Abstract
Background
The objective of this study was to determine sex-specific differences in inflammatory cytokine responses to red blood cell (RBC) transfusion in preterm infants in the neonatal period and their relationship to later neurocognitive status.
Methods
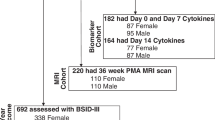
Infants with a birth weight <1000 g and gestational age 22–29 weeks were enrolled in the Transfusion of Prematures (TOP) trial. The total number of transfusions was used as a marker of transfusion status. Nineteen cytokines and biomarkers were analyzed from 71 infants longitudinally during the neonatal period. Twenty-six infants completed the Bayley Scales of Infant & Toddler Development, 3rd Edition (Bayley-III) at 12 months’ corrected age.
Results
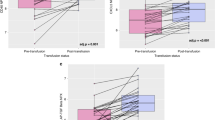
Nine cytokine levels were significantly elevated in proportion to the number of transfusions received. Of those, one cytokine showed a sex-specific finding (p = 0.004): monocyte chemoattractant protein-1, MCP-1, rose substantially in females (8.9% change per additional transfusion), but not in males (−0.8% change). Higher concentrations of MCP-1 exclusively were associated with worse Bayley-III scores: decreased cognitive raw scores (p = 0.0005) and motor scaled scores (p < 0.0001).
Conclusions
This study provides evidence of a sex-specific difference in the inflammatory response to RBC transfusions during neonatal life, with MCP-1 levels rising only in females and inversely correlating with neurocognitive status at 12 months old.
Impact
-
It is important to understand the risk factors for abnormal neurodevelopment in preterm infants, including anemia and RBC transfusion, in order to improve outcomes and provide potential targets for therapy.
-
Our study investigates and provides the first evidence of sex-specific differences in inflammatory cytokine responses to RBC transfusions in preterm infants in the neonatal period, and their relationship to later cognitive outcomes.
-
This study critically suggests that different transfusion thresholds may have a sex-specific effect on neurodevelopment: females have worse cognitive outcomes with increased number of transfusions, while males have worse outcomes with lower number of transfusions.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Saigal, S. & Doyle, L. W. An overview of mortality and sequelae of preterm birth from infancy to adulthood. Lancet 371, 261–269 (2008).
Orchinik, L. J. et al. Cognitive outcomes for extremely preterm/extremely low birth weight children in kindergarten. J. Int. Neuropsychol. Soc. 17, 1067–1079 (2011).
Arpino, C. et al. Preterm birth and neurodevelopmental outcome: a review. Childs Nerv. Syst. 26, 1139–1149 (2010).
Aarnoudse-Moens, C. S., Weisglas-Kuperus, N., van Goudoever, J. B. & Oosterlaan, J. Meta-analysis of neurobehavioral outcomes in very preterm and/or very low birth weight children. Pediatrics 124, 717–728 (2009).
Allen, M. C. Neurodevelopmental outcomes of preterm infants. Curr. Opin. Neurol. 21, 123–128 (2008).
Anderson, P. & Doyle, L. W. Neurobehavioral outcomes of school-age children born extremely low birth weight or very preterm in the 1990s. JAMA 289, 3264–3272 (2003).
Bhutta, A. T. et al. Cognitive and behavioral outcomes of school-aged children who were born preterm: a meta-analysis. JAMA 288, 728–737 (2002).
Maier, R. F. et al. Changing practices of red blood cell transfusions in infants with birth weights less than 1000 g. J. Pediatr. 136, 220–224 (2000).
Strauss, R. G. Transfusion therapy in neonates. Am. J. Dis. Child. 145, 904–911 (1991).
Keir, A. K. et al. Temporal changes in blood product usage in preterm neonates born at less than 30 weeks’ gestation in Canada. Transfusion 55, 1340–1346 (2015).
Howarth, C., Banerjee, J. & Aladangady, N. Red blood cell transfusion in preterm infants: current evidence and controversies. Neonatology 114, 7–16 (2018).
Kirpalani, H. et al. Higher or lower hemoglobin transfusion thresholds for preterm infants. N. Engl. J. Med. 383, 2639–2651 (2020).
Aylward, G. P. Update on neurodevelopmental outcomes of infants born prematurely. J. Dev. Behav. Pediatr. 35, 392–393 (2014).
Hutchinson, E. A. et al. School-age outcomes of extremely preterm or extremely low birth weight children. Pediatrics 131, e1053–e1061 (2013).
Aylward, G. P. Neurodevelopmental outcomes of infants born prematurely. J. Dev. Behav. Pediatr. 26, 427–440 (2005).
Carlo, W. A. et al. Cytokines and neurodevelopmental outcomes in extremely low birth weight infants. J. Pediatr. 159, 919–25 e3 (2011).
Leviton, A. et al. The relationship between early concentrations of 25 blood proteins and cerebral white matter injury in preterm newborns: the ELGAN study. J. Pediatr. 158, 897–903.e1 (2011).
Basu, S. et al. Elevated plasma and cerebrospinal fluid interleukin-1 beta and tumor necrosis factor-alpha concentration and combined outcome of death or abnormal neuroimaging in preterm neonates with early-onset clinical sepsis. J. Perinatol. 35, 855–861 (2015).
Hagberg, H. et al. The role of inflammation in perinatal brain injury. Nat. Rev. Neurol. 11, 192–208 (2015).
Aden, U. et al. Systemic inflammation sensitizes the neonatal brain to excitotoxicity through a pro-/anti-inflammatory imbalance: key role of TNFalpha pathway and protection by etanercept. Brain Behav. Immun. 24, 747–758 (2010).
Van Steenwinckel, J. et al. Brain damage of the preterm infant: new insights into the role of inflammation. Biochem. Soc. Trans. 42, 557–563 (2014).
Kinjo, T. et al. Serum chemokine levels and developmental outcome in preterm infants. Early Hum. Dev. 87, 439–443 (2011).
Dammann, O. & Leviton, A. Intermittent or sustained systemic inflammation and the preterm brain. Pediatr. Res. 75, 376–380 (2014).
Benavides, A. et al. Sex-specific alterations in preterm brain. Pediatr. Res. https://doi.org/10.1038/s41390-018-0187-5 (2018).
Nopoulos, P. C. et al. Long-term outcome of brain structure in premature infants: effects of liberal vs restricted red blood cell transfusions. Arch. Pediatr. Adolesc. Med. 165, 443–450 (2011).
Keir, A. K., McPhee, A. J., Andersen, C. C. & Stark, M. J. Plasma cytokines and markers of endothelial activation increase after packed red blood cell transfusion in the preterm infant. Pediatr. Res. 73, 75–79 (2013).
Dani, C. et al. Red blood cell transfusions can induce proinflammatory cytokines in preterm infants. Transfusion 57, 1304–1310 (2017).
Yu, H. et al. Serum concentrations of cytokines in infants with retinopathy of prematurity. APMIS 122, 818–823 (2014).
Transfusion of Prematures Trial (TOP). National Library of Medicine (US). https://clinicaltrials.gov/ct2/show/NCT01702805 (2012).
Holm, S. A simple sequentially rejective multiple test procedure. Scand. J. Stat. 6, 65–70 (1979).
Benjamini, Y. & Yekutieli, D. The control of the false discovery rate in multiple testing under dependency. Ann. Stat. 29, 1165–1188 (2001).
Cerri, C., Caleo, M. & Bozzi, Y. Chemokines as new inflammatory players in the pathogenesis of epilepsy. Epilepsy Res. 136, 77–83 (2017).
Lu, H. et al. Relationship between premature brain injury and multiple biomarkers in cord blood and amniotic fluid. J. Matern. Fetal Neonatal Med. https://doi.org/10.1080/14767058.2017.1359532, 1–7 (2017).
Semple, B. D. et al. Role of CCL2 (MCP-1) in traumatic brain injury (TBI): evidence from severe TBI patients and CCL2-/- mice. J. Cereb. Blood Flow. Metab. 30, 769–782 (2010).
Ho, L. et al. Elevated plasma MCP-1 concentration following traumatic brain injury as a potential “predisposition” factor associated with an increased risk for subsequent development of Alzheimer’s disease. J. Alzheimer’s Dis. 31, 301–313 (2012).
Bartha, A. I. et al. Neonatal encephalopathy: association of cytokines with MR spectroscopy and outcome. Pediatr. Res. 56, 960–966 (2004).
Wu, D. et al. The association of genetic polymorphisms with cerebral palsy: a meta-analysis. Dev. Med. Child Neurol. 53, 217–225 (2011).
Graham, A. M. et al. Maternal systemic interleukin-6 during pregnancy is associated with newborn amygdala phenotypes and subsequent behavior at 2 years of age. Biol. Psychiatry 83, 109–119 (2018).
Romero, R. et al. CXCL10 and IL-6: markers of two different forms of intra-amniotic inflammation in preterm labor. Am. J. Reprod. Immunol. 78, https://doi.org/10.1111/aji.12685 (2017).
McAdams, R. M. & Juul, S. E. The role of cytokines and inflammatory cells in perinatal brain injury. Neurol. Res. Int. 2012, 561494 (2012).
Franz, A. R. et al. Effects of liberal vs restrictive transfusion thresholds on survival and neurocognitive outcomes in extremely low-birth-weight infants: the ETTNO Randomized Clinical Trial. JAMA 324, 560–570 (2020).
Georgieff, M. K. Long-term brain and behavioral consequences of early iron deficiency. Nutr. Rev. 69, S43–S48 (2011).
Lozoff, B. & Georgieff, M. K. Iron deficiency and brain development. Semin. Pediatr. Neurol. 13, 158–165 (2006).
Lozoff, B. et al. Long-lasting neural and behavioral effects of iron deficiency in infancy. Nutr. Rev. 64, S34–S43 (2006).
Aggarwal, B. B. Signalling pathways of the TNF superfamily: a double-edged sword. Nat. Rev. Immunol. 3, 745–756 (2003).
Ward-Kavanagh, L. K., Lin, W. W., Sedy, J. R. & Ware, C. F. The TNF receptor superfamily in co-stimulating and co-inhibitory responses. Immunity 44, 1005–1019 (2016).
Etemadi, N. et al. Lymphotoxin alpha induces apoptosis, necroptosis and inflammatory signals with the same potency as tumour necrosis factor. FEBS J. 280, 5283–5297 (2013).
Tumanov, A. V. et al. Dissecting the role of lymphotoxin in lymphoid organs by conditional targeting. Immunol. Rev. 195, 106–116 (2003).
Patel, J. R. et al. Astrocyte TNFR2 is required for CXCL12-mediated regulation of oligodendrocyte progenitor proliferation and differentiation within the adult CNS. Acta Neuropathol. 124, 847–860 (2012).
McCoy, T. E. et al. The relationship between brain structure and cognition in transfused preterm children at school age. Dev. Neuropsychol. 39, 226–232 (2014).
McCoy, T. E. et al. Neurocognitive profiles of preterm infants randomly assigned to lower or higher hematocrit thresholds for transfusion. Child Neuropsychol. 17, 347–367 (2011).
Dani, C. et al. Blood transfusions increase cerebral, splanchnic, and renal oxygenation in anemic preterm infants. Transfusion 50, 1220–1226 (2010).
Arthur, C. M. et al. Anemia induces gut inflammation and injury in an animal model of preterm infants. Transfusion 59, 1233–1245 (2019).
Acknowledgements
The design and conduct of this research study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript were made possible by National Institute for Heart, Lung, and Blood (NHLBI) Parent Project Grant #5P01HL046925-22, Sub-Project ID 5779, “Immunologic and Neurodevelopmental Consequences of Neonatal Anemia and Thrombocytopenia and Their Treatments—Project 4,” and National Institute for Mental Health (NIMH) Program Grant #5T32MH019113-26 “Iowa Neuroscience Specialty Program in Research Education (INSPIRE) Program Grant.” We confirm that this manuscript has not been previously published and has not been submitted simultaneously for publication elsewhere. I, A.B., had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Author information
Authors and Affiliations
Contributions
A.B. was involved in conceptualization/design, methodology, data curation and formal analysis, and writing initial draft of this manuscript, and confirms that all authors participated in the conceptualization/design, review, and editing of this manuscript. Additionally, D.N. provided significant expertise in the methodology of transfusion, blood banking, and cytokine sampling used in this study. H.A.F. contributed significantly to the supervision/oversight, statistical methodology, and formal analysis of all data presented in this manuscript. As part of multi-institutional program project grant, H.A.F., M.K.G., C.D.J., P.N., S.R.S., and M.S.-V. provided acquisition of funding for this manuscript, as well as critical supervision/oversight and feedback for revision throughout the manuscript writing and submission process. All authors have reviewed and approved the final version of the manuscript as submitted and agree with its submission to Pediatric Research.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Statement of consent
Parents of all subjects in this study provided informed consent for participation, in full accordance with institutional review board requirements for human subject research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Benavides, A., Bell, E.F., Georgieff, M.K. et al. Sex-specific cytokine responses and neurocognitive outcome after blood transfusions in preterm infants. Pediatr Res 91, 947–954 (2022). https://doi.org/10.1038/s41390-021-01536-0
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-021-01536-0
This article is cited by
-
The transfusion of prematures early school age follow-up (TOP 5): protocol for a longitudinal cohort study
BMC Pediatrics (2025)
-
Biological sex and transfusion practices in the NICU
Pediatric Research (2025)
-
Neurodevelopmental outcomes after red cell transfusion exposure in male versus female extremely preterm infants
Pediatric Research (2025)
-
Stored RBC transfusions leads to the systemic inflammatory response syndrome in anemic murine neonates
Inflammation Research (2024)
-
Identification and prediction model of placenta-brain axis genes associated with neurodevelopmental delay in moderate and late preterm children
BMC Medicine (2023)