Abstract
Background
Given the high prevalence and complication risks of acid gastroesophageal reflux (GERD) in the first months of life in infants with esophageal atresia, the ESPGHAN/NASPGHAN consensus statement recommends systematic treatment with proton pump inhibitors (PPIs) until the age of 1 year and checking for acid GERD thereafter. However, these recommendations have not been evaluated.
Methods
This prospective study was conducted from 2007 to 2016. We evaluated the prevalence of acid GERD in 100 consecutive infants presenting with esophageal atresia/tracheoesophageal fistula after the age of 18 months when PPI treatment was stopped. The diagnosis of acid GERD was based on positive pH-metry and/or evidence of complications (e.g., peptic esophagitis, need for jejunal nutrition, or antireflux surgery). Those with acid GERD at a median age of 18 months received a control examination every year or adapted to their clinical situation.
Results
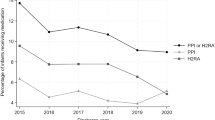
The prevalence rates of acid GERD were 64.3% at 18 months and 22.8% at the last follow-up (median age 65 months).There is no risk factor for acid GERD identified.
Conclusions
This study shows a high prevalence of acid GERD in late infancy and supports the recommendation of systematic checking for acid GERD when treatment with PPI is stopped.
Impact
-
Acid gastroesophageal reflux disease (GERD) is a frequent complication of esophageal atresia in infants. The ESPGHAN/NASPGHAN consensus, which is based on expert opinion, recommends systematic treatment of children with PPI until the age of 1 year.
-
The prevalence rates of acid GERD were 64.3% at 18 months and 22.8% at the last follow-up. This study shows a high prevalence of acid GERD in late infancy and supports the recommendation of systematic checking for acid GERD when treatment with PPI is stopped.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Sfeir, R., Michaud, L., Salleron, J. & Gottrand, F. Epidemiology of esophageal atresia. Dis. Esophagus 26, 354–355 (2013).
Nassar, N. et al. Prevalence of esophageal atresia among 18 international birth defects surveillance programs. Birth Defects Res. A Clin. Mol. Teratol. 94, 893–899 (2012).
Goyal, A., Jones, M. O., Couriel, J. M. & Losty, P. D. Oesophageal atresia and tracheo-oesophageal fistula. Arch. Dis. Child Fetal Neonatal Ed. 91, F381–F384 (2006).
Montgomery, M. & Frenckner, B. Esophageal atresia: mortality and complications related to gastroesophageal reflux. Eur. J. Pediatr. Surg. 3, 335–338 (1993).
Legrand, C. et al. Long-term outcome of children with oesophageal atresia type III. Arch. Dis. Child. 97, 808–811 (2012).
Martigne, L. et al. Prevalence and management of gastroesophageal reflux disease in children and adolescents: a nationwide cross-sectional observational study. Eur. J. Pediatr. 171, 1767–1773 (2012).
Deurloo, J. A., Ekkelkamp, S., Schoorl, M., Heij, H. A. & Aronson, D. C. Esophageal atresia: historical evolution of management and results in 371 patients. Ann. Thorac. Surg. 73, 267–272 (2002).
Little, D. C. et al. Long-term analysis of children with esophageal atresia and tracheoesophageal fistula. J. Pediatr. Surg. 38, 852–856 (2003).
Somppi, E. et al. Outcome of patients operated on for esophageal atresia: 30 years’ experience. J. Pediatr. Surg. 33, 1341–1346 (1998).
Hameeteman, W., Tytgat, G. N., Houthoff, H. J. & van den Tweel, J. G. Barrett’s esophagus: development of dysplasia and adenocarcinoma. Gastroenterology 96, 1249–1256 (1989).
Schneider, A. et al. Prevalence of Barrett esophagus in adolescents and young adults with esophageal atresia. Ann. Surg. 264, 1004–1008 (2016).
Shawyer, A. C., Pemberton, J., Kanters, D., Alnaqi, A. A. A. & Flageole, H. Quality of reporting of the literature on gastrointestinal reflux after repair of esophageal atresia-tracheoesophageal fistula. J. Pediatr. Surg. 50, 1099–1103 (2015).
Centre de référence des affections chroniques et malformatives de l'oesophage (CRACMO) et Filière nationale des maladies rares abdominothoraciques (FIMATHO), Protocole Nationale de Diagnostic et de Soins, Atrésie de l'oesophage, 2018. Available from: https://www.has-sante.fr/upload/docs/application/pdf/2018-12/20181212_pnds_atresie_de_loesophage_dec_2018_vf_charte.pdf.
Krishnan, U. et al. ESPGHAN-NASPGHAN Guidelines for the Evaluation and Treatment of Gastrointestinal and Nutritional Complications in Children With Esophageal Atresia-Tracheoesophageal Fistula. J. Pediatr. Gastroenterol. Nutr. 63, 550–570 (2016).
Ladd, W. E., Swenson, O. & Esophageal Atresia and tracheo-esophageal fistula. Ann. Surg. 125, 23–40 (1947).
Dingemann, C. et al. ERNICA Consensus Conference on the Management of Patients with Long-Gap Esophageal Atresia: Perioperative, Surgical, and Long-Term Management. Eur. J. Pediatr. Surg. 30, 326–336 (2020).
François, B. et al. Predictors of the performance of early antireflux surgery in esophageal atresia. J. Pediatr. 211, 120.e1–125.e1 (2019).
Vandenplas, Y. et al. Pediatric gastroesophageal reflux clinical practice guidelines: joint recommendations of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN) and the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN). J. Pediatr. Gastroenterol. Nutr. 49, 498–547 (2009).
Prentice, R. L. et al. The analysis of failure times in the presence of competing risks. Biometrics 34, 541–554 (1978).
Castilloux, J., Noble, A. J. & Faure, C. Risk factors for short- and long-term morbidity in children with esophageal atresia. J. Pediatr. 156, 755–760 (2010).
Catalano, P., Di Pace, M. R., Caruso, A. M., Casuccio, A. & De Grazia, E. Gastroesophageal reflux in young children treated for esophageal atresia: evaluation with pH-multichannel intraluminal impedance. J. Pediatr. Gastroenterol. Nutr. 52, 686–690 (2011).
Vergouwe, F. W. T. et al. Evaluation of gastroesophageal reflux in children born with esophageal atresia using pH and impedance monitoring. J. Pediatr. Gastroenterol. Nutr. 69, 515–522 (2019).
Righini Grunder, F. et al. Should proton pump inhibitors be systematically prescribed in patients with esophageal atresia after surgical repair? J. Pediatr. Gastroenterol. Nutr. 69, 45–51 (2019).
Koivusalo, A., Pakarinen, M. P. & Rintala, R. J. The cumulative incidence of significant gastrooesophageal reflux in patients with oesophageal atresia with a distal fistula-a systematic clinical, pH-metric, and endoscopic follow-up study. J. Pediatr. Surg. 42, 370–374 (2007).
Nakazato, Y., Landing, B. H. & Wells, T. R. Abnormal Auerbach plexus in the esophagus and stomach of patients with esophageal atresia and tracheoesophageal fistula. J. Pediatr. Surg. 21, 831–837 (1986).
Gottrand, M., Michaud, L., Sfeir, R. & Gottrand, F. Motility, digestive and nutritional problems in esophageal atresia. Paediatr. Respir. Rev. 19, 28–33 (2016).
Bardou, M., Fortinsky, K. J., Chapelle, N., Luu, M. & Barkun, A. An update on the latest chemical therapies for reflux esophagitis in children. Expert Opin. Pharmacother. 20, 231–239 (2019).
Schneider, A. et al. Results from the French National Esophageal Atresia register: one-year outcome. Orphanet J. Rare Dis. 9, 206 (2014).
Koumbourlis, A. C. et al. Care recommendations for the respiratory complications of esophageal atresia-tracheoesophageal fistula. Pediatr. Pulmonol. 55, 2713–2729 (2020).
Chang, T.-H. et al. Increased age and proton pump inhibitors are associated with severe Clostridium difficile infections in children. J. Microbiol Immunol. Infect. 53, 578–584 (2020).
Poddar, U. Gastroesophageal reflux disease (GERD) in children. Paediatr. Int. Child Health 39, 7–12 (2019).
De Bruyne, P. & Ito, S. Toxicity of long-term use of proton pump inhibitors in children. Arch. Dis. Child. 103, 78–82 (2018).
Miyake, H. et al. Are prophylactic anti-reflux medications effective after esophageal atresia repair? Systematic review and meta-analysis. Pediatr. Surg. Int. 34, 491–497 (2018).
Acknowledgements
In memory of Dr. L Michaud, who inspired this study.
Author information
Authors and Affiliations
Contributions
C.F. and F.G. contributed to conception and design, acquisition of data, analysis and interpretation of data, drafting the article, and final approval of the version to be published. M.A. contributed to conception and design and final approval of the version to be published. D.L., R.S., A.N., and M.B. contributed to final approval of the version to be published. A.D. contributed to analysis and interpretation of data.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent statement
Data were collected from a population-based registry of esophageal atresia, which began collecting data prospectively on all infants born with esophageal atresia in France from January 1, 2007. The registry was approved by the National Informatics and Privacy Committee and was qualified by the National Committee of Register. All data were used anonymously, and the parents were informed of the aims of the registry.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Flatrès, C., Aumar, M., Ley, D. et al. Prevalence of acid gastroesophageal reflux disease in infants with esophageal atresia/tracheoesophageal fistula. Pediatr Res 91, 977–983 (2022). https://doi.org/10.1038/s41390-021-01510-w
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-021-01510-w
This article is cited by
-
Esophageal atresia with concomitant hypertrophic pyloric stenosis: a case series and literature review
BMC Pediatrics (2025)
-
Endoscopic management of esophageal mucosal bridges in children with esophageal atresia
Surgical Endoscopy (2023)