Abstract
Background
Extremely preterm (EPT) birth is a major risk factor for neurodevelopmental impairments. The aim was to evaluate the predictive value of Prechtl General Movement Assessment (GMA), including the Motor Optimality Score—Revised (MOS-R), at 3 months corrected age (CA) for adverse neurodevelopmental outcome at the age of 12 years.
Methods
The GMA, including the MOS-R, was applied at 3 months CA and outcomes were assessed at 12 years by Touwen’s neurological examination, the Movement Assessment Battery for Children-2, and chart reviews.
Results
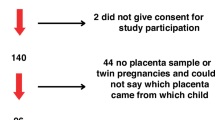
Fifty-three infants born EPT (33 boys, mean GA 25 weeks, mean body weight 805 ± 156 g) were included. Forty-two (79%) children participated in the follow-up (mean age 12.3 ± 0.4) and 62% of these had adverse outcomes. The MOS-R differed between groups (p = 0.007). The respective predictive values of GMA, aberrant FMs, and the MOS-R cut-off of 21 for adverse outcomes were positive predictive values (PPVs) of 1.00 and 0.77, negative predictive value of 0.47 and 0.63, sensitivity of 0.31 and 0.77, and specificity of 1.00 and 0.77.
Conclusions
Using the Prechtl GMA, including the MOS-R, at 3 months CA predicted an overall adverse neurodevelopment at 12 years, with a high PPV, specificity, and sensitivity in children born EPT.
Impact
-
The Prechtl GMA, including the MOS-R, can improve early identification of long-term adverse neurodevelopmental outcomes.
-
This is the first study to investigate the predictive value of the MOS-R for neurodevelopmental outcome at mid-school age in children born EPT.
-
Using the GMA, including the MOS-R, is suggested as one important part of the neurological assessment at 3 months CA in children born EPT.
-
Aberrant FMs in combination with a MOS of <21 is an indicator of an increased risk of future adverse neurodevelopment in children born EPT.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Morgan, C. et al. Effectiveness of motor interventions in infants with cerebral palsy: a systematic review. Dev. Med. Child Neurol. 58, 900–909 (2016).
Spittle, A. J., Orton, J., Anderson, P., Boyd, R. & Doyle, L. Early developmental intervention programs post hospital discharge to prevent motor and cognitive impairments in preterm infants. Cochrane Database Syst. Rev. 1, 1–56 (2015).
Bolk, J., Farooqi, A., Hafström, M., Aden, U. & Serenius, F. Developmental coordination disorder and its association with developmental comorbidities at 6.5 years in apparently healthy children born extremely preterm. JAMA Pediatr. 172, 765–774 (2018).
Broström, L., Vollmer, B., Bolk, J., Eklöf, E. & Ådén, U. Minor neurological dysfunction and associations with motor function, general cognitive abilities, and behaviour in children born extremely preterm. Dev. Med. Child Neurol. 60, 826–832 (2018).
Grunewaldt, K. H. et al. Follow-up at age 10 years in ELBW children - functional outcome, brain morphology and results from motor assessments in infancy. Early Hum. Dev. 90, 571–578 (2014).
Serenius, F. et al. Neurodevelopmental outcomes among extremely preterm infants 6.5 years after active perinatal care in Sweden. JAMA Pediatr. 170, 954–963 (2016).
Padilla, N., Alexandrou, G., Blennow, M., Lagercrantz, H. & Ådén, U. Brain growth gains and losses in extremely preterm infants at term. Cereb. Cortex 25, 1897–1905 (2015).
Einspieler, C., Prechtl, H. F. R., Bos, A. F. & Ferrarri, F. C. G. Prechtl’s Method on the Qualitative Assessment of General Movements in Preterm, Term and Young Infants (MacKeith Press; Cambridge University Press, 2004).
Einspieler, C. et al. GM Zika Working Group. Association of infants exposed to prenatal Zika virus infection with their clinical, neurologic, and developmental status evaluated via the general movement assessment tool. JAMA Netw. Open 2, e187235 (2019).
Einspieler, C. & Prechtl, H. F. R. Prechtl’s assessment of general movements: a diagnostic tool for the functional assessment of the young nervous system. Ment. Retard. Dev. Disabil. Res. Rev. 11, 61–67 (2005).
Einspieler, C. et al. Cerebral palsy: early markers of clinical phenotype and functional outcome. J. Clin. Med. 8, 1616 (2019).
Prechtl, H. F. R. et al. An early marker for neurological deficits after perinatal brain lesions. Lancet 349, 1361–1363 (1997).
Bruggink, J. L. M. et al. Quantitative aspects of the early motor repertoire in preterm infants: do they predict minor neurological dysfunction at school age? Early Hum. Dev. 85, 25–36 (2009).
Zang, F. F. et al. Very low birth weight infants in China: the predictive value of the motor repertoire at 3 to 5 months for the motor performance at 12 months. Early Hum. Dev. 100, 27–32 (2016).
Bruggink, J. L. M. et al. Early motor repertoire is related to level of self-mobility in children with cerebral palsy at school age. Dev. Med. Child Neurol. 51, 878–885 (2009).
Yang, H. et al. Cerebral palsy in children: movements and postures during early infancy, dependent on preterm vs. full term birth. Early Hum. Dev. 88, 837–843 (2012).
Bruggink, J. L. M. et al. The quality of the early motor repertoire in preterm infants predicts minor neurologic dysfunction at school age. J. Pediatr. 153, 32–39 (2008).
Salavati, S. et al. The association between the early motor repertoire and language development in term children born after normal pregnancy. Early Hum. Dev. 111, 30–35 (2017).
Bruggink, J. L. M., Van Braeckel, K. N. & Bos, A. F. The early motor repertoire of children born preterm is associated with intelligence at school age. Pediatrics 125, e1356–e1363 (2010).
Butcher, P. R. et al. The quality of preterm infants’ spontaneous movements: an early indicator of intelligence and behaviour at school age. J. Child Psychol. Psychiatry 50, 920–930 (2009).
Fjørtoft, T. et al. Assessment of motor behaviour in high-risk-infants at 3 months predicts motor and cognitive outcomes in 10 years old children. Early Hum. Dev. 89, 787–793 (2013).
Fjørtoft, T. et al. High prevalence of abnormal motor repertoire at 3 months corrected age in extremely preterm infants. Eur. J. Paediatr. Neurol. 20, 236–242 (2016).
Kwong, A. K. L. et al. Occurrence of and temporal trends in fidgety general movements in infants born extremely preterm/extremely low birthweight and term-born controls. Early Hum. Dev. 135, 11–15 (2019).
Skiöld, B., Eriksson, C., Eliasson, A. C., Ådén, U. & Vollmer, B. General movements and magnetic resonance imaging in the prediction of neuromotor outcome in children born extremely preterm. Early Hum. Dev. 89, 467–472 (2013).
Fily, A. et al. Neurological assessment at five years of age in infants born preterm. Acta Paediatr. 92, 1433–1437 (2003).
Hendersen, S. E. Movement Assessment Battery for Children - 2 2nd edn (Pearson, 2007).
Fjørtoft, T., Einspieler, C., Adde, L. & Strand, L. I. Inter-observer reliability of the “Assessment of Motor Repertoire - 3 to 5 Months” based on video recordings of infants. Early Hum. Dev. 85, 297–302 (2009).
Hadders-Algra, M. General movements: a window for early identification of children at high risk for developmental disorders. J. Pediatr. 145, 12–18 (2004).
Løhaugen, G. C. C. et al. Small for gestational age and intrauterine growth restriction decreases cognitive function in young adults. J. Pediatr. 163, 447–454 (2013).
The Express Group. One-year survival of extremely preterm infants after active perinatal care in Sweden. JAMA 301, 2225–2233 (2009).
Hafström, M. et al. Cerebral palsy in extremely preterm infants. Pediatrics 141, e20171433 (2018).
Yuge, M. et al. Movements and postures of infants aged 3 to 5 months: to what extent is their optimality related to perinatal events and to the neurological outcome? Early Hum. Dev. 87, 231–237 (2011).
Einspieler, C. et al. Highlighting the first 5 months of life: general movements in infants later diagnosed with autism spectrum disorder or Rett Syndrome. Res. Autism Spectr. Disord. 8, 286–291 (2014).
Phagava, H. et al. General movements in infants with autism spectrum disorder. Georgian Med. News 3, 100–105 (2008).
Prechtl, H. F. R., Cioni, G., Einspieler, C., Bos, A. F. & Ferrari, F. Role of vision on early motor development: lessons from the blind. Dev. Med. Child Neurol. 43, 198–201 (2001).
Groen, S. E., de Blécourt, A. C. E., Postema, K. & Hadders-Algra, M. General movements in early infancy predict neuromotor development at 9 to 12 years of age. Dev. Med. Child Neurol. 47, 731–738 (2005).
Sharp, M., Coenen, A. & Amery, N. General movement assessment and motor optimality score in extremely preterm infants. Early Hum. Dev. 124, 38–41 (2018).
Crowle, C., Galea, C., Walker, K., Novak, I. & Badawi, N. Prediction of neurodevelopment at one year of age using the general movements assessment in the neonatal surgical population. Early Hum. Dev. 118, 42–47 (2018).
Soleimani, F., Badv, R. S., Momayezi, A., Biglarian, A. & Marzban, A. General movements as a predictive tool of the neurological outcome in term born infants with hypoxic ischemic encephalopathy. Early Hum. Dev. 91, 479–482 (2015).
Spittle, A. J. et al. General movements in very preterm children and neurodevelopment at 2 and 4 years. Pediatrics 132, e452–e458 (2013).
Støen, R. et al. The Predictive accuracy of the general movement assessment for cerebral palsy: a prospective, observational study of high-risk infants in a clinical follow-up setting. J. Clin. Med. 8, 1790 (2019).
Morgan, C. et al. Sensitivity and specificity of general movements assessment for diagnostic accuracy of detecting cerebral palsy early in an Australian context. J. Paediatr. Child Health 52, 54–59 (2016).
Kwong, A. K. L., Fitzgerald, T. L., Doyle, L. W., Cheong, J. L. Y. & Spittle, A. J. Predictive validity of spontaneous early infant movement for later cerebral palsy: a systematic review. Dev. Med. Child Neurol. 60, 480–489 (2018).
van Dyk, J. et al. Prediction of long-term neurodevelopmental outcome in preterm infants using trajectories of general movement assessments. J. Perinatol. 38, 1398–1406 (2018).
Novak, I. et al. Early, accurate diagnosis and early intervention in cerebral palsy: advances in diagnosis and treatment. JAMA Pediatr. 171, 897–907 (2017).
Kwong, A. K. L. et al. The Baby Moves smartphone app for general movements assessment: engagement amongst extremely preterm and term-born infants in a state-wide geographical study. J. Paediatr. Child Health 55, 548–554 (2019).
Acknowledgements
We are grateful to all children and parents who participated in the study. We would also like to thank Christina Eriksson and Ann-Christine Eliasson as well as our research nurse Lena Swartling Schlinzig for their valuable contribution. M.Ö. was supported by Region Stockholm (clinical research appointment), Sällskapet Barnavård and the Promobilia Foundation Sweden. U.Å. was supported by grants from the Swedish Medical Research Council (grant number 2017-03043), the Stockholm County Council and the Karolinska Institutet, the Swedish Order of Freemasons in Stockholm, the Swedish Brain Foundation (grant number, FO2019-0045), and The Philipsson Foundation. The funders played no role in any aspect of the study or paper.
Author information
Authors and Affiliations
Contributions
M.Ö. and U.Å. conceptualized the study. All authors made substantial contributions of analysis and interpretation of data. M.Ö. drafted the initial manuscript, which was then critically reviewed and revised by all authors. All authors approved the final manuscript as submitted and agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
C.E. is a co-inventor of the MOS-R and member and certified tutor of the General Movements Trust. The other authors have no conflicts to declare.
Consent statement
The study was approved by The Regional Ethics Committee in Lund and Stockholm (2015/488, 2018/2547). All parents or guardians gave their written consent of participation.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Örtqvist, M., Einspieler, C. & Ådén, U. Early prediction of neurodevelopmental outcomes at 12 years in children born extremely preterm. Pediatr Res 91, 1522–1529 (2022). https://doi.org/10.1038/s41390-021-01564-w
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41390-021-01564-w
This article is cited by
-
Association between the motor optimality score-revised and clinical variables of preterm infants
BMC Pediatrics (2025)
-
Neonatal neurodevelopmental follow-up in the UK: a survey of current practice and future recommendations
BMC Pediatrics (2025)
-
Recent challenges in children’s developmental milestones
Pediatric Research (2025)
-
The implementation of EMI-Heart, a family-tailored early motor intervention in infants with complex congenital heart disease, in practice: a feasibility RCT
Pilot and Feasibility Studies (2024)
-
Motor predictors of cortical brain development and full-IQ in children born extremely preterm with and without discrete white matter abnormalities
Brain Structure and Function (2024)