Abstract
Introduction
Pediatric critical care patients with COVID-19 treated in Peru have higher mortality than those previously reported from other countries. Pediatric providers have reported a high number of patients without comorbidities presenting with hemorrhagic strokes associated with COVID-19. We present a study analyzing the factors associated with mortality in this setting.
Methods
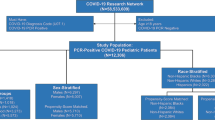
Prospective case–control study that included patients <17 years old admitted to a pediatric critical care unit with a positive test confirming COVID-19. The primary outcome was mortality. Fisher’s exact test and the Mann–Whitney U test were used for the analysis.
Results
Forty-seven patients were admitted to critical care. The mortality of our study is 21.3%. The mortality of patients with neurological presentation was 45.5%, which was significantly higher than the mortality of acute COVID-19 (26.7%) and MIS-C (4.8%), p 0.18. Other risk factors for mortality in our cohort were strokes and comorbidities. Only one patient presenting with hemorrhagic stroke had an undiagnosed comorbidity.
Conclusion
Cerebrovascular events associated with COVID-19 in pediatric patients, including infants, must be recognized as one of the more severe presentations of this infection in pediatric patients.
Impact
-
Pediatric patients with COVID-19 can present with hemorrhagic and ischemic strokes on presentation.
-
Neurological presentation in pediatric patients with COVID-19 has high mortality.
-
Mortality of pediatric patients with COVID-19 is associated with comorbidities.
-
Pediatric presentation and outcomes of COVID-19 in different regions can be novel to previously described.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Dong, Y. et al. Epidemiology of COVID-19 Among Children in China. Pediatrics 145, e20200702 (2020).
Parri, N., Lenge, M. & Buonsenso, D. Children with Covid-19 in pediatric emergency departments in Italy. N. Engl. J. Med. 383, 187–190 (2020).
Swann, O. V. et al. Clinical characteristics of children and young people admitted to hospital with covid-19 in United Kingdom: prospective multicentre observational cohort study. Bmj 370, m3249 (2020).
Belhadjer, Z. et al. Acute heart failure in multisystem inflammatory syndrome in children in the context of global SARS-CoV-2 Pandemic. Circulation 142, 429–436 (2020).
C. D. C. Multisystem Inflammatory Syndrome in Children (MIS-C) associated with Coronavirus Disease 2019 (COVID-19), case definition for MIS-C. In HAN (ed), https://emergency.cdc.gov/han/2020/han00432.asp (2020).
Feldstein, L. R. et al. Multisystem inflammatory syndrome in U.S. children and adolescents. N. Engl. J. Med. 383, 334–346 (2020).
Panupattanapong, S. & Brooks, E. B. New spectrum of COVID-19 manifestations in children: Kawasaki-like syndrome and hyperinflammatory response. Cleve Clin. J. Med. Epub ahead of print (2020).
Riphagen, S., Gomez, X., Gonzalez-Martinez, C., Wilkinson, N. & Theocharis, P. Hyperinflammatory shock in children during COVID-19 pandemic. Lancet 395, 1607–1608 (2020).
Toubiana, J. et al. Kawasaki-like multisystem inflammatory syndrome in children during the covid-19 pandemic in Paris, France: prospective observational study. BMJ 369, m2094 (2020).
Grimaud, M. et al. Acute myocarditis and multisystem inflammatory emerging disease following SARS-CoV-2 infection in critically ill children. Ann. Intensive Care 10, 69 (2020).
Kaushik, S. et al. Multisystem inflammatory syndrome in children associated with severe acute respiratory syndrome coronavirus 2 infection (MIS-C): a multi-institutional study from New York city. J. Pediatr. 224, 24–29 (2020).
Shekerdemian, L. S. et al. Characteristics and outcomes of children with Coronavirus Disease 2019 (COVID-19) infection admitted to US and Canadian Pediatric Intensive Care Units. JAMA Pediatr. Sep 1 174, 868–873 (2020).
Garcia-Salido, A. et al. Children in critical care due to severe acute respiratory syndrome coronavirus 2 infection: experience in a Spanish hospital. Pediatr. Crit. Care Med. 24, 666 (2020).
González-Dambrauskas, S. et al. Pediatric critical care and COVID19. Pediatrics. 146, e20201766 (2020).
Sachdeva, R. et al. The impact of coronavirus disease 2019 pandemic on U.S. and Canadian PICUs. Pediatr. Crit. Care Med. 21, e643–e650 (2020).
Force, A. D. T. et al. Acute respiratory distress syndrome: the Berlin Definition. JAMA 307, 2526–2533 (2012).
Parsons, T. et al. COVID-19-associated acute disseminated encephalomyelitis (ADEM). J. Neurol. 267, 2799–2802 (2020).
Mirzaee, S. M. M., Gonçalves, F. G., Mohammadifard, M., Tavakoli, S. M. & Vossough, A. Focal cerebral arteriopathy in a COVID-19 pediatric patient. Radiology. 297, E274–E275 (2020).
Ellul, M. A. et al. Neurological associations of COVID-19. Lancet Neurol. Sep 19, 767–783 (2020).
de Havenon, A., Ney, J. P., Callaghan, B., Yaghi, S. & Majersik, J. J. Excess neurological death in New York City after the emergence of COVID-19. J. Neurol. Epub ahead of print (2020).
Li, Y. et al. Acute cerebrovascular disease following COVID-19: a single center, retrospective, observational study. Stroke Vasc. Neurol. 5, 279–284 (2020).
Spence, J. D. et al. Mechanisms of stroke in COVID-19. Cerebrovasc. Dis. 9, 451–458 (2020).
Merkler, A. E. et al. Risk of ischemic stroke in patients with coronavirus disease 2019 (COVID-19) vs patients with influenza. JAMA Neurol. 77, 1–7 (2020).
Nordvig, A. S. et al. Potential neurological manifestations of COVID-19. Neurol. Clin. Pract. 11, e135–e146 (2020).
Author information
Authors and Affiliations
Contributions
All the authors participated in the conception, design, and acquisition of data. A.C.M. and J.D. analyzed and interpreted the data, and drafted the manuscript. All the authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Patient consent
No patient consent was required and was not obtained.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Coronado Munoz, A., Tasayco, J., Morales, W. et al. High incidence of stroke and mortality in pediatric critical care patients with COVID-19 in Peru. Pediatr Res 91, 1730–1734 (2022). https://doi.org/10.1038/s41390-021-01547-x
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-021-01547-x
This article is cited by
-
Neuroimaging findings in children with COVID-19 infection: a systematic review and meta-analysis
Scientific Reports (2024)
-
Neurological and neuroimaging implications of COVID-19 in the pediatric population.
Journal of Pediatric Neuropsychology (2024)
-
COVID-19: Transdisciplinary impact on children and adolescents.
Journal of Pediatric Neuropsychology (2024)
-
Advances in the Diagnosis and Treatment of Pediatric Arterial Ischemic Stroke
Neurotherapeutics (2023)