardiography within 1 year.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Burgner, D. & Harnden, A. Kawasaki disease: what is the epidemiology telling us about the etiology? Int. J. Infect. Dis. 9, 185–194 (2005).
Taubert, K. A., Rowley, A. H. & Shulman, S. T. Nationwide survey of Kawasaki disease and acute rheumatic fever. J. Pediatr. 119, 279–282 (1991).
Taubert, K. A. Epidemiology of Kawasaki disease in the United States and worldwide. Prog. Pediatr. Cardiol. 6, 181–185 (1997).
Holman, R. C. et al. Kawasaki syndrome hospitalizations in the United States, 1997 and 2000. Pediatrics 112, 495–501 (2003).
Makino, N. et al. Nationwide epidemiologic survey of Kawasaki disease in Japan, 2015-2016. Pediatr. Int J. Jpn Pediatr. Soc. 61, 397–403 (2019).
Singh, S., Vignesh, P. & Burgner, D. The epidemiology of Kawasaki disease: a global update. Arch. Dis. Child 100, 1084–1088 (2015).
Lin, M.-T. & Wu, M.-H. The global epidemiology of Kawasaki disease: review and future perspectives. Glob. Cardiol. Sci. Pract. 2017, https://doi.org/10.21542/gcsp.2017.20 (2018).
Ae, R. et al. Epidemiology, treatments, and cardiac complications in patients with Kawasaki Disease: the nationwide survey in Japan, 2017–2018. J. Pediatr. 225, 23–29 (2020).
Kim, G. B. et al. Epidemiology of Kawasaki disease in South Korea: a nationwide survey 2015–2017. Pediatr. Infect. Dis. J. 39, 1012–1016 (2020).
Huang, Y.-H. et al. Increased incidence of Kawasaki disease in Taiwan in recent years: a 15 years nationwide population-based cohort study. Front. Pediatr. 7, 121 (2019).
Manlhiot, C. et al. Epidemiology of Kawasaki disease in Canada 2004 to 2014: comparison of surveillance using administrative data vs periodic medical record review. Can. J. Cardiol. 34, 303–309 (2018).
Holman, R. C. et al. Hospitalizations for Kawasaki syndrome among children in the United States, 1997–2007. Pediatr. Infect. Dis. J. 29, 483–488 (2010).
Lin, Y. T. et al. Repeated systematic surveillance of Kawasaki disease in Ontario from 1995 to 2006: Kawasaki disease in Ontario, Canada. Pediatr. Int. 52, 699–706 (2010).
Chang, R. K. R. Hospitalizations for Kawasaki disease among children in the United States, 1988-1997. Pediatrics 109, e87 (2002).
Williams, C. L. et al. A systematic review of validated methods for identifying Kawasaki disease using administrative or claims data. Vaccine 31, K28–K33 (2013).
Statistics Canada. Ontario [Province] and Canada [Country] (table). Census profile. 2016 Census. https://www12.statcan.gc.ca/census-recensement/2016/dp-pd/prof/index.cfm?Lang=E. Accessed 10 Dec 2019 (2017).
von Elm, E. et al. The strengthening the reporting of observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet Lond. Engl. 370, 1453–1457 (2007).
Benchimol, E. I. et al. The reporting of studies conducted using observational routinely-collected health Data (RECORD) Statement. PLoS Med. 12, e1001885 (2015).
Shah, B. R. et al. Surname lists to identify South Asian and Chinese ethnicity from secondary data in Ontario, Canada: a validation study. BMC Med. Res. Methodol. 10, https://doi.org/10.1186/1471-2288-10-42 (2010)
Chanchlani, R. et al. Secular trends in incidence, modality and mortality with dialysis receiving AKI in children in Ontario: a population-based cohort study. Clin. J. Am. Soc. Nephrol. 14, 1288–1296 (2019).
Bollman, R. Rural Demography Update. Rural Ontario Institute 2016. http://www.ruralontarioinstitute.ca/file.aspx?id=26acac18-6d6e-4fc5-8be6-c16d326305fe. Accessed 10 Dec 2019 (2016).
Canadian Institute for Health Information (CIHI). Health Indicators 2013. Canadian Institute for Health Information 2013. https://secure.cihi.ca/free_products/HI2013_EN.pdf. Accessed 18 Dec 2019 (2013).
Armitage, P. Tests for linear trends in proportions and frequencies. Biometrics 11, 375 (1955).
Kim, G. B. et al. Epidemiology and clinical features of Kawasaki disease in South Korea, 2012-2014. Pediatr. Infect. Dis. J. 36, 482–485 (2017).
Ghelani, S. J. et al. Increased incidence of incomplete Kawasaki disease at a pediatric hospital after publication of the 2004 American Heart Association guidelines. Pediatr. Cardiol. 33, 1097–1103 (2012).
Hearn, J. et al. Spatiotemporal clustering of cases of Kawasaki disease and associated coronary artery aneurysms in Canada. Sci. Rep. 8, 17682 (2018).
Uehara, R. & Belay, E. D. Epidemiology of Kawasaki disease in Asia, Europe, and the United States. J. Epidemiol. 22, 79–85 (2012).
Holman, R. C. et al. Racial/ethnic differences in the incidence of Kawasaki syndrome among children in Hawaii. Hawaii Med. J. 69, 194–197 (2010).
Nakamura, Y. et al. Mortality among Japanese with a history of Kawasaki disease: results at the end of 2009. J. Epidemiol. 23, 429–434 (2013).
Son, M. B. F. et al. Treatment of Kawasaki disease: analysis of 27 US pediatric hospitals from 2001 to 2006. Pediatrics 124, 1–8 (2009).
Nakamura, Y. et al. Mortality among persons with a history of Kawasaki disease in Japan: the fifth look. Arch. Pediatr. Adolesc. Med 156, 162 (2002).
Kato, H., Ichinose, E. & Kawasaki, T. Myocardial infarction in Kawasaki disease: clinical analyses in 195 cases. J. Pediatr. 108, 923–927 (1986).
Muta, H. et al. Older age is a risk factor for the development of cardiovascular sequelae in Kawasaki disease. Pediatrics 114, 751–754 (2004).
Song, D. et al. Risk factors for Kawasaki disease-associated coronary abnormalities differ depending on age. Eur. J. Pediatr. 168, 1315–1321 (2009).
Minich, L. L. et al. Delayed diagnosis of Kawasaki disease: what are the risk factors? Pediatrics 120, e1434–e1440 (2007).
Nolan, B. E. et al. High-dose intravenous immunoglobulin is strongly associated with hemolytic anemia in patients with Kawasaki disease. Transfusion 58, 2564–2571 (2018).
Luban, N. L. C. et al. Intravenous immunoglobulin-related hemolysis in patients treated for Kawasaki disease: IVIG-related hemolysis and Kawasaki disease. Transfusion 55, S90–S94 (2015).
McCrindle, B. W. et al. Diagnosis, treatment, and long-term management of kawasaki disease: a scientific statement for health professionals from the American Heart Association. Circulation 135, e927–e999 (2017).
Dajani, A. S. et al. Guidelines for long-term management of patients with Kawasaki disease. Report from the Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease, Council on Cardiovascular Disease in the Young, American Heart Association. Circulation 89, 916–922 (1994).
Newburger, J. W. et al. Diagnosis, treatment, and long-term management of Kawasaki disease: a statement for health professionals from the Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease, Council on Cardiovascular Disease in the Young, American Heart Association. Pediatrics 114, 1708–1733 (2004).
Lowry, A. W. et al. Variability in delivery of care and echocardiogram surveillance of Kawasaki disease. Congenit. Heart Dis. 7, 336–343 (2012).
Bronstein, D. E., Besser, R. E. & Burns, J. C. Passive surveillance for Kawasaki disease in San Diego County. Pediatr. Infect. Dis. J. 16, 1015–1018 (1997).
Kao, A. S. et al. Spatial and temporal clustering of Kawasaki syndrome cases. Pediatr. Infect. Dis. J. 27, 981–985 (2008).
Holve, T. J. et al. Long-term cardiovascular outcomes in survivors of Kawasaki disease. Pediatrics 133, e305–e311 (2014).
Acknowledgements
This study was supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care. This study received funding from institutional grants from Hamilton Health Sciences and McMaster University Department of Pediatrics. Parts of this material are based on data and/or information compiled and provided by CIHI. However, the analyses, conclusions, opinions, and statements expressed in the material are those of the authors, and not necessarily those of CIHI. We thank the ICES McMaster and Ottawa teams, including Richard Perez for his dedicated work planning and supervising analysis for this study, as well as Erin O’Leary for project coordination. M.B. was supported by a New Investigator Fund from Hamilton Health Sciences. C.R. was supported by Resident Research Award funding from the Department of Pediatrics, McMaster University. E.I.B. was supported by a New Investigator Award from the Canadian Institutes of Health Research, Canadian Association of Gastroenterology, and Crohn’s and Colitis Canada. E.I.B. was also supported by the Career Enhancement Program of the Canadian Child Health Clinician Scientist Program.
Author information
Authors and Affiliations
Contributions
C.R., R.C., and M.B. conceptualized and designed the study, coordinated and supervised data collection and analysis, drafted the initial manuscript, and reviewed and revised the manuscript. H.S., E.D., and E.I.B. conceptualized and designed the study, coordinated and supervised data collection and analysis, and reviewed and revised the manuscript. S.B., C.D., T.M., R.P., J.K., B.K., E.K., C.J.-R., and R.W. reviewed and revised the proposed study design, reviewed data analyses, assisted with data interpretation, and reviewed and revised the manuscript. A.G. conceptualized and designed the study, was primarily responsible for data collection and analysis, and reviewed and revised the manuscript. All authors have approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Data sharing
Deidentified individual participant data will not be made available.
Ethical approval
The use of data in this project was authorized under section 45 of Ontario’s Personal Health Information Protection Act and was approved by Hamilton Integrated Research Ethics Board.
Patient consent
ICES is an independent, non-profit research institute whose legal status under Ontario’s health information privacy law allows it to collect and analyze healthcare and demographic data, without consent, for health system evaluation and improvement.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Robinson, C., Chanchlani, R., Gayowsky, A. et al. Incidence and short-term outcomes of Kawasaki disease. Pediatr Res 90, 670–677 (2021). https://doi.org/10.1038/s41390-021-01496-5
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-021-01496-5
This article is cited by
-
Impact of intravenous immunoglobulin treatment on peripheral blood cells in children with Kawasaki disease complicated with coronary artery lesion
Italian Journal of Pediatrics (2025)
-
An Update on Kawasaki Disease
Current Rheumatology Reports (2025)
-
Incomplete Kawasaki Disease with Bilateral Parotid Involvement, Pancreatitis and Genital Excoriation
Indian Journal of Pediatrics (2024)
-
Unexpectedly high incidence of Kawasaki Disease in a Canadian Atlantic Province- an 11-year retrospective descriptive study
Pediatric Rheumatology (2023)
-
Cardiovascular outcomes in children with Kawasaki disease: a population-based cohort study
Pediatric Research (2023)